Abstract
Objective
Evaluation of the impact of sequential chemoradiotherapy in high risk endometrial cancer (EC).
Methods
Two hundred fifty-four women with stage IB grade 3, II and III EC (2009 FIGO staging), were included in this retrospective study.
Results
Stage I, II, and III was 24%, 28.7%, and 47.3%, respectively. Grade 3 tumor was 53.2% and 71.3% had deep myometrial invasion. One hundred sixty-five women (65%) underwent pelvic (+/- aortic) lymphadenectomy and 58 (22.8%) had nodal metastases. Ninety-eight women (38.6%) underwent radiotherapy, 59 (23.2%) chemotherapy, 42 (16.5%) sequential chemoradiotherapy, and 55 (21.7%) were only observed. After a median follow-up of 101 months, 78 women (30.7%) relapsed and 91 women (35.8%) died. Sequential chemoradiotherapy improved survival rates in women who did not undergo nodal evaluation (disease-free survival [DFS], p=0.040; overall survival [OS], p=0.024) or pelvic (+/- aortic) lymphadenectomy (DFS, p=0.008; OS, p=0.021). Sequential chemoradiotherapy improved both DFS (p=0.015) and OS (p=0.014) in stage III, while only a trend was found for DFS (p=0.210) and OS (p=0.102) in stage I-II EC. In the multivariate analysis, only age (≤65 years) and sequential chemoradiotherapy were statistically related to the prognosis.
Endometrial cancer (EC) is the most common gynecologic malignancy in developed countries [1]. The most significant prognostic factors are tumor stage, histological grade and type, depth of myometrial invasion and lymphovascular space or nodal involvement [23456]. Observation only or vaginal radiotherapy are considered the best options in the low-risk subgroup [56]. Conversely, women with a high risk EC, as stage I grade 3 with deep myometrial invasion, stage II and III EC are at high risk of both pelvic and distant recurrences and death [7891011121314].
The optimal adjuvant therapy in high risk EC cancer is still controversial. Historically external beam radiotherapy (EBRT), with or without vaginal brachyradiotherapy (VRT), was considered the mainstay of treatment as it leads to good local control, but it does not reduce the risk of distant recurrences. Consequently due to the demonstrated chemosensitivity of EC to antiblastic agents, over the last 20 years a platinum-based chemotherapy was widely introduced in the clinical practice with the aim of improving survival [91011121314].
Two randomized trials, comparing adjuvant adriamycin-cyclophosfamide-cisplatin based chemotherapy with EBRT, were conducted in high risk EC. No differences in disease-free and overall survival (OS) were detected in either study. In contrast, the Gynecologic Oncology Group 122 (GOG 122) trial, that compared whole abdominal radiotherapy to adriamycin-cisplatin based chemotherapy in stage III-IV patients (residual abdominal tumor up to 2 cm allowed) showed an improvement in survival rates in case of chemotherapy administration [151617].
The purpose of this study is to report a single institution's retrospective analysis of the impact of adjuvant therapies in high risk endometrioid EC after primary surgical treatment and to assess the role of sequential chemoradiotherapy.
Patients with endometrioid EC stage IBG3, II or III according to the International Federation of Gynecology and Obstetrics (FIGO) 2009, treated from January 1988 to December 2011, at the Department of Obstetrics and Gynecology of San Gerardo Hospital, Monza, were considered as high risk and eligible for this analysis. All slides were analyzed by a dedicated experienced gynaecologist and pathologists. Patients with clear or serous were excluded from this study. Similarly, patients with macroscopic residual disease or synchronous ovarian cancer were excluded from this analysis [18].
All patients underwent total hysterectomy and bilateral salpingo-oophorectomy. Before 1996 systematic pelvic lymphadenectomy was performed in case of intraoperative pathological assessment of myometrial invasion more than 50% and/or G3 EC, in patients suitable for this surgical procedure according to the performance status. Between 1996 and 2006, women were randomized to pelvic (+/-) aortic lymphadenectomy vs. no lymphadenectomy or resection of bulky lymph nodes only [19]. Thereafter, we performed lymphadenectomy only in case of G3, cervical stromal invasion or positive preoperative positron emission tomography/computerized tomography (PET/CT) scan. Aortic lymphadenectomy was always performed only in case of positive pelvic lymph nodes, or positive aortic lymph nodes at preoperative CT or PET/CT scan [20].
Patients were proposed to receive observation only, chemotherapy, radiotherapy or sequential chemotherapy followed by radiotherapy and the antineoplastic agents and schedule were chosen by physicians according to the historical period, stage, performance status of patients and inclusion in randomized clinical trials [1521]. The technique for EBRT was either a three or a four-field pelvic brick or box technique with parallel opposed pair radiation fields, up to the upper limit as a plane passing the 5th lumbar vertebra. The radiation dose was delivered daily, with 1.80 Gy per fraction. VRT was administered only in case of cervical stromal invasion. Chemotherapy consisted of different platinum-based combination including, adriamycin 60 mg/m2 and cisplatin 50 mg/m2 every 3 weeks (AP), adriamycin 45 mg/m2-cyclophosfamide 650 mg/m2-cisplatin 50 mg/m2 every 3 weeks (PAC), cyclophosfamide 650 mg/m2-cisplatin 50mg/m2 every 3 weeks (CP), carboplatin area under curve (AUC) 5-paclitaxel 175 mg/m2 every 3 weeks (CT) and paclitaxel 175 mg/m2-epirubicin 80 mg/m2-cisplatin 50 mg/m2 every 3 weeks (TEP), with granulocyte-colony stimulating factor (G-CSF) administration.
In case of adjuvant sequential chemoradiotherapy, according to our protocol, chemotherapy was administered before radiotherapy, and was based on 3 cycles of AP every 3 weeks, or over the last years, 3-4 cycles of CT every 3 weeks.
After the surgical treatment and adjuvant treatments, all patients were followed with pelvic examination every 3 months during the first two years, then every 6 months. Chest-abdominal and pelvic CT scan were performed annually. The consultation of clinical data was authorized by the institutional review board of our institution.
Absolute and percentage frequencies were used to describe patients' population. Survival curves were built using the Kaplan-Meier method in which disease-free survival (DFS) was defined as the time from diagnosis to the earliest occurrence of relapse or death from any cause, while OS was defined as the time from diagnosis to death from tumor progression or death from any cause. Student t-test, Kruskal Wallis rank sum test and rank test for equality of survivor function were used to analyze the differences between treatment groups of patients. Univariate and multivariate logistic regression model were used to estimate the odds ratios and the p-values for association between outcomes (death and relapse) and clinical and histopathological parameters. Stata ver. 9.0 (Stata Co., College Station, TX, USA) was used for performing statistical analysis and a p<0.05 was deemed as statistical significance.
Two hundred fifty-four high risk EC were included in the present study. Median age was 61 years (range, 19 to 88 years). Two hundred fifteen women underwent open and 39 laparoscopic surgery.
Clinical and histopathological characteristics are reported in Table 1. The median number of pelvic lymph nodes removed was 21 (range, 14 to 46) and the median number of aortic lymph nodes removed, in case of aortic lymphadenectomy, was 12 (range, 8 to 29). Fifty-eight women had nodal metastases (40 only pelvic and 18 pelvic and aortic).
Adjuvant therapies administered in women with cancers stage I-II versus stage III were, as expected, significantly different (p<0.001). In particular, chemotherapy has been administered to 38.3% of stage III versus 9.7% of stage I-II and sequential chemo- and radiotherapy to 24.2% of stage III vs 9.7% of stage I-II cancers. Furthermore, we had a significant (p=0.017) different administration of adjuvant therapies (observation, 19.3% vs. 23.6%; radiotherapy [RT], 48.3% vs. 30.7%; chemotherapy, 21.9% vs. 24.3%; and sequential chemo-RT, 10.5% vs. 21.4%), in women treated before (n=114) or after 1999 (n=140).
All women were treated with platinum based chemotherapy: 35 women received AP, 21 CT, one CP, 28 CAP, and 16 TEP schedules. The median number of cycles was 5 (range, 2 to 8); 5 cycles (range, 3 to 8 cycles) in case of adjuvant chemotherapy only and 3 cycles (range, 2 to 6 cycles) in case of adjuvant sequential chemoradiotherapy. The median dose of EBRT was 45.0 Gy (range, 41.4 to 50.4 Gy). Ninety-two women (36.2%) underwent VRT and 16 women underwent aortic radiotherapy.
After a median follow-up of 101 months (range, 12 to 261 months), 78 women (30.7%) recurred and 91 women (35.8%) died, of which 60 for progressive disease and 31 for other reasons. Among stage I-II we had 37 recurrences (27.6%) and 52 women died (29 for tumor progression), while among stage III, 41 patients (34.2%) recurred and 39 died (31 for tumor progression). No treatments related death occurred.
Supplementary Table 1 reports the site of relapse. We had 30 pelvic failure (38.5%), 36 distant failure (46.2%), and 10 concomitant pelvic and distant relapse (12.8%) The pattern of relapse was similar among stage I-II versus stage III cancer.
Table 2 reports the number and the site of relapses according to the adjuvant treatment subgroups and stage of disease, showing that the reduction of the risk of relapse by the administration of the combined therapy occurred in both stage I-II as well in stage III (sequential chemoradiotherapy vs. no therapy, p=0.084; sequential chemoradiotherapy vs. radiotherapy, p=0.039; sequential chemoradiotherapy vs. chemotherapy, p=0.020).
Finally, we evaluate the impact of adjuvant therapies in the subgroup of women who did not undergo lymph nodes staging (n=89) or who had pelvic (+/- aortic) lymphadenectomy (n=165) (Supplementary Table 2). No significant difference was found in the two subgroups when we considered all the risk factors, apart stage (i.e., stage migration to stage IIIC in the lymphadenectomy subgroup). Women in the lymphadenectomy subgroup were more commonly treated with chemotherapy (25.5% vs. 19.1%) or sequential chemo-RT (18.8 % vs. 12.4%) compared with women in no lymphadenectomy group. Table 3 reports the 5-year survival rates according to the recourse to lymphadenectomy and the different adjuvant therapies. In the sub-analysis, adjuvant sequential chemoradiotherapy was significantly associated with better survival rates (DFS: hazard ratio [HR], 0.61 [0.38 to 0.98], p=0.040; OS: HR, 0.58 [0.36 to 0.93], p=0.024) in the no lymphadenectomy as well in the pelvic +/- aortic lymphadenectomy subgroup (DFS: HR, 0.67 [0.50 to 0.90], p=0.008; OS: HR, 0.69 [0.51 to 0.95], p=0.021).
The 5-year DFS and OS for the overall population were 69.6% and 77.9%. In particular the 5-year DFS was 72.9% in stage I-II versus 66% in stage III patients (p=0.848) and the 5-year OS was 78.5% in stage I-II versus 77.2% in stage III (p=0.514).
Table 4 reports the direct comparison between the adjuvant therapies administered, suggesting the clinical benefit on both risk of recurrence and death of sequential chemoradiotherapy compared with EBRT or chemotherapy alone.
Univariate and multivariate analysis are reported in Table 5. The only factors significantly correlated with prognosis in the multivariate analysis were age and adjuvant treatments. In particular, adjuvant sequential chemoradiotherapy was significantly associated with a better DFS (p=0.019) and OS (p=0.014). Adjuvant sequential chemoradiotherapy remained significant only in stage III for both DFS (p=0.005) and OS (p=0.014), but not in stage I-II for DFS (p=0.200) and OS (p=0.100) (Figs. 1, 2).
Our single institution's retrospective study suggests a potential benefit of sequential chemoradiotherapy as adjuvant therapy in high risk EC subgroup. The combined therapy is associated with a significantly better survival rates in stage III and a borderline improved survival in stage I-II, compared with adjuvant chemotherapy or radiotherapy alone.
Our results are in line with the pooled analysis of two randomized clinical trials (RCTs; NSGO-EC-9501/EORTC-55991 and MaNGO ILIADE-III) that compared the combination of sequential chemoradiotherapy with EBRT alone, in 534 intermediate and high risk women [21]. The NSGO/EORTC study recruited mostly stage I EC, considered qualified for adjuvant treatment for the risk profile, while the Italian group included only stage II-III EC, with no macroscopic residual disease. In the NSGO/EORTC study, after two amendments, chemotherapy could be administered either before or after radiotherapy and consisted on four courses of doxorubicin/epirubicin 50 mg/m2 plus cisplatin 50 mg/m2 every 4 weeks or paclitaxel 175 mg/m2 plus epirubicin 60 mg/m2 or doxorubicin 40 mg/m2 plus carboplatin AUC 5 or paclitaxel 175 mg/m2 plus carboplatin AUC 5-6 every 3 weeks, while in the Italian MaNGO ILIADEIII, chemotherapy was administered before radiotherapy and consisted of doxorubicin 60 mg/m2 plus cisplatin 50 mg/m2 every 3 weeks for three cycles. The pooled analysis showed that the sequential combined treatment was associated with a 36% reduction of the risk of relapse, a significantly better DFS (HR, 0.63; 95% confidence interval [CI], 0.41 to 0.99; p=0.04), cancer specific survival (HR, 0.55; 95% CI, 0.35 to 0.88; p=0.01) and a nearly significant improvement of OS (HR, 0.69; 95% CI, 0.46 to 1.03; p=0.07).
The combined concomitant and sequential chemoradiotherapy was also evaluated by the phase II RTOG 9708 study. Seventeen stage I-II and 27 stage IIIA-C patients, were treated with EBRT with concomitant triweekly cisplatin, followed by 4 cycles of adjuvant cisplatin-paclitaxel based chemotherapy with an OS and DFS of 85% and 81% at 4 years, respectively [22]. Recently, the Memorial Sloan Kettering Cancer Center (MSKCC) group reported a retrospective analysis of 40 patients (7 stage IIIA and 33 IIIC) treated with the same adjuvant multimodality protocol drawn by the RTOG, showing a very favorable 5-year DFS and OS of 79% and 85% [23].
The potential survival benefit of the multimodality treatment could be explained by the reduction of both pelvic and distant recurrences with a synergistic effect by the combination of EBRT and chemotherapy. In fact, in all the three randomized trials comparing EBRT with chemotherapy alone, almost 35%-40% of women developed local recurrences, while 60%-65% showed abdominal or distant relapses. Noteworthily, there was a small, although not significant, difference of better pelvic control of disease with EBRT and of distant control with adjuvant chemotherapy. These data suggest that despite the fact that systemic chemotherapy slightly reduces the distant failure rate, the pelvic area continue to be a significant site of recurrent disease [151617].
In our study, the overall rate of recurrence was 32.7% (32/98) in the EBRT, 37.3% (22/59) in the chemotherapy, and 16.7% (7/42) in the sequential chemoradiotherapy groups, respectively (Table 3). The reduction of the risk of relapse by the administration of the combined therapy is maintained in both stage I-II (1/13; 7.7%) as well in stage III (6/29; 20.7%) compared to both EBRT (35% and 29%, respectively) or chemotherapy groups (23% and 41%, respectively). In particular, after sequential chemoradiotherapy we had only one distant and no pelvic relapse in stage I-II disease, and two pelvic, three distant and one concomitant pelvic and distant recurrences among stage III disease.
Similar results are described in the NSGO-EC-9501/EORTC-55991 and MaNGO ILIADE-III clinical trial. An overall 16% of relapse rate was described in the chemoradiotherapy arm, of which 2% pelvic and 13% distant, compared with 26.2% in the EBRT arm (4% local and 20% distant). Furthermore, in the RTOG 9708 study no local or distant relapse was reported in stage I-II, while in stage III 8% and 30% of women had local and distant recurrences, respectively. Similarly, in the MSKCC series the authors reported a 6% of local and 25% of distant metastases in stage III disease [212223].
The preliminary results of the GOG 249 trial, that compared EBRT with chemotherapy plus VRT in 601 women with intermediate-high risk EC after radical surgery (lymphadenectomy in 90% of women), were presented at the 2014 Meeting of the Society of Gynecologic Oncology, showing no difference between EBRT and the experimental arm for both 2-year DFS (82% vs. 84%) and 2-year OS (93% vs. 92%). Chemotherapy was associated with a small reduction of distant (27 vs. 35) but with a significant increase of pelvic relapse (22 vs. 7), suggesting that a survival gain may arise only by the combination of the two adjuvant therapies.
Our study has some limitations, due to the retrospective nature, that should be discussed. First, due to the large period of this study, several different chemotherapeutic regimes were administered, although all patients had a platinum based chemotherapy, and the three most validated regimens (AP, CT, TEP) were used in 71% of women, while 28% underwent CAP regimen, currently considered as a suboptimal antiblastic treatment.
Second, we included only endometrioid histotype EC.
This decision was based on the subanalysis of GOG 122 and NSGO-EC-9501/EORTC-55991/MaNGO ILIADE-III trials. In both RCTs there was a significant impact on survival rates of chemotherapy or sequential chemoradiation compared to EBRT, only in endometrioid cancers, while no differences were found in serous/clear cells cancer. Furthermore, according to our department protocol, we had always treated serous or clear cell EC with chemotherapy and, consequently, we cannot perform a comparative analysis between the different adjuvant treatments [1721].
Third, in our series, there was no homogeneous recourse to lymphadenectomy due to the change in the surgical management of EC over the last 20 years, with a more frequent tailored lymphadenectomy in the last years, according to the result of the Italian randomized trial and the introduction of preoperative PET/CT imaging [1920]. Similarly, the choice of adjuvant therapies changed over the same period, with an increase of administration of sequential adjuvant chemoradiotherapy or chemotherapy alone compared to radiotherapy alone, in the overall population and in particular in stage III or positive lymph nodes (Supplementary Table 2). To overcome these confounding variables, we performed a sub analysis (Table 3) which showed that sequential chemoradiotherapy significantly improved the 5-year DFS and OS compared to EBRT or chemotherapy alone, irrespective of nodal staging (DFS: HR, 0.61 [0.38 to 0.98], p=0.040; OS: HR, 0.58 [0.36 to 0.93], p=0.024, in no lymphadenectomy subgroup; and DFS: HR, 0.67 [0.50 to 0.90], p=0.008; OS: HR, 0.69 [0.51 to 0.95], p=0.021, in the pelvic +/- aortic lymphadenectomy subgroup). The multivariate analysis (Table 5) definitively showed that only age and the combined adjuvant treatment were associated with prognosis, while lymphadenectomy did not.
Two randomized trials are ongoing to clarify the role of combined-versus single-modality therapy. The PORTEC-3 trial is evaluating the role of concomitant chemo and radiotherapy followed by 4 cycles of carboplatin-paclitaxel with EBRT only, while the GOG 258 trial is comparing the same experimental treatment with 6 cycles of chemotherapy for stage III or IV.
In conclusion, our retrospective analysis shows a potential benefit of the sequential chemo and radiotherapy adjuvant treatment in high risk EC, with a significant reduction of either local and distant recurrences and with an improvement of survival rates, in particular in stage III EC. Until results of the ongoing randomized trials are available, sequential chemo and radiotherapy should be strongly considered for the treatment of this subset of patients.
Figures and Tables
Fig. 1
Kaplan-Meier curves for (A) disease-free and (B) overall survival according to the adjuvant treatments. RT, radiotherapy.

Fig. 2
Kaplan-Meier curves for (A) disease-free survival and (B) overall according to the adjuvant treatments in stage I-II and in stage III endometrial cancer. RT, radiotherapy.
RT, radiotherapy.
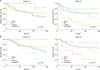
Table 1
Patient characteristics

Table 2
Number and site of relapse according to adjuvant treatment and stage of disease

Table 3
Five-year DFS and OS according to the recourse to lymphadenectomy and adjuvant therapies
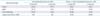
Table 4
Comparison between adjuvant therapies for the risk of recurrence and death

Table 5
Univariate and multivariate analysis of prognostic factors

References
1. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013; 63:11–30.
2. Aalders J, Abeler V, Kolstad P, Onsrud M. Postoperative external irradiation and prognostic parameters in stage I endometrial carcinoma: clinical and histopathologic study of 540 patients. Obstet Gynecol. 1980; 56:419–427.
3. Creasman WT, Morrow CP, Bundy BN, Homesley HD, Graham JE, Heller PB. Surgical pathologic spread patterns of endometrial cancer. A Gynecologic Oncology Group Study. Cancer. 1987; 60:8 Suppl. 2035–2041.
4. Guntupalli SR, Zighelboim I, Kizer NT, Zhang Q, Powell MA, Thaker PH, et al. Lymphovascular space invasion is an independent risk factor for nodal disease and poor outcomes in endometrioid endometrial cancer. Gynecol Oncol. 2012; 124:31–35.
5. Kong A, Johnson N, Kitchener HC, Lawrie TA. Adjuvant radiotherapy for stage I endometrial cancer: an updated Cochrane systematic review and meta-analysis. J Natl Cancer Inst. 2012; 104:1625–1634.
6. Nout RA, Smit VT, Putter H, Jurgenliemk-Schulz IM, Jobsen JJ, Lutgens LC, et al. Vaginal brachytherapy versus pelvic external beam radiotherapy for patients with endometrial cancer of high-intermediate risk (PORTEC-2): an open-label, non-inferiority, randomized trial. Lancet. 2010; 375:816–823.
7. Creasman WT, Kohler MF, Odicino F, Maisonneuve P, Boyle P. Prognosis of papillary serous, clear cell, and grade 3 stage I carcinoma of the endometrium. Gynecol Oncol. 2004; 95:593–596.
8. Creutzberg CL, van Putten WL, Warlam-Rodenhuis CC, van den Bergh AC, de Winter KA, Koper PC, et al. Outcome of high-risk stage IC, grade 3, compared with stage I endometrial carcinoma patients: the Postoperative Radiation Therapy in Endometrial Carcinoma Trial. J Clin Oncol. 2004; 22:1234–1241.
9. Creasman WT, Odicino F, Maisonneuve P, Quinn MA, Beller U, Benedet JL, et al. Carcinoma of the corpus uteri. FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. Int J Gynecol Obstet. 2006; 95:Suppl 1. S105–S143.
10. Long KC, Zhou Q, Hensley ML, Alektiar KM, Gomez J, Gardner GJ, et al. Patterns of recurrence in 1988 FIGO stage IC endometrioid endometrial cancer. Gynecol Oncol. 2012; 125:99–102.
11. Klopp AH, Jhingran A, Ramondetta L, Lu K, Gershenson DM, Eifel PJ. Node-positive adenocarcinoma of the endometrium: outcome and patterns of recurrence with and without external beam irradiation. Gynecol Oncol. 2009; 115:6–11.
12. Tewari KS, Filiaci VL, Spirtos NM, Mannel RS, Thigpen JT, Cibull ML, et al. Association of number of positive nodes and cervical stroma invasion with outcome of advanced endometrial cancer treated with chemotherapy or whole abdominal irradiation: a Gynecologic Oncology Group study. Gynecol Oncol. 2012; 125:87–93.
13. Hoekstra AV, Kim RJ, Small W Jr, Rademaker AW, Helenowski IB, Singh DK, et al. FIGO stage IIIC endometrial carcinoma: prognostic factors and outcomes. Gynecol Oncol. 2009; 114:273–278.
14. Bakkum-Gamez JN, Mariani A, Dowdy SC, Weaver AL, McGree ME, Martin JR, et al. Efficacy of contemporary chemotherapy in stage IIIC endometrial cancer: a histologic dichotomy. Gynecol Oncol. 2014; 132:578–584.
15. Maggi R, Lissoni A, Spina F, Melpignano M, Zola P, Favalli G, et al. Adjuvant chemotherapy vs radiotherapy in high-risk endometrial carcinoma: results of a randomised trial. Br J Cancer. 2006; 95:266–271.
16. Susumu N, Sagae S, Udagawa Y, Niwa K, Kuramoto H, Satoh S, et al. Randomized phase III trial of pelvic radiotherapy versus cisplatin-based combined chemotherapy in patients with intermediate- and high-risk endometrial cancer: a Japanese Gynecologic Oncology Group study. Gynecol Oncol. 2008; 108:226–233.
17. Randall ME, Filiaci VL, Muss H, Spirtos NM, Mannel RS, Fowler J, et al. Randomized phase III trial of whole-abdominal irradiation versus doxorubicin and cisplatin chemotherapy in advanced endometrial carcinoma: a Gynecologic Oncology Group Study. J Clin Oncol. 2006; 24:36–44.
18. Signorelli M, Fruscio R, Lissoni AA, Pirovano C, Perego P, Mangioni C. Synchronous early-stage endometrial and ovarian cancer. Int J Gynecol Obstet. 2008; 102:34–38.
19. Benedetti Panici P, Basile S, Maneschi F, Alberto Lissoni A, Signorelli M, Scambia G, et al. Systematic pelvic lymphadenectomy vs. no lymphadenectomy in early-stage endometrial carcinoma: randomized clinical trial. J Natl Cancer Inst. 2008; 100:1707–1716.
20. Crivellaro C, Signorelli M, Guerra L, De Ponti E, Pirovano C, Fruscio R, et al. Tailoring systematic lymphadenectomy in high-risk clinical early stage endometrial cancer: the role of 18F-FDG PET/CT. Gynecol Oncol. 2013; 130:306–311.
21. Hogberg T, Signorelli M, de Oliveira CF, Fossati R, Lissoni AA, Sorbe B, et al. Sequential adjuvant chemotherapy and radiotherapy in endometrial cancer: results from two randomised studies. Eur J Cancer. 2010; 46:2422–2431.
22. Greven K, Winter K, Underhill K, Fontenesci J, Cooper J, Burke T. Final analysis of RTOG 9708: adjuvant postoperative irradiation combined with cisplatin/paclitaxel chemotherapy following surgery for patients with high-risk endometrial cancer. Gynecol Oncol. 2006; 103:155–159.
23. Milgrom SA, Kollmeier MA, Abu-Rustum NR, Tew WP, Sonoda Y, Barakat RR, et al. Postoperative external beam radiation therapy and concurrent cisplatin followed by carboplatin/paclitaxel for stage III (FIGO 2009) endometrial cancer. Gynecol Oncol. 2013; 130:436–440.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download