Abstract
Objective
To analyze the cost-utility of two common clinical practices for stage IB cervical cancer patients from provider and societal viewpoints.
Methods
A decision tree model was conducted to examine value for expenditure between the following: (1) radical hysterectomy with pelvic lymph node dissection (RHPLND) with or without postoperative adjuvant therapy according to the risk of recurrence and (2) concurrent chemoradiotherapy (CCRT). The relevant studies were identified to extract the probability data, and meta-analysis was performed. Direct medical costs were estimated from hospital database and medical records review. Direct non-medical costs and utility parameters were obtained through interviews with patients to estimate quality-adjusted life years (QALYs) outcome. The time horizon was according to the life expectancy of Thai women.
Results
From provider viewpoint, RHPLND and CCRT resulted in approximate costs of US $5,281 and US $5,218, respectively. The corresponding costs from societal viewpoint were US $6,533 and US $6,335, respectively. QALYs were 16.40 years for RHPLND and 15.94 years for CCRT. The estimated incremental cost effectiveness ratio of RHPLND in comparison to CCRT from provider and societal viewpoints were US $100/QALY and US $430/QALY, respectively. RHPLND had more cost-effectiveness than CCRT if patients did not need adjuvant therapy. The most effective parameter in model was a direct medical cost of CCRT. At the current ceiling ratio in Thailand, RHPLND provides better value for money than CCRT, with a probability of 75%.
Cervical cancer is a major global health problem, especially in less-developed regions. It is the second most common cancer in Thai females, with an average age standardized incidence rate of 20.6 per 100,000 [1]. The treatment of cervical cancer is primarily based on the stage of disease. The appropriate treatment for stage IB disease has been a controversial issue [2,3,4,5]. Although this stage could be divided into stage IB1 and IB2 according to tumor size, most researchers have studied stage IB in their investigations [2,3,4,5,6,7,8,9,10]. The primary treatments for stage IB cervical cancer patients that are acknowledged as standard treatments are initiated with radical hysterectomy with pelvic lymph node dissection (RHPLND) and postoperative adjuvant therapy for individuals according to individual risk factors [6,7] or concurrent chemoradiotherapy (CCRT) [8]. No randomized controlled trial (RCT) compares these treatment modalities. The previous studies reported only disease-free survival (DFS) or overall survival (OS), whereas the quality of life and the costs of treatment have rarely been addressed.
Developed and developing countries are increasingly aware of the need for efficient use of health care resources [11], and the data on the cost-utility in each resource setting is crucial. Cervical cancer is a common cancer; however, there have been few cost effectiveness studies on this cancer [12,13,14]. Two studies, which focused their evaluation on stage IB2 cancer only, reported conflicting results [12,13]. An effect on the quality of life, which is one of the most important sequelae among toxicities, was not included in their analyses. The focus on the costs was from the third-party viewpoint. These data did not represent the actual burden on patients during or after treatment, which was shown from the societal viewpoint. Therefore, the objective of our study was to evaluate the clinical and cost outcomes in the aspect of a cost-utility analysis (CUA) of stage IB cervical cancer between RHPLND and CCRT in provider and societal viewpoints.
We conducted a decision tree model to compare the cost and utility between two primary treatment modalities for stage IB cervical cancer patients, based on their risks, as follows: RHPLND following postoperative adjuvant therapy vs. CCRT (Fig. 1). With surgery as the primary treatment, some patients had a probability of aborted RHPLND because of parametrial invasion or pelvic lymph node (LN) metastasis. The cases were confirmed by frozen section studies, and those patients received CCRT instead, as follows: 50 Gy of external beam radiotherapy (XRT) in 25 fractions with weekly cisplatin and high dose-rate intracavitary radiotherapy (ICRT). The patients who underwent RHPLND were distributed into three groups based on the risk of recurrence obtained by pathology findings [6,7]. The patients who had a positive surgical margin, positive pelvic nodes or positive parametrial tissue, which are high risk (HR) factors requiring postoperative CCRT, received the following treatment: 50 Gy of XRT in 25 fractions with weekly cisplatin±high dose-rate ICRT. The intermediate risk (IR) group, defined by having two or more factors including tumor diameter of more than 4 cm, deep stromal invasion or vascular lymphatic invasion, received postoperative 50 Gy of XRT alone. The patients without any risk factors comprised the low risk (LR) group and did not receive adjuvant treatment. The patients who started treatment with CCRT received radiation therapy composed of two dimensions of XRT with a four-field box technique at a total dose of 50 Gy in 25 fractions. Four fractions of high dose-rate ICRT were followed by weekly fractions of 6.5-7.0 Gy each to point A, depending on the tumor volume. Weekly cisplatin was given on an outpatient basis with XRT at a dosage of 40 mg/m2. In the recurrent disease group, there were three groups of patients in whom curative treatment could be achieved. These three groups were the aborted RHPLND, the LR group and the CCRT group. The salvage treatment for each group is shown in Fig. 1. Those patients did not have subsequent recurrence of disease, and had the life expectancy of Thai women. The survival time of the remaining patients who had disease relapse and received palliative treatment was 1 year [15].
The follow-up for all of the patients was based on physical examination. In the first two years, the follow-up period was every 3 months and then every 6 months during the third to fifth years. The time horizon of this study was the 76-year life expectancy of Thai women [16]. Patients who had no evidence of recurrent cancer were followed-up every year until the age of 76 years. Incremental cost effectiveness ratio (ICER) between RHPLND and CCRT was the result. The numerator was the difference in costs, whereas the denominator was the difference in the quality-adjusted life years (QALYs). The equation was as follows.
We searched for the English studies that reported RHPLND or CCRT as the primary treatment for stage IB cervical cancer. The data from RCTs were prioritized. If the essential data for analysis were not available from the RCTs, additional data from phase II or retrospective studies were used. The clinical parameters collected in our model included the probability of the patients having the following outcomes after primary surgery: aborted RHPLND, LR, IR, HR, and 5-year DFS. Meta-analysis was conducted for all of the risk proportions by the R program. The DFS of the patients who had primary surgery (with all of the outcomes) and primary CCRT were extracted from the landmark studies. The probability of "cure" by subsequent salvage treatments in the patients with recurrences was derived from the panel experts' opinions because of the inadequate data in the literature. The clinical parameters are shown in Table 1 [17,18,19,20,21,22,23].
The cost analysis in this study is from provider and societal viewpoints. Data consisted of the direct medical costs and the direct non-medical costs. All of the costs were collected from all of the stage IB cervical cancer patients who were receiving treatment or being follow-up at the Faculty of Medicine Vajira Hospital during October 2011 to September 2012. The number of patients needed for interviews about their direct non-medical costs was approximately 20 patients in each treatment arm and for each follow up visit period. Time horizon of the collected costs began at the time of the patient's visit and ended at the patient's death from cancer or until the patient was 76 years old, which is the life expectancy of Thai women. We converted all of the costs of the following years to year 2012 values using discount rate of 3% [24]. Table 2 demonstrates the cost of these parameters in US $ (the average currency exchange rate was approximately 32 Thai Baht [THB]/US $).
Direct medical costs were the costs of all diagnostic procedures and investigations. The treatment costs depended on the primary treatment modalities including surgical costs, radiation therapy costs (XRT and ICRT), chemotherapy costs (premedication and cisplatin 40 mg/m2), costs of management of all of the acute and chronic complications during and after treatment, and costs of salvage and/or palliative treatment. We adjusted all costs by multiplying 1.63 to our hospital charges [24].
Direct non-medical costs were all of the other costs including transportation expenses, food, income loss, and other costs incurred by patients or their families. All of the data were obtained from face-to-face interviews with patients.
The information of utility was acquired from the Euro-Quality of Life Five-Dimension-Thai version (EQ-5D-TH) questionnaire (registered at the EuroQol website) [25,26,27]. The health value ranged from 0 (death) to 1 (full health). The health state preferences in each time period were obtained from interviews with the patients and were converted to utility scores. The scores were multiplied by life year gained for QALYs. These results were obtained with the direct non-medical costs of the same patients (Table 3).
Because of the uncertainty of the parameters, we used one-way sensitivity and probabilistic analysis to manage and adjust the ICER when each parameter was changed or changed together. All of the costs ranged between 75% and 125%, whereas all of the probability and utility varied between the lower and upper value of the 95% confidence interval. We used the 0% to 6% discount rates of the Health Intervention and Technology Assessment Program (HITAP) of Thailand [24]. We reported all of the sensitivity analyses according to the societal viewpoint, because this viewpoint is the most interest in this study.
From October 2011 to September 2012, 100 stage IB cervical cancer patients participated in this study for all of the costs and utility; the study included 170 interviews (one patient might be interviewed more than one time because of the different follow-up times). The lifetime costs of RHPLND per patient were US $5,281 and US $6,533 from the viewpoints of the provider and society, respectively. From diagnosis to death, QALYs of the RHPLND patients were 16.40 years. For CCRT, the corresponding lifetime costs were US $5,218 from the provider viewpoints and US $6,335 from the societal viewpoints whereas the QALYs were 15.94 years. In the comparison with CCRT, the ICER gained from primary RHPLND was US $98/QALY and US $430/QALY from the provider and societal viewpoints, respectively.
When we analyzed the ICER for each risk group after RHPLND, the ICER was highest in the IR group with US $210,800/QALY gained because of the near equality of QALYs between the primary RHPLND (15.942) and CCRT (15.937). The costs, QALYs, and ICERs of the patients in each risk group after RHPLND are shown and compared with those of CCRT in Table 4.
When we estimated each parameter by variation in range as described above, the most powerful parameter was the direct medical cost of CCRT. If there were a 25% decrease in this cost, the efficiency of primary surgery decreased because of the higher cost needed to gain one QALY (US $2,295/QALY). If CCRT costs reached a peak at 125% of the baseline cost, primary surgery was preferred because the cost was lower and the QALYs were higher than with CCRT.
For the probability parameters, the probability of LR group had the most influence. The ICER increased to 178% (US $1,192/QALY) when the number of LR probability dropped to 0.34. If this proportion of probability increased to 0.45, an approximate 90% decrease of ICER (US $31/QALY) was observed. The other parameters, e.g., discount rate, other direct medical costs (except the direct medical cost of CCRT), all of the direct non-medical costs, and the utility in each treatment did not significantly influence ICER in one-way sensitivity analysis.
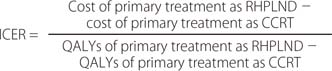
All of the parameter uncertainty analyses were conducted using Monte Carlo simulation 1,000 times, and the results are presented in Fig. 2. The line graph represents the probabilities of each treatment option that would be cost-effective in association with the ceiling ratio. At the Thai ceiling ratio of 120,000 THB/QALY or US $3,750/QALY, the probabilities of RHPLND and CCRT cost-effectiveness would be 75% and 25%, respectively.
This analytical study found that primary treatment by RHPLND had higher direct medical and non-medical costs than those of CCRT; however, RHPLND provided longer QALYs than CCRT. The ICER of primary RHPLND in comparison to CCRT was US $430/QALY. When we categorized the RHPLND patients into risk groups, only patients in the LR group had an advantage from having RHPLND as the primary treatment. The highest ICER to gain one QALY, approximately US $210,000, occurred in the IR group. The patients who could not receive a RHPLND treatment plan (aborted RHPLND) or were in the HR group after RHPLND, would have higher costs with less QALYs than the patients in the CCRT group. These results revealed that additional treatment modalities with RHPLND followed by adjuvant RT alone or adjuvant CCRT did not improve treatment outcomes. Selection of an appropriate primary treatment is crucial. Primary surgery should be offered to only the patients who have a substantial chance of being in the LR group. Other patients who are expected to be in the IR or HR group should have CCRT as a primary treatment to avoid multimodality treatment.
In the sensitivity analysis for each parameter, the most significant effect factor on ICER was the direct medical cost of CCRT. This cost consisted of XRT, ICRT, and chemotherapy (weekly cisplatin at 40 mg/m2). The highest cost among these was XRT (US $1,800); this cost had the most potential influence on our results. Radiation equipment typically has high capital and maintenance costs. Whereas this study used two-dimensions for the RT technique, this cost remained the most affected parameter. The next influencing parameter for ICER among the patients who started treatment with RHPLND was the probability of being in the LR group. This factor was related to the influence of the CCRT cost because the LR patients required no adjuvant RT or CCRT (which had a high cost). The direct medical cost of the LR patients was the cost of surgery with or without the costs of surgery complications, which was the lowest cost. An increase in the probability of the LR group was associated with an increase in the cost effectiveness of RHPLND for stage IB cervical cancer treatment. If the cost-effectiveness ceiling threshold in Thailand is 120,000 THB/QALY (US $3,750), RHPLND was the best treatment modality, which indicates a good value for the money. The probability of the cost-effectiveness of RHPLND increased to 75% in comparison with CCRT. Tools or predictive factors that could accurately determine the patient risk factors prior to surgery are important investments.
There were two studies about cost effectiveness analysis in stage IB2 cervical cancer [12,13]. These studies were conducted in the United States, and had conflicting results. The first study was by Rocconi et al. [12] in 2005. Three strategies were selected for comparison including RHPLND, CCRT and neoadjuvant chemotherapy (NCT) preceding surgery. The study found that the highest ICER for treatment of stage IB2 cervical cancer was CCRT (US $72,613 per cure), whereas the lowest ICER was RHPLND (US $41,212 per cure). Complication costs were not included in this analysis. In 2007, Jewell et al. [13] compared RHPLND and CCRT, as in our study, for stage IB2 cervical cancer treatment from a third party perspective. The study stratified patients according to the risk of recurrence after RHPLND based on the positron emission tomography/computed tomography [PET/CT] and pathological results. The costs for treatment comprised the cost of each treatment and toxicities. The ICER of RHPLND was US $63,689 per life year saved over the cost of CCRT. This study concluded that RHPLND was more expensive than CCRT in basic cases. In the patients who did not have disease in the paraaortic LN as observed on PET/CT scanning, RHPLND was a possible treatment on the basis of cost effectiveness. The authors described that the high cost of brachytherapy in the United States would significantly affect the patients who had indications for adjuvant treatment after surgery. Dissimilarities were observed in those two studies and our work. First, those studies focused particularly on stage IB2 cervical cancer. Some data in those studies were extracted from patients with all IB stages of cancer [2,3,4,6,7,17,18,19]. Several patients could not absolutely be defined as having stage IB1 (tumor size ≤4 cm) or IB2 (tumor size >4 cm) by vaginal examination; this study might well reflect the results of generalization. Second, the authors of those studies had 5-year DFS [12] and 5-year OS [13] as their final outcome, whereas our study had QALYs (obtained from utility and life year gained) as the outcome of effectiveness. In addition to the survival rate and costs, one of the most important factors that physicians should realize is the utility or quality of life of the patients after starting each treatment. From the patient perspective, utility could refer to toxicities or other consequences of different treatments. Finally, different analytical viewpoints were observed. The viewpoint of third party was the main focus in the study of Jewell et al. [13], whereas the societal viewpoint was primary in this study. We included the direct non-medical costs of patients and their families with the costs of the provider. Although the viewpoint of the analysis and model used in our study (decision tree model) and those in the study by Jewell et al. (Markov model) were different, the concept of choosing patients for surgery in the two studies was identical. RHPLND is appropriate for patients who did not have an indication for adjuvant treatment after RHPLND or who were at LR of recurrence. We selected RHPLND and CCRT as comparable model modalities because of their frequent and longstanding use in clinical practice and the many reports on their outcomes. No RCT has compared these two treatments. It is necessary to use the data concerning the 5-year DFS from different studies of each risk group following RHPLND and CCRT. There has been one RCT directly comparing RHPLND to primary RT; however, the comparison did not include CCRT [3]. Similar 5-year DFS rates were observed between primary RHPLND and RT in that study. In Table 1, the 5-year DFS of patients in the HR group in the study by Peter et al. [7] was higher than the 5-year DFS of the patients treated with CCRT in a study by Stehman et al. [8]. Because of the use of an indirect comparison, the possibility of a 5-year DFS in each risk group after RHPLND, especially in the HR group, could be overestimated, which is a limitation of this study. NCT was reported to be an alternative treatment option to RHPLND or CCRT in stage IB2 cervical cancer. The treatment outcomes, regimens of chemotherapy and indications for adjuvant treatment after RHPLND are controversial in the studies of NCT [17,20,28,29,30]; thus, NCT before surgery was not included in our analytical models. There is no optimal treatment for stage IB cervical cancer. The treatment outcomes of the three primary treatments-RHPLND, CCRT, or NCT-have not been compared in the same study. Our study was the first report to evaluate the costs and utility of treatment for stage IB cervical cancer from the provider and societal aspects. We found that RHPLND was the most efficient treatment in terms of provider and societal perspectives; however, this advantage was particularly related only to the LR group. We emphasize the importance of patient selection for primary treatment. Balancing the costs and outcome should be taken into account for all stakeholders.
Figures and Tables
Fig. 1
Decision tree model: two branches (radical hysterectomy with pelvic lymph node dissection [RHPLND] and concurrent chemoradiotherapy [CCRT]) from decision node. Aborted-CCRT, aborted RHPLND and received concurrent chemoradiotherapy; Sx_no disease, salvage treatment by surgery and no disease; I/C, indication; IR_RT, intermediate risk and received postoperative radiation therapy; HR_CCRT, high risk and received postoperative concurrent chemoradiotherapy; CCRT_no disease, salvage treatment by concurrent chemoradiotherapy and no disease; "no disease" means that there is no evidence of disease recurrence for a lifetime; "disease" means that there are evidence of disease recurrence including local recurrence or distant metastasis, which can or cannot receive salvage treatment for cure again; "disease_palliation" means that there is evidence of disease recurrence including local recurrence or distant metastasis, which cannot receive salvage treatment again. Therefore, the further treatment is palliation.

Fig. 2
Cost-effectiveness acceptability curve at willingness-to-pay (US $3,750 or 120,000 Thai Baht). CCRT, concurrent chemoradiotherapy; RHPLND, radical hysterectomy with pelvic lymph node dissection.
ACKNOWLEDGEMENTS
This work is granted by Thai Health Promotion Foundation and medical research fund of Faculty of Medicine Vajira Hospital, Navamindradhiraj University. The authors thank the Health Intervention and Technology Assessment Program (HITAP) for their scientific assistance. We also thank Prof. Jatupol Srisomboon, Assoc. Prof. Vicharn Lorvidhaya, Assoc. Prof. Prasert Lertsanguansinchai, Assoc. Prof. Chawalit Lertbutsayanukul and Assoc. Prof. Jitti Harnprasertpong for their expert comments on validation of all parameters and model.
Notes
References
1. Sriplung H, Wiangnon S, Sontipong S, Sumitsawan Y, Martin N. Cancer incidence trends in Thailand, 1989-2000. Asian Pac J Cancer Prev. 2006; 7:239–244.
2. Hopkins MP, Morley GW. Radical hysterectomy versus radiation therapy for stage IB squamous cell cancer of the cervix. Cancer. 1991; 68:272–277.
3. Landoni F, Maneo A, Colombo A, Placa F, Milani R, Perego P, et al. Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet. 1997; 350:535–540.
4. Keys HM, Bundy BN, Stehman FB, Muderspach LI, Chafe WE, Suggs CL 3rd, et al. Cisplatin, radiation, and adjuvant hysterectomy compared with radiation and adjuvant hysterectomy for bulky stage IB cervical carcinoma. N Engl J Med. 1999; 340:1154–1161.
5. Monk BJ, Wang J, Im S, Stock RJ, Peters WA 3rd, Liu PY, et al. Rethinking the use of radiation and chemotherapy after radical hysterectomy: a clinical-pathologic analysis of a Gynecologic Oncology Group/Southwest Oncology Group/Radiation Therapy Oncology Group trial. Gynecol Oncol. 2005; 96:721–728.
6. Sedlis A, Bundy BN, Rotman MZ, Lentz SS, Muderspach LI, Zaino RJ. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: A Gynecologic Oncology Group Study. Gynecol Oncol. 1999; 73:177–183.
7. Peters WA 3rd, Liu PY, Barrett RJ 2nd, Stock RJ, Monk BJ, Berek JS, et al. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000; 18:1606–1613.
8. Stehman FB, Ali S, Keys HM, Muderspach LI, Chafe WE, Gallup DG, et al. Radiation therapy with or without weekly cisplatin for bulky stage 1B cervical carcinoma: follow-up of a Gynecologic Oncology Group trial. Am J Obstet Gynecol. 2007; 197:503.e1–503.e6.
9. Chang SJ, Kim WY, Yoo SC, Yoon JH, Chun M, Chang KH, et al. A validation study of new risk grouping criteria for postoperative treatment in stage IB cervical cancers without high-risk factors: rethinking the Gynecologic Oncology Group criteria. Eur J Obstet Gynecol Reprod Biol. 2009; 147:91–96.
10. Is pelvic radiation beneficial in the postoperative management of stage Ib squamous cell carcinoma of the cervix with pelvic node metastasis treated by radical hysterectomy and pelvic lymphadenectomy? A report from the Presidential Panel at the 1979 Annual Meeting of the Society of Gynecologic Oncologists. Gynecol Oncol. 1980; 10:105–110.
11. Lyman GH, Levine M. Comparative effectiveness research in oncology: an overview. J Clin Oncol. 2012; 30:4181–4184.
12. Rocconi RP, Estes JM, Leath CA 3rd, Kilgore LC, Huh WK, Straughn JM Jr. Management strategies for stage IB2 cervical cancer: a cost-effectiveness analysis. Gynecol Oncol. 2005; 97:387–394.
13. Jewell EL, Kulasingam S, Myers ER, Alvarez Secord A, Havrilesky LJ. Primary surgery versus chemoradiation in the treatment of IB2 cervical carcinoma: a cost effectiveness analysis. Gynecol Oncol. 2007; 107:532–540.
14. Phippen NT, Leath CA 3rd, Chino JP, Jewell EL, Havrilesky LJ, Barnett JC. Cost effectiveness of concurrent gemcitabine and cisplatin with radiation followed by adjuvant gemcitabine and cisplatin in patients with stages IIB to IVA carcinoma of the cervix. Gynecol Oncol. 2012; 127:267–272.
15. Look KY, Rocereto TF. Relapse patterns in FIGO stage IB carcinoma of the cervix. Gynecol Oncol. 1990; 38:114–120.
16. Thailand life expectancy at birth [Internet]. IndexMundi;c2013. cited 2012 Sep 30. Available from: http://www.indexmundi.com/thailand/life_expectancy_at_birth.html.
17. Sardi JE, Giaroli A, Sananes C, Ferreira M, Soderini A, Bermudez A, et al. Long-term follow-up of the first randomized trial using neoadjuvant chemotherapy in stage Ib squamous carcinoma of the cervix: the final results. Gynecol Oncol. 1997; 67:61–69.
18. Whitney CW, Stehman FB. The abandoned radical hysterectomy: a Gynecologic Oncology Group Study. Gynecol Oncol. 2000; 79:350–356.
19. Leath CA 3rd, Straughn JM Jr, Estes JM, Kirby TO, Bhoola SM, Barnes MN 3rd, et al. The impact of aborted radical hysterectomy in patients with cervical carcinoma. Gynecol Oncol. 2004; 95:204–207.
20. Cai HB, Chen HZ, Yin HH. Randomized study of preoperative chemotherapy versus primary surgery for stage IB cervical cancer. J Obstet Gynaecol Res. 2006; 32:315–323.
21. Van de Putte G, Lie AK, Vach W, Baekelandt M, Kristensen GB. Risk grouping in stage IB squamous cell cervical carcinoma. Gynecol Oncol. 2005; 99:106–112.
22. Rutledge TL, Kamelle SA, Tillmanns TD, Gould NS, Wright JD, Cohn DE, et al. A comparison of stages IB1 and IB2 cervical cancers treated with radical hysterectomy. Is size the real difference? Gynecol Oncol. 2004; 95:70–76.
23. Rotman M, Sedlis A, Piedmonte MR, Bundy B, Lentz SS, Muderspach LI, et al. A phase III randomized trial of postoperative pelvic irradiation in Stage IB cervical carcinoma with poor prognostic features: follow-up of a gynecologic oncology group study. Int J Radiat Oncol Biol Phys. 2006; 65:169–176.
24. Chaikledkaew U, Teerawattananon Y, Suksomboon N. Health intervention and technology assessment program. Nonthaburi, Thailand: Graphico Systems Co.;2009.
25. Brooks R. EuroQol: the current state of play. Health Policy. 1996; 37:53–72.
26. EuroQol Group. EuroQol: a new facility for the measurement of health-related quality of life. Health Policy. 1990; 16:199–208.
27. Tongsiri S, Cairns J. Estimating population-based values for EQ-5D health states in Thailand. Value Health. 2011; 14:1142–1145.
28. Napolitano U, Imperato F, Mossa B, Framarino ML, Marziani R, Marzetti L. The role of neoadjuvant chemotherapy for squamous cell cervical cancer (Ib-IIIb): a long-term randomized trial. Eur J Gynaecol Oncol. 2003; 24:51–59.
29. Eddy GL, Bundy BN, Creasman WT, Spirtos NM, Mannel RS, Hannigan E, et al. Treatment of ("bulky") stage IB cervical cancer with or without neoadjuvant vincristine and cisplatin prior to radical hysterectomy and pelvic/para-aortic lymphadenectomy: a phase III trial of the gynecologic oncology group. Gynecol Oncol. 2007; 106:362–369.
30. Kim HS, Sardi JE, Katsumata N, Ryu HS, Nam JH, Chung HH, et al. Efficacy of neoadjuvant chemotherapy in patients with FIGO stage IB1 to IIA cervical cancer: an international collaborative meta-analysis. Eur J Surg Oncol. 2013; 39:115–124.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download