Abstract
Objective
To investigate the completeness of pedigree and of number of pedigree analysis to know the acceptable familial history in Korean women with ovarian cancer.
Methods
Interview was conducted in 50 ovarian cancer patients for obtaining familial history three times over the 6 weeks. The completeness of pedigree is estimated in terms of familial history of disease (cancer), health status (health living, disease and death), and onset age of disease and death.
Results
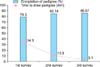
The completion of pedigree was 79.3, 85.1, and 85.6% at the 1st, 2nd, and 3rd time of interview and the time for pedigree analysis was 34.3, 10.8, and 3.1 minutes, respectively. The factors limiting pedigree analysis were as follows: out of contact with their relatives (38%), no living ancestors who know the family history (34%), dispersed family member because of the Korean War (16%), unknown cause of death (12%), reluctance to ask medical history of relatives (10%), and concealing their ovarian cancer (10%). The percentage of cancers revealed in 1st (2%) and 2nd degree (8%) relatives were increasing through surveys, especially colorectal cancer related with Lynch syndrome (4%).
The incidence of ovarian cancer, which has the highest mortality of all gynecologic cancers, continues to increase [1,2,3]. Family history is an important component of the workup process for malignant tumors such as ovarian cancer [4]. Of the solid tumors, ovarian cancer has the largest incidence due to genetic background, with the risk of BRCA1 or BRCA2 mutation at 10% to 14% in epithelial ovarian cancer [5]. Ovarian cancer has a shared etiology with breast cancer arising from BRCA1 or BRCA2 mutation and colon cancer caused by Lynch syndrome [6,7]. Family history should be evaluated in cases of suspected or diagnosed ovarian cancer [8]. Genetic tests could be indicated based on the family history [3,6].
A pedigree is a diagram illustrating family history and genetic relationships. Pedigrees have been a practical and useful tool in genetic counseling for nearly a century [9]. There are several challenges to collecting an accurate pedigree. First, it takes several minutes to complete the three generation pedigree during an interview [10,11]. Second, there is not adequate time to obtain a complete family history in routine clinical practice [12]. Third, patients usually focus on their own problems and do not consider family history significant [13]. Lastly, pedigree drawing is often hindered because of inexact information about relatives' disease status and due to interrupted contact. In our clinical experience, repeated pedigree analysis is required to address information not initially known by the patient. However, the minimum required number of interviews to complete pedigree analysis has not been clearly determined. To answer this question, we investigated the extent of pedigree completion for ovarian cancer patients extending to 2nd degree relatives.
This cross sectional study was approved by the Institutional Review Board of National Cancer Center (NCCNCS-13-832). The inclusion criterion in this study was women with pathologically diagnosed epithelial ovarian cancer treated at the National Cancer Center. Women with memory impairment or trouble with communication were excluded from this study. A total of 50 women with ovarian cancer participated in this study. Data were collected from December 2013 to February 2014.
All women participated in this study after understanding the aim of the study and signing the written informed consent form. To obtain family history, a data sheet for pedigree information was used during an interview (Supplementary data 1). This data sheet contained subjects' relation to the participant, age, health status (divided into alive and healthy living, alive with disease and dead), diagnosis of current disease, onset age of disease, and age at time of death through 2nd degree relatives. Interviews were conducted three times over 6 weeks. The follow-up period for patients' clinic visits was too diverse, ranging from 2 weeks to more than 6 months, to maintain regular intervals for face-to-face surveys only. It was not feasible in the research setting or daily clinical practice for patients to only visit the hospital for the 2nd and 3rd surveys. Therefore, the 1st survey was carried out face-to-face and the 2nd and 3rd surveys were performed by telephone. Full pedigree analysis at the 1st face-to-face visit was conducted using the data sheet with easy fill in the blanks for family history. During the 1st survey, the researcher explained that the 2nd and 3rd surveys would be conducted using a telephone interview within 3 weeks. The telephone surveys were followed by a survey to obtain values missing after the 2nd and 3rd surveys. The completeness of the pedigree is defined by familial history of disease (cancer), health status (alive and healthy, alive with disease and dead), onset age of disease and age at time of death, which are key features in screening for hereditary cancer susceptibility [14].
The demographic and clinicopathological characteristics of participants including age, age at diagnosis of ovarian cancer, tumor histology, and the International Federation of Gynecology and Obstetrics (FIGO) stage were collected. While collecting family history, we did not record identifying information, such as names, birth date, or date of death to protect privacy and confidentiality. Only the relationship of the family member to the participant, such as uncle, aunt, niece, and age or age at time of death, were depicted on the pedigree. The percentage of pedigree completion, time to collect family information, interval of each follow-up period, and related factors affecting pedigree completion were also analyzed.
The clinicopathological characteristics of participants are summarized in Table 1. Among 50 patients with epithelial ovarian cancer in this study population, mean age at time of survey was 53.3 years (range, 25 to 77 years) and mean age at diagnosis of ovarian cancer was 51.3 years (range, 24 to 76 years). Over half the participants (n=27; 54%) presented with FIGO stage III cancer. Thirty women (60%) had the serous histologic type.
The mean interval from the 1st to 2nd survey and the 2nd to 3rd survey were 12.4 days (range, 2 to 20 days) and 15.2 days (range, 7 to 20 days), respectively. The completeness of the pedigrees was 79.3%, 85.1%, and 85.6% at the 1st, 2nd, and 3rd interviews, respectively (p<0.001). The time to obtain family history ranged from 15 to 62 minutes at the 1st face-to-face survey and 2 to 40 minutes and 1 to 9 minutes at the 2nd and 3rd telephone surveys, respectively. The mean time to take family history was 34.3, 10.8, and 3.1 minutes, respectively (p<0.001) (Fig. 1).
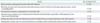
There were several factors limiting pedigree construction (Table 2). Most participants (n=19; 38%) reported that the reason it was difficult to complete the family history was being out of contact with their relatives. After the death of parents or because relatives lived in foreign countries, participants had limited opportunities to meet or contact certain relatives.
Ancestors, such as parents, aunts, uncles and grandparents, who knew the family history were either no longer alive or, if living, did not remember the family history for 16% of the participants. Dispersion of family members because of the Korean War was a barrier to completing pedigree analysis for eight participants (16%). An unknown cause of death due to limited medical facilities, especially in older relatives living in rural areas several decades ago, was a factor contributing to incomplete pedigree analysis for six participants (12%). In addition, five women (10%) felt uncomfortable asking relatives for their medical history because they felt it was impolite. Finally, five participants (10%) had not informed their relatives that they had been diagnosed with ovarian cancer.
Few family history data were corrected by participants over the 2nd and 3rd interviews. Six women (12%) discovered their exact relationship, such as aunt or uncle, to a family member. Three participants (6%) rectified incorrect information, for example, the type of cancer, death of relative, and current age.
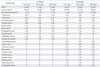
The types of cancer identified in relatives of the women with ovarian cancer are listed in Table 3. Nineteen (38%) and 28 (56%) of participants had a familial cancer history in 1st and 2nd degree relatives, respectively. These included gastrointestinal (14%), lung (8%), liver (6%), and colorectal (6%) cancer in 1st degree relatives; and gastrointestinal (20%), colorectal (8%), hematologic (6%), larynx (6%), and pancreatic (6%) cancer in 2nd degree of relatives at the time of the last survey. Between the 1st and 3rd surveys, the percentage of cancers in 1st and 2nd degree relatives increased from 2% to 8%. Two women (4%) had a family history of ovarian cancer, three women (6%) of breast cancer and seven women (14%) of colorectal cancer at the time of the last survey. The rate of breast cancer within 1st (2%) and 2nd degree relatives (4%) and ovarian cancer within 1st (2%) and 2nd degree relatives (0%) was unchanged between the 1st and 2nd surveys. In contrast, the rate of colorectal cancer within 2nd degree relatives of women with ovarian cancer increased from 10% to 14% over the three surveys.
In the current study, we found how many blank data of pedigree were completed following the three surveys. The percentage of pedigree completion increased 5.8% from the 1st survey (79.3%) to the 2nd survey (85.1%), while it increased only 0.5% from the 2nd survey (85.1%) to the 3rd survey (85.6%). This suggests that obtaining family history just once is not enough, it should be done at least twice. Furthermore, family history of patients should be continuously updated [15].
In this study, the time needed to obtain family history fell dramatically by 23.5 minutes from the 1st survey (34.3 minutes) to the 2nd survey (10.8 minutes), whereas it reduced slightly by 7.7 minutes from the 2nd survey (10.8 minutes) to the 3rd survey (3.1 minutes). Time to evaluate the family history at the 1st survey took over 30 minutes, similar to the previous study [10,11]. Family history should be routinely checked for every patient [16,17]. In the clinical environment, there is not enough time to obtain family history [18]. If the data sheet for pedigree analysis is filled by patients themselves before genetic counseling, it can make a time-consuming process easier. On the other hand, distributing copies of the pedigree could remind the patients that they need to update the family history data [19]. A computer-based program is useful to clarify and analyze family history [11].
In the current study, several factors were identified as limiting the pedigree in our study. Factors such as no living ancestors to describe the family history, family members separated due to the Korean War, and unknown cause of death due to lack of medical facilities a few decades ago may cause blanks in the family history that cannot be filled. Parents are key informers of family history [20]. On the other hand, patients might conceal or feel reluctant to ask relatives about medical history. This might change with adequate intervention. There is still a kind of taboo surrounding cancer [21], especially ovarian cancer, because it is a malignant tumor of the genital tract [22]. Absence of ancestors or parents cannot be overcome, but inappropriate recognition because of concealing cancer or absence of communication with relatives might be overcome. Education and genetic counseling can enable patients to share the information about their disease with each other [23,24].
Accuracy of family medical information depends on degree of closeness to the affected family member. Specially, medical information about second degree relatives (grandparents, aunts and uncles, nieces and nephews, grandchildren) or beyond (cousins) can be inaccurate compared with that of first degree relatives (parents, siblings, children) [25]. Furthermore, informers believe that relatives have cancer even when the results of biopsy is benign [26], and common cancer is easier to correct, whereas gender specific cancer such as ovarian cancer, cervical cancer and endometrial cancer has higher errors in medical data [27]. More detailed information in the family history helps to assess other potential candidates of hereditary cancer in their families, approach a proper preventive treatment, and suggest genetic testing [28].
The percentage of newly identified cancers in 2nd degree relatives was four times higher than that in the 1st relatives in the current study (8% vs. 2%). Participants usually know the information about their 1st degree relatives better than about 2nd degree relatives. Even if they knew that their 2nd degree relatives had cancer, they did not know the exact type of cancer. This may affect the accuracy of family history. To confirm the family history, especially cancer diagnosis, medical records are required [28]. However, medical records of relatives are confidential information and not easy to access in research-based settings or clinical environments. The accuracy of pedigree is affected by the relationship between relatives [29]. Genetic counselors need to help patients communicate and pass on information of their cancer to other family members [20]. Genetic counselors and clinicians should help patients to contact their relatives and persuade them how important it is to obtain information about their medical history and to visit hospital together.
The rate of breast and ovarian cancer, which is related with hereditary breast ovarian cancer [6], in 1st and 2nd degree relatives was not increased among the three time surveys, whereas the rate of colorectal cancer, which is involved in Lynch syndrome [30], increased by 4%. The presence of relatives with ovarian cancer and breast cancer or colorectal cancer indicates an increased likelihood of a BRCA1 or BRCA2 and MMR mutation [31,32]. In this study, 10% (5/50) of participants were considered to have hereditary breast/ovarian cancer because of familial history of ovarian or breast cancer within 2nd degree relatives. It is smaller than our previous study in Korea (16%, 54/337) [6]. However, as few patients participated in this study, there might be a selection bias. Therefore, larger prospective studies are necessary to detect the real proportion of BRCA mutations in the Korean population. Furthermore, the status of BRCA1 or BRCA2 mutations of patients who are suspected of having hereditary breast ovarian cancer is not examined yet. In a previous study, the incidences of BRCA mutations in ovarian cancer patients with family history of breast or ovarian cancer are varied: 55% in USA [33], 33% in Korea [6], 26% in Germany [34], and 12% in Pakistan [35]. Thus, genetic testing should be conducted to confirm the existence of BRCA mutations in the family history in this study. Currently, risk-reducing salpingo-oophorectomy (RRSO) has been covered by the Health Insurance Review and Assessment Service system in Korea since Dec 2012. If patients with ovarian cancer have BRCA1 or BRCA2 mutation, there are several benefits for the patients and their relatives. First, BRCA1 or BRCA2 mutation is a prognostic marker. Second, target therapy such as olaparib targeting such patients is now ongoing and very promising. Third, RRSO is the only effective way to prevent and reduce the incidence of ovarian cancer and breast cancer for the patients and their relatives. Fourth, tailored cancer prevention and screening programs might be planned according to the status of BRCA1 or BRCA2 mutation for the member of pedigrees.
There are a few limitations in the current study. First, a limited number of patients (n=50) participated. However, we believe that the increased rate of familial history of cancer and completeness, which was investigated earlier could be identified with the current study. Second, the definitive medical diagnosis has not been confirmed based on the medical records of all familial members during pedigree analysis. Currently, genetic testing for BRCA1 or BRCA2 is performed based on the familial history of breast or ovarian cancer in the family members of women with ovarian cancer [36]. Therefore, we think that completeness of family history based on daily clinical practice has been adequately evaluated.
In conclusion, analysis of pedigree twice is acceptable in Korean women with ovarian cancer from the first study in Korea. The completion of pedigree increased, while time to take family history decreasing during the three surveys. Some factors affecting the completeness of pedigree could be overcome with adequate education during genetic counseling. Interventional trials on this issue are needed in the near future.
References
1. Jung KW, Won YJ, Kong HJ, Oh CM, Seo HG, Lee JS. Cancer statistics in Korea: incidence, mortality, survival and prevalence in 2010. Cancer Res Treat. 2013; 45:1–14.
2. Chiang YC, Chen CA, Chiang CJ, Hsu TH, Lin MC, You SL, et al. Trends in incidence and survival outcome of epithelial ovarian cancer: 30-year national population-based registry in Taiwan. J Gynecol Oncol. 2013; 24:342–351.
3. Lim MC, Moon EK, Shin A, Jung KW, Won YJ, Seo SS, et al. Incidence of cervical, endometrial, and ovarian cancer in Korea, 1999-2010. J Gynecol Oncol. 2013; 24:298–302.
4. Elit L. Familial ovarian cancer. Can Fam Physician. 2001; 47:778–784.
5. Berek JS, Novak E. Berek and Novak's gynecology. 15th ed. Philadelphia: Lippincott Williams & Wilkins;2011.
6. Lim MC, Kang S, Seo SS, Kong SY, Lee BY, Lee SK, et al. BRCA1 and BRCA2 germline mutations in Korean ovarian cancer patients. J Cancer Res Clin Oncol. 2009; 135:1593–1599.
7. Lim MC, Seo SS, Kang S, Seong MW, Lee BY, Park SY. Hereditary non-polyposis colorectal cancer/Lynch syndrome in Korean patients with endometrial cancer. Jpn J Clin Oncol. 2010; 40:1121–1127.
8. Morgan RJ Jr, Alvarez RD, Armstrong DK, Burger RA, Castells M, Chen LM, et al. Ovarian cancer, version 3.2012. J Natl Compr Canc Netw. 2012; 10:1339–1349.
9. Resta RG. The crane's foot: The rise of the pedigree in human genetics. J Genet Couns. 1993; 2:235–260.
10. Rogers J, Durkin M. The semi-structured genogram interview. I: Protocol. II: Evaluation. Fam Syst Med. 1984; 2:176–187.
11. Waters I, Watson W, Wetzel W. Genograms. Practical tools for family physicians. Can Fam Physician. 1994; 40:282–287.
12. Acheson LS, Wiesner GL, Zyzanski SJ, Goodwin MA, Stange KC. Family history-taking in community family practice: implications for genetic screening. Genet Med. 2000; 2:180–185.
13. Wattendorf DJ, Hadley DW. Family history: the three-generation pedigree. Am Fam Physician. 2005; 72:441–448.
14. Bennett RL. The practical guide to the genetic family history. 2nd ed. Hoboken: Wiley-Blackwell;2011.
15. Hunt SC, Williams RR, Barlow GK. A comparison of positive family history definitions for defining risk of future disease. J Chronic Dis. 1986; 39:809–821.
16. Ramsey PG, Curtis JR, Paauw DS, Carline JD, Wenrich MD. History-taking and preventive medicine skills among primary care physicians: an assessment using standardized patients. Am J Med. 1998; 104:152–158.
17. Acton RT, Burst NM, Casebeer L, Ferguson SM, Greene P, Laird BL, et al. Knowledge, attitudes, and behaviors of Alabama's primary care physicians regarding cancer genetics. Acad Med. 2000; 75:850–852.
18. Rich EC, Burke W, Heaton CJ, Haga S, Pinsky L, Short MP, et al. Reconsidering the family history in primary care. J Gen Intern Med. 2004; 19:273–280.
19. Guttmacher AE, Collins FS, Carmona RH. The family history: more important than ever. N Engl J Med. 2004; 351:2333–2336.
20. Green J, Richards M, Murton F, Statham H, Hallowell N. Family communication and genetic counseling: the case of hereditary breast and ovarian cancer. J Genet Couns. 1997; 6:45–60.
21. Balshem M. Cancer, control, and causality: talking about cancer in a working-class community. Am Ethnol. 1991; 18:152–172.
22. Wenzel LB, Donnelly JP, Fowler JM, Habbal R, Taylor TH, Aziz N, et al. Resilience, reflection, and residual stress in ovarian cancer survivorship: a gynecologic oncology group study. Psychooncology. 2002; 11:142–153.
23. Lerman C, Biesecker B, Benkendorf JL, Kerner J, Gomez-Caminero A, Hughes C, et al. Controlled trial of pretest education approaches to enhance informed decision-making for BRCA1 gene testing. J Natl Cancer Inst. 1997; 89:148–157.
24. Bernhardt BA, Biesecker BB, Mastromarino CL. Goals, benefits, and outcomes of genetic counseling: client and genetic counselor assessment. Am J Med Genet. 2000; 94:189–197.
25. Schneider KA, DiGianni LM, Patenaude AF, Klar N, Stopfer JE, Calzone KA, et al. Accuracy of cancer family histories: comparison of two breast cancer syndromes. Genet Test. 2004; 8:222–228.
26. King TM, Tong L, Pack RJ, Spencer C, Amos CI. Accuracy of family history of cancer as reported by men with prostate cancer. Urology. 2002; 59:546–550.
27. Douglas FS, O'Dair LC, Robinson M, Evans DG, Lynch SA. The accuracy of diagnoses as reported in families with cancer: a retrospective study. J Med Genet. 1999; 36:309–312.
28. Trepanier A, Ahrens M, McKinnon W, Peters J, Stopfer J, Grumet SC, et al. Genetic cancer risk assessment and counseling: recommendations of the national society of genetic counselors. J Genet Couns. 2004; 13:83–114.
29. Sijmons RH, Boonstra AE, Reefhuis J, Hordijk-Hos JM, de Walle HE, Oosterwijk JC, et al. Accuracy of family history of cancer: clinical genetic implications. Eur J Hum Genet. 2000; 8:181–186.
30. Watson P, Butzow R, Lynch HT, Mecklin JP, Jarvinen HJ, Vasen HF, et al. The clinical features of ovarian cancer in hereditary nonpolyposis colorectal cancer. Gynecol Oncol. 2001; 82:223–228.
31. Frank TS, Manley SA, Olopade OI, Cummings S, Garber JE, Bernhardt B, et al. Sequence analysis of BRCA1 and BRCA2: correlation of mutations with family history and ovarian cancer risk. J Clin Oncol. 1998; 16:2417–2425.
32. Vasen HF, Watson P, Mecklin JP, Lynch HT. New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the International Collaborative group on HNPCC. Gastroenterology. 1999; 116:1453–1456.
33. Martin AM, Blackwood MA, Antin-Ozerkis D, Shih HA, Calzone K, Colligon TA, et al. Germline mutations in BRCA1 and BRCA2 in breast-ovarian families from a breast cancer risk evaluation clinic. J Clin Oncol. 2001; 19:2247–2253.
34. Meindl A. German Consortium for Hereditary Breast and Ovarian Cancer. Comprehensive analysis of 989 patients with breast or ovarian cancer provides BRCA1 and BRCA2 mutation profiles and frequencies for the German population. Int J Cancer. 2002; 97:472–480.
35. Rashid MU, Zaidi A, Torres D, Sultan F, Benner A, Naqvi B, et al. Prevalence of BRCA1 and BRCA2 mutations in Pakistani breast and ovarian cancer patients. Int J Cancer. 2006; 119:2832–2839.
36. Barcenas CH, Hosain GM, Arun B, Zong J, Zhou X, Chen J, et al. Assessing BRCA carrier probabilities in extended families. J Clin Oncol. 2006; 24:354–360.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download