Abstract
Objective
The surgical staging system for endometrial carcinoma developed by International Federation of Gynecology and Obstetrics (FIGO) in 1988 was revised in 2009. Given the importance of continuous validation of the prognostic performance of staging systems, we analyzed the disease specific survival for patients with endometrial carcinoma using FIGO 1988 and 2009 systems. Further, the stage distribution of endometrioid and nonendometrioid carcinomas was studied.
Methods
Eight hundred twenty-one women with endometrial carcinoma were retrospectively staged using FIGO 1988 and 2009 systems.
Results
FIGO 1988 IC was associated with an inferior survival compared with IA-IB. Survival overlapped for 1988 IA and IB, for 1988 IC and IIA, and for 2009 IB and II. FIGO 2009 IA-II patients with negative peritoneal cytology had a superior survival compared with 1988 IIIA patients with positive cytology only. The survival was similar for 1988 IIIA with positive cytology only and for 2009 IIIA. Cox proportional hazards model recognized grade 3 endometrioid and nonendometrioid histology, tumor spread beyond the uterine corpus and cervix, and positive peritoneal cytology as significant predictors of death. Among 2009 IIIC substages, the proportion of IIIC2 tumors was higher for nonendometrioid than for endometrioid carcinomas (p=0.003).
Conclusion
Stage I with deep myometrial invasion and stage II endometrial carcinoma seem to have similar survival outcomes. Although positive peritoneal cytology does not alter the stage according to the FIGO 2009 system, it should be considered a poor prognostic sign. The high proportion of nonendometrioid carcinomas in the stage IIIC2 category may reflect different patterns of retroperitoneal spread among tumors with different histologic subtypes.
Endometrial carcinoma is the most common female genital tract malignancy in the Western world [1] and in Finland the third most common female cancer after breast and colon cancer [2]. Generally the prognosis of endometrial carcinoma is good with an overall survival of around 80% [3]. Poor prognostic signs include old age, advanced-stage disease, high tumor grade, and nonendometrioid histology [3]. Of these, tumor stage, i.e. the extent of the disease at the time of presentation, is the most powerful prognostic parameter. Thus, staging provides an important tool for outcome comparisons, and facilitates recommendations for adjuvant therapy [4].
The International Federation of Gynecology and Obstetrics (FIGO) developed its classification and staging system for endometrial carcinoma and other female genital cancers in 1958 [5]. The staging of endometrial carcinoma was altered from clinical to surgicopathologic in 1988 [6]. A revised version was introduced in 2009, with a rationale to further improve the prognostic performance of surgical staging [7]. Main changes for the FIGO 2009 system include: (1) noninvasive tumors (1988 IA) and tumors with <50% myometrial invasion (1988 IB) are combined (2009 IA); (2) cervical glandular involvement does not affect staging (1988 IIA shifted to 2009 IA-IB); (3) peritoneal cytology does not affect staging (1988 IIIA with positive cytology only shifted to 2009 IA-II); (4) tumors with lymph node metastasis (1988 IIIC) are subdivided to stages IIIC1 (indicating positive pelvic nodes) and IIIC2 (indicating positive para-aortic nodes with or without positive pelvic nodes).
With the recognition that the validity of the FIGO 2009 staging system for endometrial carcinoma needs continuous monitoring for possible refinements, we compared FIGO 1988 and 2009 staging systems in two respects. First, we studied the stage-by-stage disease specific survivals using both staging systems. Second, we examined the stage distribution of endometrioid and nonendometrioid subtype carcinomas.
Women with endometrial carcinoma treated surgically between January 2008 and December 2012 at the Department of Obstetrics and Gynecology, Helsinki University Central Hospital, were included in the study (n=821). Clinicopathologic data, including age at surgery, body mass index, tumor histology, and tumor grade were collected. The median follow-up time was 29 months (range, 1 to 64 months). Pelvic lymph node dissection was performed for patients with grade 1-2 endometrioid carcinomas; however, as of January 2012, lymphadenectomy was omitted in tumors with <50% myometrial invasion according to magnetic resonance imaging. Pelvic and para-aortic lymphadenectomy was performed in deeply invasive grade 1-2 endometrioid carcinomas, grade 3 endometrioid carcinomas, and nonendometrioid carcinomas. There was some variance in practice patterns because the decision to perform lymphadenectomy and the extent of the procedure depended on patient age and comorbidities. Tumors were staged according to FIGO 1988 [6] and FIGO 2009 [7] criteria. Hematoxylin and eosin-stained slides of the primary tumors were reviewed by a gynecologic pathologist (RB) for confirmation of the original diagnosis of endometrial adenocarcinoma and determination of the histologic subtype and grade of the tumors. Patient characteristics and surgical data are shown in Table 1. Institutional Review Board approval was obtained for the study.
Survival was determined as the number of months from surgery to date of death. Disease specific survival was evaluated using Kaplan-Meier curves. A Cox proportional hazards model was used to assess the importance of individual covariates in survival times. Pearson χ2 analysis was used to compare the incidence of different histological subtypes in various tumor stages. A p<0.05 was considered statistically significant.
FIGO 1988 stage IA and IB patients showed similar disease specific survival (p=0.182), whereas 1988 IC was associated with inferior survival compared with 1988 IA-IB (Fig. 1). Survival for patients with 1988 IC and IIA was not significantly different (Fig. 2). Moreover, survival overlapped for 2009 IB and II (Fig. 3).
FIGO 2009 stage IA-II patients with negative peritoneal cytology had superior survival compared with 1988 IIIA patients with positive cytology only (Fig. 4). The survival overlapped for patients with 1988 IIIA with positive cytology only and patients with 2009 IIIA (p=0.301). The disease specific survival for 2009 IIIC1 and IIIC2 was 48±4 months and 39±6 months, respectively (mean±SD). This difference was of a borderline significance (p=0.132).
Multivariate analysis using Cox proportional hazards model was conducted to evaluate the effect of histologic subtype, stage, and finding of pelvic washing cytology on disease specific survival (Table 2). We found that grade 3 endometrioid and nonendometrioid histology, tumor spread beyond the uterine corpus and cervix, and positive cytology were significant predictors of death.
Twenty-nine patients (3.5%) were down-staged with the elimination of stages IIA and IIIA with positive peritoneal cytology only from the FIGO 2009 staging system. The proportion of endometrioid and nonendometrioid carcinomas in the eliminated stages was similar (Table 3). Further, the proportion of endometrioid and nonendometrioid carcinomas in FIGO 1988 stage IA was not significantly different (Table 3). The study population included 50 stage IIIC endometrioid carcinomas and 14 IIIC nonendometrioid carcinomas. Among them, the proportion of stage IIIC2 tumors was higher for nonendometrioid (71.4%) than for endometrioid carcinomas (28.0%; p=0.003) (Table 3). The difference persisted after excluding patients with IIIC1 tumors who did not receive para-aortic lymphadenectomy (proportion of IIIC2 tumors 100% and 58.3% for nonendometrioid and endometrioid carcinomas, respectively; p=0.015).
Several comparative studies on the prognostic performance of FIGO 1988 and 2009 endometrial carcinoma staging systems have been published. Two studies from the United States included only endometrioid carcinomas in the analysis, and due to being register-based, could not restage 1988 IIA tumors and IIIA tumors with positive peritoneal cytology only [8,9]. A European multicenter study recruited patients with endometrioid and nonendometrioid carcinomas to analyze the disease specific survival using FIGO 1988 and 2009 systems [10]. The cause specific survival of patients with nonendometrioid carcinomas was assessed in a register-based study from the United States [11], and a study from Korea compared the overall survival of nonendometrioid carcinomas with that of grade 3 endometrioid carcinomas [12]. Lastly, overall survivals according to the two staging systems were compared in two single institution studies [13,14], one of which sought to describe survival differences for various substages of stage I endometrioid carcinomas [13]. The results of these earlier studies have been somewhat inconclusive, especially regarding the outcome of stage I and II carcinomas, with or without positive peritoneal cytology.
Here, we analyzed the disease specific survival and stage distribution of endometrioid and nonendometrioid subtype carcinomas in 821 patients treated at our institution, using both FIGO 1988 and 2009 systems as a reference. The varying indications of radiotherapy and chemotherapy as adjuvant treatments for endometrial carcinoma emphasize the importance of standardized treatment protocols in prognostic studies. We trust that our study design, i.e., a single institution study on a large sample with a relatively high lymphadenectomy rate (68.0%), allows for a collection of reliable data on the outcome of women with endometrial carcinoma.
A number of reports have failed to show an association between positive peritoneal cytology and survival or recurrence in patients with early stage endometrial carcinoma [15-17]. Further, it has been suggested that positive peritoneal cytology potentiates the effect of other poor prognostic factors rather than serves as an independent predictor of outcome [18,19]. Consequently, pelvic washings were dropped from FIGO 2009 staging criteria for endometrial carcinoma, but may still be reported separately. Importantly, we found that positive peritoneal cytology had a negative impact on survival (survival rates 63.6% and 96.1% for FIGO 2009 IA-II tumors with and without positive peritoneal cytology, respectively, during the median follow-up time of 29 months). By contrast, Kato et al. [14] found similar overall survivals for FIGO 1988 stage IIIA with positive peritoneal cytology only and for FIGO 2009 stage I. Nevertheless, we were able to confirm the survival benefit for negative cytology by a Cox proportional hazards model that accounted histologic subtype and stage as additional covariates. Our data suggest that peritoneal cytology should be considered for an accurate risk stratification of patients with endometrial carcinoma. This conclusion is also supported by a population-based study in which positive cytology was found to be an independent predictor of survival after adjusting for other contributory factors [20].
We found similar outcomes for patients with FIGO 1988 stage IA and IB carcinomas, thus supporting their combination in a single stage in the FIGO 2009 system. This renewal in the staging system is supported by other studies [8,9,11,14]. Abu-Rustum et al. [13] found a survival difference for 1988 stage IA and IB endometrioid carcinomas, but instead of disease specific survival they had overall survival as their end-point. This may have affected the results, considering the multiple comorbidities that are common in patients with endometrial carcinoma.
Stage IIA (cervical glandular involvement) was eliminated from FIGO 2009 staging criteria; these patients are now down-staged to stages IA-IB. This revision is supported by our finding of similar outcomes for FIGO 1988 stages IC and IIA, and by Werner et al. [10] who found overlapping disease specific survivals for patients with 1988 stage IIA and 2009 stage IA-B carcinomas.
Lewin et al. [8] found inferior survival for FIGO 2009 stage II compared with stage IB, a finding that could not be confirmed in the present study, possibly because of the above-mentioned differences in study designs. In another study, the reproducibility of identification of cervical gland and endocervical stromal involvement was only slight to fair among pathologists [21]. Moreover, similar to our finding of equal outcomes for FIGO 2009 stages IB and II, the recurrence-free survival of patients with any type of cervical involvement was not significantly different from stage I controls [21]. Altogether, these data indicate that cervical spread may not be a useful prognostic indicator.
We observed a difference in the distribution of endometrioid and nonendometrioid carcinomas among FIGO 2009 IIIC substages so that less than one third of endometrioid and more than two thirds of nonendometrioid carcinomas with lymphatic spread belonged to stage IIIC2. It is unlikely that the difference can be explained by a higher rate of para-aortic lymphadenectomy in patients with nonendometrioid carcinomas because the finding persisted after exclusion of patients with IIIC1 tumors in whom para-aortic lymphadenectomy was not performed. Although we cannot exclude the possibility of a longer diagnostic delay in patients with nonendometrioid carcinomas, it could be hypothesized that a true difference in the pattern of retroperitoneal spread exists between tumors with different histological subtypes. This fits in with the notion that the outcome of patients with serous and clear cell carcinomas is significantly worse than that of patients with grade 3 endometrioid carcinomas [12,22].
In summary, we have described the disease specific survival for patients with endometrial carcinoma using two FIGO staging systems in a large population from a single institution. Patients with stage I tumor with deep myometrial invasion and stage II tumor seem to have similar outcomes. Thus, a reliable risk stratification of these patients may require other than anatomical staging systems, perhaps such that take notice of the presence of lymphovascular space invasion [23] or expression of certain growth-promoting factors [24]. Although positive peritoneal cytology does not affect endometrial carcinoma staging according to the FIGO 2009 system, it should be considered a poor prognostic sign. The high proportion of nonendometrioid carcinomas in the stage IIIC2 category may reflect different patterns of retroperitoneal spread among tumors with different histologic subtypes.
Figures and Tables
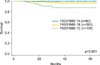 | Fig. 1Disease specific survival for patients with International Federation of Gynecology and Obstetrics (FIGO) 1988 stages IA-IC (+, censored data). |
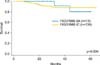 | Fig. 2Disease specific survival for patients with International Federation of Gynecology and Obstetrics (FIGO) 1988 stages IC and IIA (+, censored data). |
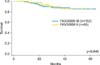 | Fig. 3Disease specific survival for patients with International Federation of Gynecology and Obstetrics (FIGO) 2009 stages IB and II (+, censored data). |
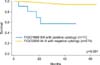 | Fig. 4Disease specific survival for patients with International Federation of Gynecology and Obstetrics (FIGO) 2009 stages IA-II with negative peritoneal cytology and FIGO 1988 stage IIIA with positive cytology only (+, censored data). |
References
1. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012; 62:10–29.
2. Institute for Statistical and Epidemiological Cancer Research. Finnish Cancer Registry: statistics [Internet]. Institute for Statistical and Epidemiological Cancer Research;cited 2013 Nov 20. Available from: http://www.cancerregistry.fi.
3. Sorosky JI. Endometrial cancer. Obstet Gynecol. 2012; 120(2 Pt 1):383–397.
4. Prat J. Prognostic parameters of endometrial carcinoma. Hum Pathol. 2004; 35:649–662.
5. Odicino F, Pecorelli S, Zigliani L, Creasman WT. History of the FIGO cancer staging system. Int J Gynaecol Obstet. 2008; 101:205–210.
6. Shepherd JH. Revised FIGO staging for gynaecological cancer. Br J Obstet Gynaecol. 1989; 96:889–892.
7. Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. 2009; 105:103–104.
8. Lewin SN, Herzog TJ, Barrena Medel NI, Deutsch I, Burke WM, Sun X, et al. Comparative performance of the 2009 international Federation of gynecology and obstetrics' staging system for uterine corpus cancer. Obstet Gynecol. 2010; 116:1141–1149.
9. Cooke EW, Pappas L, Gaffney DK. Does the revised International Federation of Gynecology and Obstetrics staging system for endometrial cancer lead to increased discrimination in patient outcomes? Cancer. 2011; 117:4231–4237.
10. Werner HM, Trovik J, Marcickiewicz J, Tingulstad S, Staff AC, Amant F, et al. Revision of FIGO surgical staging in 2009 for endometrial cancer validates to improve risk stratification. Gynecol Oncol. 2012; 125:103–108.
11. Page BR, Pappas L, Cooke EW, Gaffney DK. Does the FIGO 2009 endometrial cancer staging system more accurately correlate with clinical outcome in different histologies? Revised staging, endometrial cancer, histology. Int J Gynecol Cancer. 2012; 22:593–598.
12. Kim HJ, Kim TJ, Lee YY, Choi CH, Lee JW, Bae DS, et al. A comparison of uterine papillary serous, clear cell carcinomas, and grade 3 endometrioid corpus cancers using 2009 FIGO staging system. J Gynecol Oncol. 2013; 24:120–127.
13. Abu-Rustum NR, Zhou Q, Iasonos A, Alektiar KM, Leitao MM Jr, Chi DS, et al. The revised 2009 FIGO staging system for endometrial cancer: should the 1988 FIGO stages IA and IB be altered? Int J Gynecol Cancer. 2011; 21:511–516.
14. Kato T, Watari H, Endo D, Mitamura T, Odagiri T, Konno Y, et al. New revised FIGO 2008 staging system for endometrial cancer produces better discrimination in survival compared with the 1988 staging system. J Surg Oncol. 2012; 106:938–941.
15. Kasamatsu T, Onda T, Katsumata N, Sawada M, Yamada T, Tsunematsu R, et al. Prognostic significance of positive peritoneal cytology in endometrial carcinoma confined to the uterus. Br J Cancer. 2003; 88:245–250.
16. Tebeu PM, Popowski GY, Verkooijen HM, Casals J, Ludicke F, Zeciri G, et al. Impact of peritoneal cytology on survival of endometrial cancer patients treated with surgery and radiotherapy. Br J Cancer. 2003; 89:2023–2026.
17. Fadare O, Mariappan MR, Hileeto D, Wang S, McAlpine JN, Rimm DL. Upstaging based solely on positive peritoneal washing does not affect outcome in endometrial cancer. Mod Pathol. 2005; 18:673–680.
18. Takeshima N, Nishida H, Tabata T, Hirai Y, Hasumi K. Positive peritoneal cytology in endometrial cancer: enhancement of other prognostic indicators. Gynecol Oncol. 2001; 82:470–473.
19. Mariani A, Webb MJ, Keeney GL, Aletti G, Podratz KC. Assessment of prognostic factors in stage IIIA endometrial cancer. Gynecol Oncol. 2002; 86:38–44.
20. Garg G, Gao F, Wright JD, Hagemann AR, Mutch DG, Powell MA. Positive peritoneal cytology is an independent risk-factor in early stage endometrial cancer. Gynecol Oncol. 2013; 128:77–82.
21. Zaino RJ, Abendroth C, Yemelyanova A, Oliva E, Lim D, Soslow R, et al. Endocervical involvement in endometrial adenocarcinoma is not prognostically significant and the pathologic assessment of the pattern of involvement is not reproducible. Gynecol Oncol. 2013; 128:83–87.
22. Hamilton CA, Cheung MK, Osann K, Chen L, Teng NN, Longacre TA, et al. Uterine papillary serous and clear cell carcinomas predict for poorer survival compared to grade 3 endometrioid corpus cancers. Br J Cancer. 2006; 94:642–646.
23. Guntupalli SR, Zighelboim I, Kizer NT, Zhang Q, Powell MA, Thaker PH, et al. Lymphovascular space invasion is an independent risk factor for nodal disease and poor outcomes in endometrioid endometrial cancer. Gynecol Oncol. 2012; 124:31–35.
24. Salvesen HB, Haldorsen IS, Trovik J. Markers for individualised therapy in endometrial carcinoma. Lancet Oncol. 2012; 13:e353–e361.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download