Abstract
Methods
For three Asian countries and one region (Japan, Korea, Singapore, and Hong Kong), we extracted number of deaths for each year from the World Health Organization (WHO) mortality database, focusing on women ≥20 years old. The WHO population data were used to estimate person-years at risk for women. The annual age-standardized, truncated rates were evaluated for four age groups. We also compared age-specific mortality rates during three calendar periods (1979 to 1988, 1989 to 1998, and 1999 to 2010). Joinpoint regression was used to determine secular trends in mortality. To obtain cervical and uterine corpus cancer mortality rates in Korea, we re-allocated the cases with uterine cancer of unspecified subsite according to the proportion in the National Cancer Incidence Databases.
Results
Overall, uterine cancer mortality has decreased in each of the Asian regions. In Korea, corrected cervical cancer mortality has declined since 1993, at an annual percentage change (APC) of -4.8% (95% confidence interval [CI], -5.3 to -4.4). On the other hand, corrected uterine corpus cancer mortality has abruptly increased since 1995 (APC, 6.7; 95% CI, 5.4 to 8.0). Ovarian cancer mortality was stable, except in Korea, where mortality rates steadily increased at an APC of 6.2% (95% CI, 3.4 to 9.0) during 1995 to 2000, and subsequently stabilized.
Uterine and ovarian cancers are responsible for 10% and 2% of all cancer deaths worldwide, respectively, causing an estimated 489,000 deaths annually. Indeed, cancers of the cervix and ovary are respectively the fifth and seventh most common causes of death from cancer in Asia [1]. It has been estimated that the number of deaths due to uterine and ovarian cancer will reach approximately 347,100 by 2020 in Asia alone [1].
Mortality from cancers of the uterus and ovaries has been declining in Western countries for decades [2,3,4,5]. The incidence and mortality rates of gynecologic cancers in Asian countries differ from those in Western countries. Cervical cancer remains a major health problem in East Asia, although incidence rates have been decreasing [6,7]. In recent decades, East Asia has experienced rapid economic growth and social transformation. These socioeconomic changes have resulted in improved treatments and advances in screening. In particular, cervical cancer screening programs were introduced as early as the 1980s, and routine gynecologic examination has become popular in East Asian countries. In addition, behavioral factors such as delayed and reduced childbearing, use of hormone-replacement therapy, and reduced physical activity have also become more prevalent among East Asian women. These reproductive and lifestyle changes are associated with higher incidences of uterine corpus and ovarian cancer [8,9]. However, there are few studies on temporal trend in gynecologic cancer mortality in East Asian regions.
Specific trends in gynecologic cancer mortality differ widely by geographic region, age group, and time period. The aim of this study was to report and compare secular trends of uterine and ovarian cancer in Hong Kong, Japan, Korea, and Singapore. We designed our study to fully investigate the different cancer trends that are present in different regions, age groups, and time periods. In addition, we used national cancer incidence data from Korea to correct cervical and uterine corpus cancer mortality rates, which are otherwise substantially biased by missing cancer subsite information in mortality databases.
The World Health Organization (WHO) obtains data on deaths by age, sex, and cause of death, as reported annually by member states based on their civil registration systems. WHO compiles these data in the WHO mortality database. The 4 East Asian regions with data available for longest period were Japan, Singapore, Korea, and Hong Kong. The coverage of cause of death in the registration systems had increased over 85% since 1990. We extracted annual uterine cancer mortality data for women aged ≥20 years in Hong Kong (1966 to 2009), Japan (1955 to 2010), Korea (1985 to 2010), and Singapore (1966 to 2009) from the WHO mortality database [10]. Ovarian cancer mortality data were also extracted from the same database for Hong Kong (2001 to 2009), Japan (1979 to 2010), Korea (1985 to 2010), and Singapore (1979 to 2009). To obtain estimates of person-years at risk, we used WHO population data [10].
Uterine cancer mortality was defined as deaths in the WHO mortality database that were coded as C53 (uterine cervical cancer), C54 (uterine corpus cancer), or C55 (unspecified uterine cancer), according to the International Statistical Classification of Disease and Related Health Problems, 10th revision (ICD-10) [11]. Assessment of ovarian cancer mortality was based on the ICD-10 code C56. Uterine cervical cancer and uterine corpus cancer have different etiologies and prognoses, and the ICD-10 code C55 (which is, "uterus, unspecified site") makes it difficult to determine the exact cervical and uterine corpus cancer mortality trends [12,13,14,15]. To solve this problem, we corrected the number of cervical cancer and uterine corpus cancer deaths using death certificate data during 1993 to 2010 from the Statistics Korea and data on cases of unspecified uterine cancer from the National Cancer Incidence Databases (NCIDB) of Korea [16]. To obtain a corrected count of cervical cancer deaths, we multiplied the total number of registered unspecified uterine cancer deaths (ICD-10: C55) by the proportion of registered, incident uterine cancer cases that were specifically coded as cervical cancer (ICD-10: C53). We then added the result to the deaths known to cause cervical cancer, thereby achieving at a corrected total of cervical cancer deaths. Analogous methods were applied to obtain a corrected estimate of uterine corpus deaths. The details of this correction procedure have been described in a previous report [17]. As the personal identification number used for data was deleted, this study did not require the ethical approval of the Institutional Review Board.
Annual age-standardized mortality rates were estimated using the world standard population [18]. Rates were age-standardized to the Segi's 1960 world standard, using the direct method. Annual percentage change (APC) was used to compare changes in gynecologic cancer mortality by age group within each time period. We also compared age-specific mortality rates across three calendar periods (1979 to 1988, 1989 to 1998, and 1999 to 2010). Trends in gynecologic cancer mortality were assessed using joinpoint regression model. This analysis was performed using the Joinpoint software ver. 3.5.3 from the Surveillance Research Program of the US National Cancer Institute (Bethesda, MD, USA) [19]. The joinpoint method identifies the best-fit lines through several years of data. The method proceeds by fitting a series of joined lines, which are straight on a logarithmic scale, to trends in the annual age-adjusted cancer mortality rates. The line segments are joined at points called joinpoints, each of which indicates a statistically significant change in trend.
Table 1 presents age-standardized uterine and ovarian cancer mortality rates per 100,000 women for each region. In general, mortality rates due to uterine cancer are higher than those due to ovarian cancer. During 1966 to 2009, Singapore experienced the highest uterine cancer mortality rates among the four regions. In 2009, Korea had the lowest uterine cancer mortality rates among these regions. Between 2000 and 2009, Singapore had the highest ovarian cancer mortality rates. Furthermore, Korea and Hong Kong had the lowest ovarian cancer mortality rates.
Fig. 1A presents overall trends in uterine cancer mortality rates for each of the four East Asian regions. When certified uterine cancer deaths (ICD-10: C53, C54, and C55) are plotted, a significantly decreasing trend is evident throughout the entire study period.
Indeed, overall, uterine cancer mortality rates significantly declined across the study period for each of the four regions (Table 2, Fig. 1A). During the entire study period, Singapore had the highest uterine cancer mortality of the four regions, although there has been a trend of decreasing uterine cancer mortality in Singapore since 1966 (APC, -2.3%; 95% confidence interval [CI], -2.6 to -2.1). In Hong Kong, there was an overall trend of decrease of uterine cancer mortality since at least 1966 (APC, -4.0%; 95% CI, -4.6 to -3.5). More rapid reductions in uterine cancer mortality occurred in Japan between 1970 and 1990 (APC, -4.9%; 95% CI, -5.1 to -4.8) and in Korea between 1994 and 2010 (APC, -4.4%; 95% CI, -4.8 to -4.0). After 1990, however, the trend of decreased mortality began to slow in Japan. In the three Asian countries and Hong Kong, uterine cancer mortality rates have been declining significantly in almost all age groups. Fig. 2A presents changes in mortality rates by age group. Interestingly, the uterine cancer mortality rates tended to increase among women 20 to 34 years of age in Japan and among women over 70 years of age in Korea.
Overall, no significant changes in ovarian cancer mortality were observed, except in Korea and Japan (Table 2). In Korea, ovarian cancer mortality rates significantly increased (APC, 2.6%; 95% CI, 1.8 to 3.5) across the entire period (1995 to 2010). Especially, rapid increase in ovarian cancer mortality occurred during 1995 to 2000 (APC, 6.2%; 95% CI, 3.4 to 9.0). In Japan, ovarian cancer mortality rates began to increase during 1990 to 1997 (APC, 1.1%; 95% CI, 0.4 to 1.8). Subsequently, the mortality rates appeared to decline, but the reduction was not statistically significant. Fig. 1B presents overall trends in ovarian cancer mortality rates for the four regions that were investigated in the current study. Fig. 2B presents ovarian cancer mortality by age group, again for each of these four regions. Among women older than 70 years, prominent increasing trends were found in Japan, Korea, and Singapore.
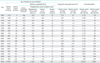
Table 3 presents our method of correcting the number of annual deaths due to uterine cervix and uterine corpus cancer, based on the NCIDB in Korea. The proportion of all uterine cancer deaths with unspecified subtype was the highest in 1993 (69.2%) and gradually diminished until 2010 (7.4%), which suggest significant improvement of quality of the death certificate over the past two decades.
Fig. 3 presents the overall trends in cervical and uterine corpus cancer mortality rates in Korea, using the corrected estimates of mortality. After corrections, it was evident that overall age-standardized cervical cancer mortality rates significantly declined during 1993 to 2010 (APC, -4.8%; 95% CI, -5.3 to -4.4). On the other hand, increase in corrected uterine corpus mortality rates were observed during 1995 to 2010 (APC, 6.7%; 95% CI, 5.4 to 8.0). Suppl. Table 1 and Fig. 1 present changes in mortality rates by age group. Whereas cervical cancer mortality rates have been declining significantly in almost all age groups, a nonsignificant trend of increasing mortality rates was found among women 20 to 34 years of age after 2004 (APC, 6.4%; 95% CI, -2.6 to 16.2).
In the present study, we compared and assessed secular trends of gynecologic cancer mortality among four East Asian female populations, including specific examinations of age-specific mortality. In some European countries, over 70% of deaths from uterine cancer were allotted to "uterus unspecified" during 1960; however, this proportion had reduced to 30% by around 1995 [14]. In Korea, a proportion of classification of "uterus, unspecified" has decreased from 69.1% of uterine cancer deaths in 1993 to 18.4% of uterine cancer deaths in 2002 [17]. We corrected the counts of cervical cancer and uterine corpus cancer deaths by referencing NCIDB in Korea. Our correction procedure allowed us to estimate separate mortality rates for cervical and uterine corpus cancer. After correcting the WHO mortality data, we found that cervical cancer mortality rates had decreased since at least 1993. On the other hand, the corrected data also revealed a trend of increasing uterine corpus cancer mortality rates, which began during or before 1995.
Considering the similar cancer mortality patterns that we observed across the four Asian regions, it is likely that the majority of deaths registered as "uterus, unspecified site" are the result of cervical cancer, as we found in Korea. Therefore, the overall trend of declining uterine cancer mortality might be attributed to the specific decline in cervical cancer mortality. This finding is also confirmed by gynecologic cancer mortality statistics from the Singapore Cancer Registry (Suppl. Fig. 2) [20].
Cervical cancer mortality has been decreasing in most developed countries, possibly as a result of early diagnosis and improved treatments [12,21,22,23]. Two causes likely explain the majority of the trend of decreasing cervical cancer mortality that we found in the four East Asian regions. First, mortality reductions have resulted from trends of decreasing incidence. Particularly, cervical cancer incidence has decreased as lesions have been detected increasingly early, when they are precancerous. The value of cervical cancer screening programs is widely accepted, and national screening programs for cervical cancer have been introduced in Japan (1983), Korea (1988), Taiwan (1995), and Hong Kong (2004). Cervical cancer screening programs have led to decreases in the incidence of invasive cervical cancer in Japan [7], Korea [24], and Taiwan [25]. Further, successful treatment of precancerous lesions (such as intraepithelial neoplasm and carcinoma in situ) has resulted in a decreasing trend of invasive cervical cancer. Second, mortality reductions have resulted from advances in cervical cancer therapy, particularly the introduction of concurrent chemoradiation. In 1999, Keys et al. [26] demonstrated that concurrent chemoradiation is associated with better outcomes than radiation alone. Since then, concurrent chemoradiation has been accepted as a standard treatment in the form of either a primary treatment or adjuvant treatment after surgery.
A worrying finding of our study was that uterine cancer mortality rates appeared to be increasing among women <50 years in Japan. Most deaths from uterine cancer among women <50 years can be attributed to cervical cancers [14]. Accordingly, the trend of increasing uterine cancer among younger women in Japan may reflect the trend of increasing cervical cancer incidence in this same population [27,28,29]. In Korea, cervical cancer mortality rates tended to increase among women 20 to 34 years of age after 2004. Although this increase was not statistically significant (APC, 6.4%; 95% CI, -2.6 to 16.2), further efforts are required to improve the outcomes in this young age group.
Despite decreasing trends of cervical cancer mortality in Asian countries, cervical cancer still has the second greatest incidence of all cancers among young women in East Asian countries [30]. Because cervical cancer has been demonstrated to be a preventable disease, additional efforts are warranted in East Asia. Specific strategies to prevent cervical cancer are required, including both primary and secondary preventive measures, such as human papillomavirus vaccination and national cervical cytology screening.
Although the trends of decreasing cervical cancer mortality are promising, our results show an abrupt increase in uterine corpus cancer mortality in Korea. This finding should be interpreted in the context of the abruptly increasing incidence of endometrial cancer in East Asia [7,31]. Uterine cancer is mainly diagnosed among postmenopausal women. Endometrial cancer constitutes the majority of cases, while uterine sarcoma is a rare malignancy that accounts for approximately 3% of all uterine cancers [32]. Although endometrial cancer is the most common malignancy of the female genital tract in Western countries, its incidence is rather low in East Asia [33]. Changes in risk factors, especially those associated with lifestyle, have been suggested as the principal cause of the increasing endometrial cancer incidence in East Asia [31]. In particular, one of the established risk factors for endometrial cancer is an increase in unopposed estrogen, which can result from obesity or diabetes mellitus. Based on the trend of increasing uterine corpus cancer incidence that has been reported [34], we suggest that the burden of mortality from uterine corpus cancer will also increase in East Asia within the near future.
A troubling finding of the present study was the persistently high pattern of ovarian cancer mortality rates in Hong Kong, Japan, and Singapore, along with the trend of increased mortality in Korea. In Korea, increases in ovarian cancer mortality rates were found for all age groups, except women 20 to 34 years of age. In Japan and Singapore, it appeared that past age-specific decreases ovarian cancer mortality were reversing.
In the United States, ovarian cancer mortality rates leveled off during the 1980s and declined during the 1990s, with an annual average change of 0.9% [35]. Three or more years of oral contraceptive use reduces the risk of ovarian cancer, and consequently, widespread use of oral contraceptives has contributed to the trend of declining mortality [36]. Although oral contraceptives have long been the most common method of contraception for women in the United States and European countries, the rate of contraceptive use in East Asia has been substantially lower. The proportion of the Chinese women who used pills was only 2.1% in 2006 [37], while approximately 30% of European women used oral contraceptives in 2003 [38]. Therefore, the protective effects of oral contraceptives only contribute minimally to population cancer rates in Korea. In addition, early age at menarche, late age at menopause, lower fertility rates, and other reproductive factors are also risk factors for ovarian cancer. Korea and Japan are among the countries that have the lowest total fertility rates. Indeed, the total fertility rate has remained below 1.3 in Korea since 2005 [39]. East Asia underwent rapid industrialization during the 1960s, and Asian women born after the 1960s have tended to undergo menarche at earlier, delay childbirth, and have reduced fertility rates. The very low fertility rate and the low use of oral contraceptives will presumably sustain the trend of increasing ovarian cancer rates in East Asia [40]. Considering that epithelial ovarian cancer is mostly found at an advanced stage, and has low survival rates, we expect the burden from ovarian cancer to increase in Asian countries. Therefore, improvements to optimal cytoreductive surgery and new therapeutic modalities are urgently required for ovarian cancer.
In the current study, most of the deaths due to ovarian cancer occurred in women older than 50 years. Mortality rates for women over 70 years of age showed an increasing trend in Asian countries, while rates for women younger than 35 years remained stable or decreased. The present study shows that mortality rates for women over 70 years of age have doubled in past 20 years in Korea and Singapore. Considering that ovarian cancer incidence has not increased abruptly during the same period (and indeed has remained stable) [34], the increasing trend of mortality in old age groups could be the result of under treatment of ovarian cancer [41]. Elderly patients have been less likely to undergo standard treatments for ovarian cancer, such as optimal debulking surgery, and have been less likely to complete chemotherapy. Indeed, it has been reported that, among patients who do receive optimal treatment, old age is not an independent poor prognostic factor [42].
The main limitation to this study is the presence of "uterus, unspecified site" as the cause of death on many death certificates. This made it impossible to evaluate cervical and uterine corpus cancer trends separately, based on the WHO mortality database alone. We corrected Korean cervical and uterine corpus cancer mortality rates using Korea NCIDB. However, we were unable to correct the mortality rates for other regions. In addition, this study is limited by several problems that are inherent to the WHO mortality database. Specifically, some mortality data are incomplete and the database does not include full coverage of all deaths in every region. Inaccuracies in death registration coverage and cross-national differences in coding practices should be considered when applying the results of this study.
In conclusion, uterine cancer mortality has decreased in Hong Kong, Japan, Korea, and Singapore. After correcting the cervical and uterine corpus mortality rates in Korea, a significant trend of decreasing mortality was found for cervical cancer, and a trend of rapidly increasing mortality was observed for uterine corpus cancer. The most important contributor to declines in cervical cancer mortality has been the early diagnosis and improved treatments. Overall, ovarian cancer mortality was stable in East Asia, with the exception of Korea. A continuing increase in ovarian cancer mortality should be expected because of trend of increasing incidence in East Asia. Preventive measures, early detection programs, and standard use of optimal therapeutic strategies are urgently required, particularly for older age groups. Such improvements could include obesity control programs, increases in fertility, wider oral contraceptive use, optimal cytoreductive surgery, and novel target agents.
Figures and Tables
Fig. 1
Trends in uterine* and ovarian cancer mortality rates (age-standardized, women ≥20 years) obtained by joinpoint regression for 4 female Asian populations. (A) Uterine cancer. (B) Ovarian cancer. *Uterine cancer includes cervix uteri (International Statistical Classification of Disease and Related Health Problems, 10th revision [ICD-10] code C53); corpus uteri (ICD-10 code C54); and uterus, unspecified (ICD-10 code C55).
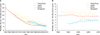
Fig. 2
Uterine and ovarian cancer mortality by age group, period, and region. (A) Uterine cancer. (B) Ovarian cancer. *Uterine cancer includes cervix uteri (International Statistical Classification of Disease and Related Health Problems, 10th revision [ICD-10] code C53); corpus uteri (ICD-10 code C54); and uterus, unspecified (ICD-10 code C55).

Fig. 3
Corrected trends in cervical and uterine corpus cancer mortality in Korea (age-standardized, women ≥20 years) obtained by joinpoint regression. (A) Cervix. (B) Corpus uteri.
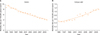
Table 1
Gynecologic cancer deaths and age-adjusted mortality rates among women ≥20 years according to region and calendar year

Table 2
Estimated annual percentage change of gynecologic cancer death rates, with 95% CIs

APC, annual percentage change; CI, confidence interval.
*Uterine cancer includes cervix uteri (International Statistical Classification of Disease and Related Health Problems, 10th revision [ICD-10] code C53); corpus uteri (ICD-10 code C54); and uterus, unspecified (ICD-10 code C55). †The APC is significantly different from zero (p<0.05).
ACKNOWLEDGEMENTS
This study was supported by the National Cancer Center Grant of Korea (NCC-1310222).
References
1. Felay J, Shin H, Bray F, Forman D, Mathers C, Parkin D. GLOBOCAN 2008: cancer incidence and mortality worldwide: IARC CancerBase No. 10. Lyon: IARC Press;2010.
2. Akhtar-Danesh N, Elit L, Lytwyn A. Temporal trends in the relative survival among women with cervical cancer in Canada: a population-based study. Int J Gynecol Cancer. 2012; 22:1208–1213.
3. Bray F, Loos AH, Tognazzo S, La Vecchia C. Ovarian cancer in Europe: cross-sectional trends in incidence and mortality in 28 countries, 1953-2000. Int J Cancer. 2005; 113:977–990.
4. Gonzalez-Diego P, Lopez-Abente G, Pollan M, Ruiz M. Time trends in ovarian cancer mortality in Europe (1955-1993): effect of age, birth cohort and period of death. Eur J Cancer. 2000; 36:1816–1824.
5. Hannibal CG, Cortes R, Engholm G, Kjaer SK. Survival of ovarian cancer patients in Denmark: excess mortality risk analysis of five-year relative survival in the period 1978-2002. Acta Obstet Gynecol Scand. 2008; 87:1353–1360.
6. Chung HH, Jang MJ, Jung KW, Won YJ, Shin HR, Kim JW, et al. Cervical cancer incidence and survival in Korea: 1993-2002. Int J Gynecol Cancer. 2006; 16:1833–1838.
7. Katanoda K, Matsuda T, Matsuda A, Shibata A, Nishino Y, Fujita M, et al. An updated report of the trends in cancer incidence and mortality in Japan. Jpn J Clin Oncol. 2013; 43:492–507.
8. Cramer DW. The epidemiology of endometrial and ovarian cancer. Hematol Oncol Clin North Am. 2012; 26:1–12.
9. Pasalich M, Su D, Binns CW, Lee AH. Reproductive factors for ovarian cancer in southern Chinese women. J Gynecol Oncol. 2013; 24:135–140.
10. World Health Organization Statistical Information System. WHO mortality database [Internet]. Geneva: World Health Organization;c2014. cited 2013 Jul 29. Available from: http://www.who.int/healthinfo/mortality_data/en/.
11. World Health Organization. International statistical classification of idseases and related health problems. Geneva: World Health Organization;1994.
12. Arbyn M, Geys H. Trend of cervical cancer mortality in Belgium (1954-1994): tentative solution for the certification problem of unspecified uterine cancer. Int J Cancer. 2002; 102:649–654.
13. Bosch FX. Trends in cervical cancer mortality. J Epidemiol Community Health. 1999; 53:392.
14. Levi F, Lucchini F, Negri E, Franceschi S, la Vecchia C. Cervical cancer mortality in young women in Europe: patterns and trends. Eur J Cancer. 2000; 36:2266–2271.
15. Loos AH, Bray F, McCarron P, Weiderpass E, Hakama M, Parkin DM. Sheep and goats: separating cervix and corpus uteri from imprecisely coded uterine cancer deaths, for studies of geographical and temporal variations in mortality. Eur J Cancer. 2004; 40:2794–2803.
16. Shin HR, Won YJ, Jung KW, Kong HJ, Yim SH, Lee JK, et al. Nationwide cancer incidence in Korea, 1999-2001: first result using the national cancer incidence database. Cancer Res Treat. 2005; 37:325–331.
17. Shin HR, Park S, Hwang SY, Kim JE, Jung KW, Won YJ, et al. Trends in cervical cancer mortality in Korea 1993-2002: corrected mortality using national death certification data and national cancer incidence data. Int J Cancer. 2008; 122:393–397.
18. Segi M, Fujisaku S. Cancer mortality for selected sites in 24 countries (1950-1957). Sendai: Department of Public Health, Tohoku University School of Medicine;1960.
19. Joinpoint Regression Program version 3.5.3 [Internet]. 2012 ed. Bethesda, MD: National Cancer Institute;2012. cited 2012 Aug 5. Available from: http://surveillance.cancer.gov/joinpoint/.
20. Ministry of Health. National Registry of Disease Office [Interent]. Singapore: Ministry of Health;c2013. cited 2013 Nov 3. Available from: https://www.nrdo.gov.sg/page.aspx?id=76.
21. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009; 59:225–249.
22. Minelli L, Stracci F, Prandini S, Moffa IF, La Rosa F. Gynaecological cancers in Umbria (Italy): trends of incidence, mortality and survival, 1978-1998. Eur J Obstet Gynecol Reprod Biol. 2004; 115:59–65.
23. Remontet L, Esteve J, Bouvier AM, Grosclaude P, Launoy G, Menegoz F, et al. Cancer incidence and mortality in France over the period 1978-2000. Rev Epidemiol Sante Publique. 2003; 51(1 Pt 1):3–30.
24. Jung KW, Won YJ, Kong HJ, Oh CM, Seo HG, Lee JS. Cancer statistics in Korea: incidence, mortality, survival and prevalence in 2010. Cancer Res Treat. 2013; 45:1–14.
25. Chen YY, You SL, Chen CA, Shih LY, Koong SL, Chao KY, et al. Effectiveness of national cervical cancer screening programme in Taiwan: 12-year experiences. Br J Cancer. 2009; 101:174–177.
26. Keys HM, Bundy BN, Stehman FB, Muderspach LI, Chafe WE, Suggs CL 3rd, et al. Cisplatin, radiation, and adjuvant hysterectomy compared with radiation and adjuvant hysterectomy for bulky stage IB cervical carcinoma. N Engl J Med. 1999; 340:1154–1161.
27. Kokawa K, Takekida S, Kamiura S, Kita M, Enomoto T, Kawaguchi R, et al. The incidence, treatment and prognosis of cervical carcinoma in young women: a retrospective analysis of 4,975 cases in Japan. Eur J Gynaecol Oncol. 2010; 31:37–43.
28. Banzai C, Yahata T, Tanaka K. Trends in the incidence of uterine cancer in Niigata, Japan: a population-based study from 1982 to 2007. Eur J Gynaecol Oncol. 2011; 32:521–524.
29. Yang L, Fujimoto J, Qiu D, Sakamoto N. Trends in cancer mortality in Japanese adolescents and young adults aged 15-29 years, 1970-2006. Ann Oncol. 2009; 20:758–766.
30. Arbyn M, Castellsague X, de Sanjose S, Bruni L, Saraiya M, Bray F, et al. Worldwide burden of cervical cancer in 2008. Ann Oncol. 2011; 22:2675–2686.
31. Huang CY, Chen CA, Chen YL, Chiang CJ, Hsu TH, Lin MC, et al. Nationwide surveillance in uterine cancer: survival analysis and the importance of birth cohort: 30-year population-based registry in Taiwan. PLoS One. 2012; 7:e51372.
32. D'Angelo E, Prat J. Uterine sarcomas: a review. Gynecol Oncol. 2010; 116:131–139.
33. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005; 55:74–108.
34. Lim MC, Moon EK, Shin A, Jung KW, Won YJ, Seo SS, et al. Incidence of cervical, endometrial, and ovarian cancer in Korea, 1999-2010. J Gynecol Oncol. 2013; 24:298–302.
35. Wingo PA, Cardinez CJ, Landis SH, Greenlee RT, Ries LA, Anderson RN, et al. Long-term trends in cancer mortality in the United States, 1930-1998. Cancer. 2003; 97:12 Suppl. 3133–3275.
36. Mant JW, Vessey MP. Ovarian and endometrial cancers. Cancer Surv. 1994; 19-20:287–307.
37. Zheng X, Tan L, Ren Q, Cui Z, Wu J, Lin T, et al. Trends in contraceptive patterns and behaviors during a period of fertility transition in China: 1988-2006. Contraception. 2012; 86:204–213.
38. Skouby SO. Contraceptive use and behavior in the 21st century: a comprehensive study across five European countries. Eur J Contracept Reprod Health Care. 2010; 15:Suppl 2. S42–S53.
39. Central Intelligence Agency. CIA world factbook [Internet]. Washington, DC: Central Intelligence Agency;c2013. cited 2013 Nov 3. Available from: https://www.cia.gov/library/publications/the-world-factbook/.
40. Wong KH, Mang OW, Au KH, Law SC. Incidence, mortality, and survival trends of ovarian cancer in Hong Kong, 1997 to 2006: a population-based study. Hong Kong Med J. 2012; 18:466–474.
41. Bouchardy C, Rapiti E, Blagojevic S, Vlastos AT, Vlastos G. Older female cancer patients: importance, causes, and consequences of undertreatment. J Clin Oncol. 2007; 25:1858–1869.
42. Jorgensen TL, Teiblum S, Paludan M, Poulsen LO, Jorgensen AY, Bruun KH, et al. Significance of age and comorbidity on treatment modality, treatment adherence, and prognosis in elderly ovarian cancer patients. Gynecol Oncol. 2012; 127:367–374.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download