Abstract
Objective
To assess the use of colony-stimulating factors (CSFs) in patients with ovarian cancer who receive adjuvant paclitaxel and carboplatin chemotherapy in clinical practice and to assess whether the frequency of CSF use differs among hospitals in Japan.
Methods
CSF use in patients with ovarian cancer who received first-line paclitaxel and carboplatin was analyzed retrospectively using data from the Japanese hospitalization payment system.
Results
A total of 1,050 patients at 104 hospitals were identified. The median age was 60 years (range, 22 to 88 years). Of these, 163 patients (15.5%) were diagnosed with neutropenia and 134 patients (12.8%) received CSFs. Among the patients who received CSFs, 125 (93%) received them for the treatment of neutropenia without fever and 1 received them for febrile neutropenia. In total, CSFs were administered for 272 cycles of chemotherapy. Among them, CSFs were used as treatment for neutropenia without fever in 259 cycles (95%), as prophylaxis (primary or secondary) in 12 cycles (4%), and as treatment for febrile neutropenia in 1 cycle. Among hospitals, a median of 4.0% of patients received CSFs with an interquartile range of 25% (Q1, 0%; Q3, 25%). A logistic random effects model showed that the variation in the proportion of patients receiving CSFs among the 104 hospitals was 2.0 (p<0.001), suggesting that the use of CSFs varied across hospitals.
Neutropenia is a serious complication associated with chemotherapy. Febrile neutropenia can be fatal. Hematopoietic colony-stimulating factors (CSFs) are administered to patients receiving chemotherapy to reduce the risk of neutropenia with or without febrile neutropenia. There are several indications for administration of CSFs: primary prophylaxis, secondary prophylaxis, and therapeutic use. Primary prophylaxis is defined as the administration of CSFs 24-72 hours after the first cycle of chemotherapy. Secondary prophylaxis is defined as the administration of CSFs to patients who experienced febrile neutropenia during a previous cycle of chemotherapy. Therapeutic use is defined as the administration of CSFs to patients with neutropenia or febrile neutropenia after the administration of chemotherapy [1]. To standardize the use of CSFs, clinical guidelines have been developed by the American Society of Clinical Oncology [1], the National Comprehensive Cancer Network [2], and the European Organization for Research and Treatment of Cancer [3]. All guidelines recommend primary prophylactic use of CSFs to prevent febrile neutropenia in patients who receive chemotherapy with a high risk (≥20%) of febrile neutropenia. The use of CSFs is also recommended for patients with an intermediate risk (10%-20%) who have clinical factors predisposing them to prolonged neutropenia. These factors include older age, poor performance status, previous episodes of febrile neutropenia, extensive prior treatment (radiation or administration of combination chemotherapy), cytopenia due to bone marrow involvement by the tumor, poor nutritional status, presence of open wounds or active infections, and a more advanced cancer [1,2,3]. Although secondary prophylaxis with CSFs is recommended for patients who have experienced febrile neutropenia during a previous cycle of chemotherapy, dose reduction or delay is the preferred alternative in such cases. Therapeutic use of CSFs is not recommended for the treatment of febrile neutropenia or severe neutropenia without fever. Routine therapeutic application of CSFs in patients with afebrile neutropenia does reduce the duration of neutropenia, but it does not seem to produce the clinical benefits associated with CSF therapy, such as reductions in hospitalization rate, hospitalization stay, and rate of infection [4]. Moreover, CSF therapy does not reduce the risk of death due to febrile neutropenia [5].
Although the use of CSFs is restricted according to the guidelines, little is known about its use in clinical practice. Surveys have suggested that physicians prescribe CSFs for indications not supported by the guidelines and that CSFs are generally overused [6,7]. Considering the high cost of CSFs (US $300 per dose in Japan) and their adverse events, such as injection-site discomfort, fever, bone pain, and splenic rupture [8], their use should be optimized and standardized in clinical practice.
Clinical trials have reported that the incidence of febrile neutropenia in patients with ovarian cancer receiving paclitaxel and carboplatin (TC) chemotherapy is<10% [9,10], and the guidelines indicate that CSFs are not needed for primary prophylaxis in these patients. To assess the actual use of CSFs in patients with ovarian cancer, we analyzed the rate of their use and the difference in practice patterns among hospitals for patients who received first-line TC chemotherapy. We used data from the diagnosis procedure combination (DPC) system, the Japanese hospitalization payment system.
We retrospectively analyzed accessible DPC data collected by the Global Health Consulting Japan Co., Ltd from 104 hospitals in Japan between July 2011 and February 2012. Global Health Consulting Japan Co. Ltd is a consulting company specialized in the management of medical institutions. The hospitals included in the study were those that outsourced the DPC data analysis to the company. All hospitals consented to the use of their data for this study. A nondisclosure agreement regarding the use of data was signed by the company and the Department of Medical Oncology of Nippon Medical School Musashikosugi Hospital. This study was approved by the Institutional Review Board of Nippon Medical School Musashikosugi Hospital (approval number 324014).
Japan has used an exclusive fee-for-service system since universal healthcare coverage was implemented in the 1960s. However, when faced with a medical care financial crisis, the Japanese government introduced prospective payment instead of a fee-for-service payment to reduce the length of hospital stay and improve medical care efficiency. The DPC system was introduced in 2003 and records inpatient medical care costs. It covers 18 major diagnosis categories and includes 1,880 diagnosis groups. Approximately 1,500 hospitals in Japan have adopted the DPC payment system [11].
We selected a dataset of patients with ovarian cancer who received first-line TC chemotherapy between July 2011 and February 2012. Data from 1,050 patients treated at 104 hospitals were analyzed. DPC data analyzed included patient age, clinical stage, Barthel activities of daily living index (BADLI), number of chemotherapy cycles, number of cycles for which CSFs were administered, diagnosis of grade 3 or 4 neutropenia according to the Common Terminology Criteria for Adverse Events ver. 4.0, and diagnosis of febrile neutropenia. Laboratory data and the purpose of CSF use (primary prophylaxis, secondary prophylaxis, or therapeutic use) were not recorded in the DPC system.
BADLI is a scale used to measure activities of daily living (ADL) by evaluating 10 basic daily activities: (1) feeding, (2) personal hygiene, (3) toilet use, (4) bathing, (5) dressing, (6) bowel and bladder control, (7) mobility, (8) chair-to-bed transfer, (9) ability to go up a flight of stairs, and (10) ability to go down a flight of stairs. Scores range from 0 to 100, with 0 indicating maximum dependence and 100 indicating total independence for these evaluated daily activities [12].
The rate of use of CSFs at each hospital, defined as the number of ovarian cancer patients who received CSFs divided by the number who received first-line TC chemotherapy, was calculated. Descriptive analyses were based on frequencies and medians with interquartile ranges. A logistic random effects model was used to evaluate variations in the rate of use of CSFs among the 104 hospitals. The hospitals were classified into two groups according to the rate of use of CSFs: group 1 consisted of 51 hospitals, involving 916 patients, in which CSFs were not used; group 2 consisted of 53 hospitals, involving 134 patients, in which CSFs were administered to at least 1 patient. Distributions according to age (≥65 years or <65 years), neutropenia (yes or no), BADLI (0-50, 51-80, 81-100, or unknown), and stage (I, II, III, IV, or unknown) were compared between the two groups using Fisher exact test. A 2-sided p<0.05 was considered statistically significant. All statistical analyses were performed using SAS ver. 9.3 (SAS Institute Inc., Cary, NC, USA).
The study population consisted of 1,050 patients treated at 104 hospitals. These patients received a total of 3,341 cycles of chemotherapy during the study period. The median age was 60 years (range, 22 to 88 years). Most patients (96%) had high ADL scores (BADLI 80-100). Of the 1,050 patients, 108 (10%) had International Federation of Gynecology and Obstetrics (FIGO) stage I disease, 33 (3%) had stage II disease, 129 (12%) had stage III disease, 58 (6%) had stage IV disease, and 722 (69%) had disease of unknown stage. Similarly, 163 patients (15.5%) were diagnosed with neutropenia and 134 patients (12.8%) received CSFs. Only 2 patients were diagnosed with febrile neutropenia. Among the patients who received CSFs, 125 patients (93%) received CSFs for the treatment of neutropenia without fever, 8 patients (6%) received CSFs as prophylaxis, and 1 patient received CSFs for febrile neutropenia. In total, CSFs were used in 272 cycles of chemotherapy. Of these, CSFs were used as treatment for neutropenia without fever in 259 cycles (95%), as prophylaxis (primary or secondary) in 12 cycles (4%), and as treatment for febrile neutropenia in 1 cycle.
The characteristics of the 916 patients treated at the 51 hospitals in which CSFs were not used (group 1) and the 134 patients treated at the 53 hospitals in which CSFs were used (group 2) are listed in Table 1. A higher proportion of older patients (p=0.01) and patients with neutropenia (p<0.001) tended to receive CSFs. The mean number of chemotherapy cycles per patient was 3.1 (range, 1 to 21) in group 1, and 3.8 (range, 1 to 18) in group 2 (p=0.017).
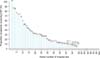
The median number of patients per hospital was 10 (range, 1 to 42). Fig. 1 shows the distribution of the proportion of patients receiving CSFs at each hospital. The median proportion of patients who received CSFs was 4.0%, and the interquartile range was 25%. In addition, our logistic random effects model showed that variation in the proportion of patients receiving CSFs in the 104 hospitals was 2.0 (p<0.001), suggesting that the rate of CSFs administration varied across hospitals. The hospitals in which CSFs were used in a high proportion of patients tended to treat only a small number of patients.
We analyzed the clinical practice patterns of the use of CSFs in patients with ovarian cancer receiving TC chemotherapy using data from the Japanese DPC. Overall, 12.8% of the 1,050 patients received CSFs, and this rate is similar to that found in previous trials [9,10,13]. In addition, 95% of patients received CSFs in response to neutropenia and 4% received CSFs for prophylaxis. Older patients and patients with neutropenia tended to receive CSFs; ADL and disease stage did not influence the decision to use CSFs. The frequency of the use of CSFs varied widely among hospitals.
Several studies have evaluated the discretionary use of CSFs in clinical practice. Their results suggest that CSFs are underutilized in patients treated with chemotherapy regimens who are at high risk for febrile neutropenia, and overutilized in patients treated with chemotherapy regimens who are at low risk for febrile neutropenia [6,7]. A nationwide survey in the United States showed that 67% of gynecologic oncologists who routinely administer chemotherapy prefer to use CSFs for secondary prophylaxis after a neutropenic complication. Only 2% use CSFs for primary prophylaxis in first-line treatment for ovarian cancer and most use CSFs to maintain relative dose intensity in their patients [14]. However, most physicians did not use CSFs for prophylaxis but for treatment of neutropenia in this study.
In Japan, CSFs tend to be used frequently. In the Japanese Gynecologic Oncology Group (JGOG) 3016 trial, comparisons between the dose-dense weekly TC and TC every 3 weeks for patients with advanced ovarian cancer showed that 67% and 60% of patients received CSFs, respectively [9]. Frequent use of CSFs may be attributable to the provisions of the Japanese health insurance system. Japan has a universal national health insurance system, and physician compensation is not directly affected by drug administration. A cohort study in the United States showed that enrollment in a health maintenance organization (HMO), in which physician compensation is unrelated to treatment, was strongly associated with a lower rate of discretionary use of CSFs compared with non-enrollment in an HMO [7]. These findings suggest that financial incentives may drive the discretionary use of CSFs. The Japanese health insurance system pays for treatment with CSFs for adult and pediatric patients with solid tumors who have a neutrophil count of<500/mm3 or fever of >38℃ and a neutrophil count of<1,000/mm3 while receiving chemotherapy [15]. These criteria may contribute to the use of CSFs with a therapeutic intent.
The frequency of the use of CSFs varied widely among hospitals. This variation suggests that appropriate use of CSFs is not standardized among the hospitals included in this study. Moreover, the hospitals where CSFs were used in a high proportion of patients tended to treat only small number of patients. Several studies have reported that the clinical outcomes of ovarian cancer treatment differ across institutions; patients who are treated at specialized, high-volume centers are more likely to have improved surgical and chemotherapy outcomes [16,17,18]. It is essential for institutions to treat a critical number of patients for medical professionals to develop and maintain their expertise. Appropriate use of CSFs requires physicians to have an in-depth knowledge of chemotherapy regimens; consequently, such expertise might vary among the hospitals included in this study.
In this study, the rate of febrile neutropenia was extremely low at 0.2% (2 patients), much lower than those previously reported for patients undergoing TC chemotherapy. The rate of neutropenia, febrile neutropenia, and receiving CSFs were 88%, 9%, and 67%, respectively, in the JGOG 3016 study [9], and 31.8%, 8%, and 14.4%, respectively, in the Arbeitsgemeinschaft Gynakologische Onkologie (AGO) group study [10]. Thus, Japanese patients received more CSFs than do European patients, but the occurrence of febrile neutropenia was similar in the 2 studies. In this study, the therapeutic use of CSFs for patients with neutropenia without fever might prevent the occurrence of febrile neutropenia. However, the therapeutic use of CSFs in patients with afebrile neutropenia does not provide its known clinical benefits [4] and the use of CSFs for febrile neutropenia does not reduce the risk of death [5]. Moreover, considering the cost (US $300 per dose in Japan) and adverse events, such as injection site discomfort, fever, bone pain, and splenic rupture [8], use of CSFs in patients with afebrile neutropenia should be limited in clinical practice. However, CSFs should be administered as secondary prophylaxis to prevent neutropenia.
Our study has several limitations. First, this study was based only on data from hospitalized patients. Thus, we might not be able to extrapolate our findings to the general population. However, patients in this study were not a high risk population: the median age was 60 years, most patients had good ADL scores, and most patients did not seem to have received prior chemotherapy in a first-line setting. Furthermore, a report from the Japanese government showed that, of 796 hospitals adopting the DPC payment system, 89% administered TC chemotherapy to patients with ovarian cancer on an inpatient basis in 2010 [19]. Therefore, our study population seems to reflect practice patterns for use of CSFs in Japanese patients with ovarian cancer. Many Japanese patients have reported concerns about receiving chemotherapy at outpatient clinics because of the possibility of adverse events, inconvenience to their families, and their desire to have consultations in the evenings or during holidays [20]. These concerns may have led to the high percentage of hospitals administering chemotherapy on an inpatient basis. Second, a considerable amount of data were missing, including data on clinical stages for 70% of our patients, patient comorbidities, prior chemotherapy or radiation treatment, nutritional status, and presence of open wounds or active infections. In patients who received CSFs for prophylaxis, we could not determine if this was for primary or secondary prophylaxis. We used BADLI instead of performance status to evaluate general patient status, although this is not commonly used to evaluate cancer patients [21,22]. These limitations prevented complete evaluation of the risk factors that influenced use of CSFs.
In conclusion, the frequency of use of CSFs in patients with ovarian cancer receiving first-line TC chemotherapy differed significantly among hospitals. Most patients received CSFs in response to neutropenia, not for prophylaxis or febrile neutropenia. Standardized and evidence-based use of CSFs is required. The therapeutic administration of CSFs in afebrile patients with neutropenia might lower the rate of febrile neutropenia; however, considering that CSFs for the treatment of febrile neutropenia do not reduce the risk of death, their cost, and their adverse events, administration of CSFs in patients with afebrile neutropenia should be limited.
Figures and Tables
References
1. Smith TJ, Khatcheressian J, Lyman GH, Ozer H, Armitage JO, Balducci L, et al. 2006 update of recommendations for the use of white blood cell growth factors: an evidence-based clinical practice guideline. J Clin Oncol. 2006; 24:3187–3205.
2. Crawford J, Armitage J, Balducci L, Becker PS, Blayney DW, Cataland SR, et al. NCCN clinical practice guidelines in oncology: Myeloid growth factors. ver. 2 [Internet]. Fort Washington, PA: National Comprehensive Cancer Network;2013. cited 2013 Nov 29. Available from: http://www.nccn.org/professionals/physician_gls/pdf/myeloid_growth.pdf.
3. Aapro MS, Bohlius J, Cameron DA, Dal Lago L, Donnelly JP, Kearney N, et al. 2010 update of EORTC guidelines for the use of granulocyte-colony stimulating factor to reduce the incidence of chemotherapy-induced febrile neutropenia in adult patients with lymphoproliferative disorders and solid tumours. Eur J Cancer. 2011; 47:8–32.
4. Hartmann LC, Tschetter LK, Habermann TM, Ebbert LP, Johnson PS, Mailliard JA, et al. Granulocyte colony-stimulating factor in severe chemotherapy-induced afebrile neutropenia. N Engl J Med. 1997; 336:1776–1780.
5. Garcia-Carbonero R, Mayordomo JI, Tornamira MV, Lopez-Brea M, Rueda A, Guillem V, et al. Granulocyte colony-stimulating factor in the treatment of high-risk febrile neutropenia: a multicenter randomized trial. J Natl Cancer Inst. 2001; 93:31–38.
6. Ramsey SD, McCune JS, Blough DK, McDermott CL, Clarke L, Malin JL, et al. Colony-stimulating factor prescribing patterns in patients receiving chemotherapy for cancer. Am J Manag Care. 2010; 16:678–686.
7. Potosky AL, Malin JL, Kim B, Chrischilles EA, Makgoeng SB, Howlader N, et al. Use of colony-stimulating factors with chemotherapy: opportunities for cost savings and improved outcomes. J Natl Cancer Inst. 2011; 103:979–982.
8. Bennett CL, Djulbegovic B, Norris LB, Armitage JO. Colony-stimulating factors for febrile neutropenia during cancer therapy. N Engl J Med. 2013; 368:1131–1139.
9. Katsumata N, Yasuda M, Takahashi F, Isonishi S, Jobo T, Aoki D, et al. Dose-dense paclitaxel once a week in combination with carboplatin every 3 weeks for advanced ovarian cancer: a phase 3, open-label, randomised controlled trial. Lancet. 2009; 374:1331–1338.
10. du Bois A, Luck HJ, Meier W, Adams HP, Mobus V, Costa S, et al. A randomized clinical trial of cisplatin/paclitaxel versus carboplatin/paclitaxel as first-line treatment of ovarian cancer. J Natl Cancer Inst. 2003; 95:1320–1329.
11. Ministry of Health, Labor, and Welfare. Overview of revision of payment system related to DPC 2012 [Internet]. Tokyo: Ministry of Health, Labor, and Welfare;cited 2013 Jun 29. Available from: http://www.mhlw.go.jp/bunya/iryouhoken/iryouhoken15/dl/h24_01-05.pdf.
12. Mahoney FI, Barthel DW. Functional evaluation: the barthel index. Md State Med J. 1965; 14:61–65.
13. Ozols RF, Bundy BN, Greer BE, Fowler JM, Clarke-Pearson D, Burger RA, et al. Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a Gynecologic Oncology Group study. J Clin Oncol. 2003; 21:3194–3200.
14. Alvarez Secord A, Bae-Jump V, Havrilesky LJ, Calingaert B, Clarke-Pearson DL, Soper JT, et al. Attitudes regarding the use of hematopoietic colony-stimulating factors and maintenance of relative dose intensity among gynecologic oncologists. Int J Gynecol Cancer. 2009; 19:447–454.
15. Pharmaceuticals and Medical Devices Agency. GRAN SYRINGE: usage and dosage/efficacy or effectiveness [Internet]. Tokyo: Pharmaceuticals and Medical Devices Agency;2013. cited 2013 Jun 29. Available from: http://www.info.pmda.go.jp/go/pack/3399405A1027_4_06/.
16. Vernooij F, Heintz P, Witteveen E, van der Graaf Y. The outcomes of ovarian cancer treatment are better when provided by gynecologic oncologists and in specialized hospitals: a systematic review. Gynecol Oncol. 2007; 105:801–812.
17. Chan JK, Kapp DS, Shin JY, Husain A, Teng NN, Berek JS, et al. Influence of the gynecologic oncologist on the survival of ovarian cancer patients. Obstet Gynecol. 2007; 109:1342–1350.
18. Vernooij F, Heintz AP, Coebergh JW, Massuger LF, Witteveen PO, van der Graaf Y. Specialized and high-volume care leads to better outcomes of ovarian cancer treatment in the Netherlands. Gynecol Oncol. 2009; 112:455–461.
19. Ministry of Health, Labor, and Welfare. Agenda, compensation survey and DPC evaluation subcommittee 9th FY 2011 [Internet]. Tokyo: Ministry of Health, Labor, and Welfare;cited 2013 Jun 29. Available from: http://www.mhlw.go.jp/stf/shingi/2r9852000001u23a.html.
20. Uramoto H, Kabashima M, Yamazaki K, Kadota T, Narimatsu M, Iwashige A, et al. What do cancer chemotherapy outpatients want?: results of a questionnaire survey. Gan To Kagaku Ryoho. 2006; 33:1681–1683.
21. Jalali R, Dutta D, Kamble R, Gupta T, Munshi A, Sarin R, et al. Prospective assessment of activities of daily living using modified Barthel's Index in children and young adults with low-grade gliomas treated with stereotactic conformal radiotherapy. J Neurooncol. 2008; 90:321–328.
22. Gazzotti MR, Malheiros SM, Batan Alith M, Nascimento O, Santoro IL, Jardim JR, et al. Quality of life and physical limitations in primary brain tumor patients. Qual Life Res. 2011; 20:1639–1643.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download