Abstract
The standard treatment of advanced ovarian cancer is rapidly changing. As we begin to understand that epithelial ovarian cancer is a heterogeneous disease, our treatment strategies are evolving to include novel biologic drugs that specifically exploit altered pathways. Surgery remains an essential component in the treatment of ovarian cancer; however, the importance of surgical specialization and defining "optimal cytoreduction" as no visible residual disease has been further validated. Ongoing studies are defining the role of neoadjuvant chemotherapy in the upfront treatment of advanced ovarian cancer. In addition, clinical trials are evaluating intraperitoneal, dose dense, antiangiogenic drugs as well as targeted maintenance therapies which will establish new standards of care in the near future.
For many years the optimal treatment for women with advanced ovarian cancer has been surgical cytoreduction followed by intravenous platinum and taxane chemotherapy on an every three-week schedule. Recent clinical trials suggest that new treatment paradigms with different routes, dosing schedules and addition of targeted biologic therapies are replacing this old standard. In addition, new research suggests that ovarian, fallopian tube and peritoneal cancers may arise from a similar precursor, but histologic variants may require different treatment strategies.
A paradigm shift has recently occurred in our understanding of the pathologic origin of ovarian, fallopian tube and peritoneal cancers [1]. Many of the high grade serous tumors of the female pelvis are now thought to arise from the fallopian tube [1-5]. These type II cancers have fairly rapid progression and account for 60-70% of epithelial ovarian cancer [1]. Type I ovarian cancers include clear cell and endometrioid cancers which are thought to arise from endometriosis and mucinous tumors which are thought to arise from benign or low malignant potential (LMP) mucinous neoplasms [2,6]. Even grouped together, type I cancers account for only about 30% of ovarian cancer. These tumors tend to be slower growing and more likely to present in stage I, but also may be more resistant to chemotherapy when they present in advanced stages.
The more common high grade serous cancers, using the new nomenclature, are categorized as type II ovarian cancer. These cancers account for about 60-70% of what has been designated epithelial ovarian cancers, but in fact many of these high grade serous cancers are now known to arise from the distal fallopian tube [1-5]. Regardless of origin (tube, ovary, or peritoneum) these type II cancers have rapid progression and normally present in advanced stages.
Molecular profiling shows significant differences between high grade serous, low grade serous, mucinous, endometrioid, and clear cell cancers. High grade serous tumors have mutations in TP53 and have genetic instability [1-5]. High grade endometrioid tumors are similar to serous tumors but low grade endometrioid tumors often have mutations in the PI3KCA/AKT/PTEN and Wnt/CTNNB1/Tcf pathways [2]. Mucinous tumors like colorectal tumors often have KRAS mutations [2]. Low grade serous tumors often have mutations in KRAS or BRAF [2]. Better understanding of molecular differences between the types of cancer should lead to better treatment strategies that more specifically target or exploit the abnormalities in these pathways.
Research has shown that in the setting of advanced disease response rates to chemotherapy and survival is significantly different for the specific histologic types of cancer. In studies by Mackay et al. [7] (8,704 patients from 7 GCIG randomized trials) and Winter et al. [8] (1,895 women enrolled in Gynecologic Oncology Group [GOG] randomized trials) in which patients with all histologic types of advanced ovarian cancer were treated with taxane/platinum combinations, the serous and endometrioid cancers had the best survival, and clear cell and mucinous had a 2-4 fold increase in death. As we have come to understand, epithelial ovarian cancer is a very heterogeneous disease. Current clinical trials are incorporating this new information and we are beginning to use treatment protocols that are histologic specific. For example, in mucinous tumors the GOG is conducting a trial comparing the gastrointestinal (GI) regimen capecitabine and oxaliplatin +/- bevacizumab vs. paclitaxel and carboplatin +/- bevacizumab. In clear cell cancers, the GOG is evaluating the combination of paclitaxel, carboplatin and temsirolimus, an mTOR inhibitor which is Food Drug Administration (FDA) approved to treat renal cell carcinoma. In low grade serous tumors, AZD6244, a drug that blocks a protein MEK which has been shown to play a role in tumors with BRAF mutations, is also being investigated. Another successful targeted therapy has been poly (adenosine diphosphate, ADP)-ribose polymerase (PARP) inhibitors for high grade serous tumors. PARP inhibitors prevent repair of DNA damage. Because ovarian cancer cells with BRCA mutations, either germ line or somatic, also have limited ability to repair DNA damage the combination of PARP inhibition with BRCA mutation results in irreparable and lethal DNA damage. This was demonstrated clinically in a study of 65 women with high grade serous or undifferentiated ovarian cancer treated with the PARP inhibitor olaparib. Response rates of 41% were seen in women with BRCA1 or BRCA2 germline mutations but only 24% for those without germline mutations [9].
Surgery has always been the cornerstone in the treatment of ovarian cancer [10,11]. In most cases it is first required for diagnosis, then staging for early stage disease and cytoreduction in those with advanced stage disease. Approximately 70-80% of women with ovarian, tubal and peritoneal cancers present with advanced stage disease. Although there have never been any prospective randomized trials for cytoreduction, it has been shown in numerous retrospective studies to be one of the most important prognostic factors for survival [10-18]. Over the past decade the definition of "optimal cytoreduction" has changed from less than 1 cm to no visible residual disease [19-21]. Research by multiple investigators has shown that median OS in women with no residual disease will be 70 months or greater [18-21]. In a recent Cochrane analysis of the impact of residual disease on survival in women with advanced ovarian cancer, the hazard ratio for death was 2.2 (95% confidence interval [CI], 1.9 to 2.54) for women with less than 1 cm as compared to women with no residual disease [22]. Therefore, the goal of every cytoreductive procedure should be to debulk the cancer to no visible disease. In addition, several studies suggest that lymphadenectomy, especially in those who have all disease resected, may improve outcomes [18]. Finally, surgical specialization has been associated with higher rates of optimal cytoreduction, appropriate surgical care and survival [23-26]. Whenever possible, a gynecologic oncologist should be involved in the surgical management of all women with ovarian cancer. In general, with gynecologic oncology involvement approximately 60-70% of patients will be able to be optimally cytoreduced using the new definition of no visible residual disease. [12,17].
Neoadjuvant chemotherapy (NACT) is an alternative to primary cytoreduction. The goal is to use chemotherapy prior to surgery to reduce perioperative morbidity and mortality and increase the likelihood of a complete surgical cytoreduction [27]. A recent European Organisation for Research and Treatment of Cancer (EORTC) trial compared NACT vs. primary cytoreduction. Women with stage IIIC and IV epithelial ovarian, tubal and peritoneal cancer were randomized to primary debulking surgery (PDS) followed by six cycles of platin based chemotherapy vs. NACT with three cycles of platin based chemotherapy, surgery for cytoreduction and then three more cycles of chemotherapy. This study found that the NACT group had a significantly lower rate of complications, a higher rate of optimal cytoreduction to <1 cm (81% vs. 42%), but no difference in median overall survival (OS; 30 months NCAT vs. 29 months for PDS). This study has been criticized for several reasons. First, only 78% (PDS) and 88% (NACT) actually received a combination of platin and taxane based chemotherapy. In addition, in the PDS group only about 20% of patients were cytoreduced to no residual disease, which is considerably lower than what would be expected in centers of excellence [28]. Finally, median OS was only 30 months which is considerably less than the 60+ months expected with optimal cytoreduction followed by chemotherapy [19,27]. Views about NACT vary significantly between Society of Gynecologic Oncology (SGO) members and European Society of Gynecologic Oncology (ESGO) members. A survey of SGO members found the 82% felt there was not enough evidence to justify the use of NCAT [29]. In contrast, 70% of ESGO members felt there was sufficient evidence to recommend NCAT [30]. There are two other randomized trials that have completed enrollment and will provide additional information about the role of NACT. The first is the chemotherapy or upfront surgery (CHORUS) trial which has a similar design to the EORTC trial and is being conducted in the UK. The Japanese GOG (JGOG) is also conducting a trial comparing PDS followed by eight cycles of chemotherapy to four cycles of NCAT followed by surgery and four more cycles of chemotherapy.
Once patients with advanced stage ovarian, tubal and peritoneal cancer have undergone surgery the next choice is to decide which chemotherapy regimen to prescribe. In 1996 the GOG published the results of their landmark trial showing that patients who received cisplatin and paclitaxel had superior survival to those treated with cisplatin and cyclophosphamide [31]. This was confirmed in additional studies by EORTC [32], and since then platin and taxane have remained the standard for treating these cancers. Given the toxicity associated with the cisplatin/paclitaxel regimen, follow-up studies from GOG and Arbeitsgemeinschaft Gynäkologische Onkologie (AGO) compared paclitaxel in combination with cisplatin or carboplatin and found that the carboplatin combination was equally effective and was better tolerated than paclitaxel and cisplatin [33,34]. An additional trial (Scottish randomized trial in ovarian cancer, SCOTROC) confirmed that docetaxel and carboplatin was equally effective as carboplatin and paclitaxel. While there was more hematologic toxicity with docetaxel, there was less neurotoxicity [35]. Currently there is no role for adding a third agent to carboplatin and paclitaxel. Phase III trials have demonstrated no improvement in survival when additional drugs (topotecan, gemcitabine, or liposomaldoxorubicin) are added to the platin/taxane backbone [19,36]. In addition, high dose chemotherapy with stem cell transplant has been evaluated and found not to have any survival benefit [37]. Finally, the concept of maintenance chemotherapy has been the study of numerous trials. Other than a single GOG trial which found an improvement in progression-free survival (PFS) but not OS for 12 months of maintenance paclitaxel chemotherapy as compared to 3 months, no other studies have found that maintenance after front-line chemotherapy improves outcomes [11,38,39]. Maintenance with biologic agents such as anti-vascular endothelial growth factor (VEGF) or PARP inhibitors has also shown improvement in PFS but not OS [40-42].
The most significant advances in improving survival with chemotherapy have been from changing the route of daily delivery and switching to a dose dense schedule of paclitaxel. In 2005 the GOG published results of GOG 172 (intravenous [IV] paclitaxel IV cisplatin vs. IV paclitaxel intraperitoneal [IP] cisplatin IP paclitaxel) [27]. In this study women who were optimally cytoreduced to less than 1 cm were randomized to one of the two groups. The OS for the IP group was 65.6 months compared to 49.7 months for the IV group. The IP arm was associated with increased toxicity and only 42% of patients in the IP arm were able to complete all 6 cycles of treatment, but quality of life was similar in both groups at 6 months after completion of treatment. Additional clinical trials have also shown improved overall survival with IP treatment [43-45], and the use of IP chemotherapy was advocated in a National Cancer Institute Clinical Alert in 2006 [46].
The other treatment strategy which has been shown to improve OS is dose dense administration of paclitaxel [47]. The JGOG randomized women with stage II-IV ovarian cancer to receive every three week paclitaxel or weekly paclitaxel, with both regimens including carboplatin administered every three weeks. This study found a significant improvement in both PFS and OS, with 5-year survival of 58.7% and 51.1% for dose dense and standard treatment arms respectively. Improvement in survival was seen for all patient subgroups except for women with clear cell carcinoma. Toxicity was similar in both groups with the exception of more anemia and transfusions in the dose dense arm. In addition, both GOG 262 and International Collaborative Ovarian Neoplasm (ICON) 8 are conducting trials to confirm the JGOG findings and preliminary results should be reported soon.
Clinical trials are now underway to directly compare IP chemotherapy and dose dense paclitaxel. GOG 252, which has recently completed accrual, is evaluating this in women after an optimal cytoreduction. This study has three treatment arms: arm 1, IV carboplatin with IV dose dense paclitaxel; arm 2, IP carboplatin with IV dose dense paclitaxel; and arm 3, IV paclitaxel IP cisplatin and day 8 IP paclitaxel (GOG 172). In all 3 arms bevacizumab, 15 mg/m2, with cycles 2-6 followed by bevacizumab maintenance for an additional 18 months. In the JGOG iPocc trial, carboplatin IV with dose dense paclitaxel is being compared with carboplatin IP with IV dose dense paclitaxel. These trials will be very important in determining what the optimal standard of care should be for these optimally cytoreduced patients.
Another important advance in the treatment of ovarian cancer is the use of agents to inhibit tumor angiogenesis [40,41,48]. Bevacizumab, a monoclonal antibody directed to vascular endothelial growth factor VEGF has been shown to have significant single agent activity in women with recurrent epithelial cancer. And two large randomized studies, GOG 218 and ICON 7, have now been conducted using bevacizumab with chemotherapy in newly diagnosed patients. In the GOG trial [40], women with advanced stage ovarian cancer were randomized to arm 1, carboplatin and paclitaxel every three weeks with placebo; arm 2, carboplatin paclitaxel bevacizumab (cycles 2-6); arm 3, carboplatin paclitaxel with bevacizumab (cycles 2-6) followed by 15 additional cycles of bevacizumab maintenance. Bevacizumab was given at 15 mg/kg every 3 weeks. This study found a significant improvement in PFS of 3.8 months, but only for the group that received bevacizumab with chemotherapy and maintenance. Overall survival between the three groups was not significantly different. In a similar study, ICON 7 [41], women with ovarian cancer stage I-IV were randomized to receive standard carboplatin/paclitaxel or carboplatin/paclitaxel with bevacizumab every 3 weeks for 6 cycles and then bevacizumab maintenance for an additional 12 cycles. The bevacizumab in this study was dosed at 7.5 mg/kg (50% less than the GOG study). In this study, PFS was significantly longer in the bevacizumab arm, 24 months vs. 22 months, but there was no difference in OS. Subgroup analysis of women with suboptimal stage IIIC and IV disease revealed a significant improvement in PFS, 18 months vs. 14 months and OS 37 months vs. 29 months. While these latter findings require confirmation, it seems that given these results those patients at highest risk for progression may derive the most benefit from bevacizumab given with chemotherapy followed by bevacizumab maintenance. One interesting difference between the GOG study conducted in the United States and the ICON 7 study conducted in Europe was that bevacizumab was available and covered by many insurance carries in the US but not in Europe. So crossover may have confounded the results in the US trial, thus obscuring the expected benefit with bevacizumab.
Current clinical trials are evaluating extended maintenance schedules for bevacizumab as well as other antiangiogenic agents. The Trinova-3 study is comparing carboplatin and paclitaxel on an every 3 week schedule given with placebo or AMG 386 (Trebananib), followed by 18 months of AMG 386 or placebo. AMG 386 inhibits angiogenesis by sequestering angiopoietin 1 and 2, thus preventing their interaction with the Tie 2 receptor on endothelial cells. The LUME-OVAR 1 trial is comparing carboplatin and paclitaxel with BIBF1120 (nintedanib) vs. placebo in women with advanced ovarian cancer. In this trial, the BIBF1120 will be continued until progression, adverse event, or for a maximum of 120 weeks after randomization. BIBF1120 is a tyrosine kinase inhibitor which targets vascular endothelial growth factor receptor (VEGFR), platelet-derived growth factor receptor (PDGFR), and fibroblast growth factor receptor (FGFR). The AGO-OVAR16/VEG110655 trial is a study enrolling women with ovarian cancer who have completed first line chemotherapy without progression. Patients are randomized to placebo or up to 24 months of Pazopanib. Pazopanib is also a tyrosine kinase inhibitor which targets VEGFR, PDGFR, c-kit, and FGFR. These studies should help us better define the role of antiangiogenic treatments in both upfront and maintenance therapy for women with advanced ovarian cancer.
In the setting of recurrent disease there are several important trials addressing the role of secondary cytoreduction. As a general rule, secondary cytoreduction is only appropriate for women with recurrence more than six months from completing chemotherapy. GOG 213 is randomizing women with platin sensitive recurrence who are surgical candidates to cytoreductive surgery or no surgery. A second randomization is also done to allow comparison of carboplatin and paclitaxel either with or without bevacizumab, plus bevacizumab maintenance until progression in the group randomized to receive bevacizumab. In the AGO-OVAR desktop III trial women with platinum sensitive recurrent disease are also being randomized to cytoreductive surgery followed by platinum based therapy. Both of these trials, when completed, will help define the role of secondary cytoreduction in this population of patients.
In women with platinum sensitive recurrent disease, ICON 4 [49], AGO-OVAR-2.5 [50], and CALYPSO [51] have all shown the value of platinum doublets. These trials combined carboplatin with paclitaxel, gemcitabine or liposomal doxorubicin, respectively. Which couplet to use in clinical practice is usually influenced by which schedule is most convenient as well as pre-existing and expected toxicities. Overall response rates will be approximately 70% for any of these three couplets. Recently the use of bevacizumab has been evaluated in this population of patients. The OCEANS trial randomized women with first recurrence after more than six months from frontline chemotherapy to carboplatin, gemcitabine and placebo vs. carboplatin, gemcitabine and bevacizumab with bevacizumab maintenance until progression or adverse event [48,52]. The PFS for those who received the placebo was 8.4 months and 12.4 months for bevacizumab, with a hazard ratio of 0.484 (95% CI, 0.388 to 0.605). No patient on bevacizumab developed a GI perforation. Despite the significant improvement in PFS this did not translate into improvement in OS between the groups. But two observations still support the use of bevacizumab in this population. First, was the median OS for both groups was 33 months from enrollment, which is the longest OS reported for any clinical trial for this population of patients. Second, this finding probably relates to crossover to bevacizumab in the placebo group plus the fact that 55% of patients received at least three additional lines of chemotherapy after progression on study, hence obscuring the possible benefit from bevacizumab.
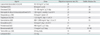
In the setting of platinum resistant disease (defined as relapse less than 6 months from previous platinum therapy), single agent therapy is generally recommended [53-65]. Table 1 shows the most active agents. In contrast with platin-sensitive recurrences, combination chemotherapy has been shown to increase toxicity without improvement in response rate of PFS/OS. However, there may be a role for combining one chemotherapy drug with bevacizumab. In 2012 results of the AURELIA trial were reported to American Society of Clinical Oncology (ASCO) and European Society for Medical Oncology (ESMO) [66,67]. In this study women with platinum resistant ovarian cancer were randomized to standard chemotherapy with or without bevacizumab. Investigators could choose weekly paclitaxel, weekly topotecan or liposomal doxorubicin. Preliminary results found that addition of bevacizumab to all drugs significantly improved the PFS. Overall, the hazard ratio for the bevacizumab treated women was 0.48. This risk of grade 2 GI perforation, fistula, or abscess was less than 3%. A subset analysis based on choice of chemotherapy found that PFS for the 3 chemotherapies with and without bevacizumab respectively was paclitaxel 10 months vs. 4 months, topotecan 6 months vs. 2 months, and liposomal doxorubicin 5 months vs. 4 months. Each of these findings was statistically significant. The impact of bevacizumab on OS in this population is not yet reported.
Substantial progress is being made in the diagnosis and treatment of ovarian, tubal, and peritoneal cancers. We are beginning to understand the molecular heterogeneity of these tumors and how we can use this information to produce less toxic and more targeted therapies. Historical treatment paradigms in ovarian cancer are being challenged and are evolving. In 2013, surgery does remain the cornerstone of diagnosis and treatment, but ongoing studies will better define when to use neoadjuvant chemotherapy. We also expect clinical trials to guide optimal use of intraperitoneal, dose dense, antiangiogenic therapies and targeted maintenance therapies in both the up front and recurrent disease setting. Finally, there are a large number of clinical trials being conducted by cooperative groups and single institutions that are targeting the underlying molecular biology of ovarian cancer. It is likely in the near future that histology will be less important than knowing the molecular alterations in various pathways, which in turn will predict response to certain types of drugs. The promise of personalized medicine is rapidly becoming a reality for the treatment of ovarian cancer and will need to be a factor in future clinical trials.
References
1. Kurman RJ, Shih IeM. The origin and pathogenesis of epithelial ovarian cancer: a proposed unifying theory. Am J Surg Pathol. 2010. 34:433–443.
2. Sfakianos GP, Secord AA, Shih lM. Karlan BY, Bristow RE, Li AJ, editors. Epithelial ovarian cancers: low malignant potential and non-serous ovarian histologies. Gynecologic oncology clinical practice & surgical atlas. 2012. New York: McGraw Hill Medical;237–256.
3. Crum CP, McKeon FD, Xian W. The oviduct and ovarian cancer: causality, clinical implications, and "targeted prevention". Clin Obstet Gynecol. 2012. 55:24–35.
4. Kuhn E, Kurman RJ, Vang R, Sehdev AS, Han G, Soslow R, et al. TP53 mutations in serous tubal intraepithelial carcinoma and concurrent pelvic high-grade serous carcinoma: evidence supporting the clonal relationship of the two lesions. J Pathol. 2012. 226:421–426.
5. Vang R, Shih IeM, Kurman RJ. Fallopian tube precursors of ovarian low- and high-grade serous neoplasms. Histopathology. 2013. 62:44–58.
6. Ayhan A, Mao TL, Seckin T, Wu CH, Guan B, Ogawa H, et al. Loss of ARID1A expression is an early molecular event in tumor progression from ovarian endometriotic cyst to clear cell and endometrioid carcinoma. Int J Gynecol Cancer. 2012. 22:1310–1315.
7. Mackay HJ, Brady MF, Oza AM, Reuss A, Pujade-Lauraine E, Swart AM, et al. Prognostic relevance of uncommon ovarian histology in women with stage III/IV epithelial ovarian cancer. Int J Gynecol Cancer. 2010. 20:945–952.
8. Winter WE 3rd, Maxwell GL, Tian C, Carlson JW, Ozols RF, Rose PG, et al. Prognostic factors for stage III epithelial ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol. 2007. 25:3621–3627.
9. Gelmon KA, Tischkowitz M, Mackay H, Swenerton K, Robidoux A, Tonkin K, et al. Olaparib in patients with recurrent high-grade serous or poorly differentiated ovarian carcinoma or triple-negative breast cancer: a phase 2, multicentre, open-label, non-randomised study. Lancet Oncol. 2011. 12:852–861.
10. Griffiths CT. Surgical resection of tumor bulk in the primary treatment of ovarian carcinoma. Natl Cancer Inst Monogr. 1975. 42:101–104.
11. Cohn DE, Alvarez RD. Karlan BY, Bristow RE, Li AJ, editors. High-grade serous carcinomas of the ovary, fallopian tube, and peritoneum. Gynecologic oncology clinical practice & surgical atlas. 2012. New York: McGraw Hill Medical;217–236.
12. Harter P, Muallem ZM, Buhrmann C, Lorenz D, Kaub C, Hils R, et al. Impact of a structured quality management program on surgical outcome in primary advanced ovarian cancer. Gynecol Oncol. 2011. 121:615–619.
13. Hoskins WJ, McGuire WP, Brady MF, Homesley HD, Creasman WT, Berman M, et al. The effect of diameter of largest residual disease on survival after primary cytoreductive surgery in patients with suboptimal residual epithelial ovarian carcinoma. Am J Obstet Gynecol. 1994. 170:974–979.
14. Bristow RE, Tomacruz RS, Armstrong DK, Trimble EL, Montz FJ. Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a meta-analysis. J Clin Oncol. 2002. 20:1248–1259.
15. Chi DS, Eisenhauer EL, Lang J, Huh J, Haddad L, Abu-Rustum NR, et al. What is the optimal goal of primary cytoreductive surgery for bulky stage IIIC epithelial ovarian carcinoma (EOC)? Gynecol Oncol. 2006. 103:559–564.
16. Eisenkop SM, Spirtos NM, Lin WC. "Optimal" cytoreduction for advanced epithelial ovarian cancer: a commentary. Gynecol Oncol. 2006. 103:329–335.
17. Chi DS, Franklin CC, Levine DA, Akselrod F, Sabbatini P, Jarnagin WR, et al. Improved optimal cytoreduction rates for stages IIIC and IV epithelial ovarian, fallopian tube, and primary peritoneal cancer: a change in surgical approach. Gynecol Oncol. 2004. 94:650–654.
18. du Bois A, Reuss A, Harter P, Pujade-Lauraine E, Ray-Coquard I, Pfisterer J, et al. Potential role of lymphadenectomy in advanced ovarian cancer: a combined exploratory analysis of three prospectively randomized phase III multicenter trials. J Clin Oncol. 2010. 28:1733–1739.
19. Bookman MA, Brady MF, McGuire WP, Harper PG, Alberts DS, Friedlander M, et al. Evaluation of new platinum-based treatment regimens in advanced-stage ovarian cancer: a Phase III Trial of the Gynecologic Cancer Intergroup. J Clin Oncol. 2009. 27:1419–1425.
20. Aletti GD, Dowdy SC, Gostout BS, Jones MB, Stanhope CR, Wilson TO, et al. Aggressive surgical effort and improved survival in advanced-stage ovarian cancer. Obstet Gynecol. 2006. 107:77–85.
21. Chang SJ, Bristow RE, Ryu HS. Impact of complete cytoreduction leaving no gross residual disease associated with radical cytoreductive surgical procedures on survival in advanced ovarian cancer. Ann Surg Oncol. 2012. 19:4059–4067.
22. Elattar A, Bryant A, Winter-Roach BA, Hatem M, Naik R. Optimal primary surgical treatment for advanced epithelial ovarian cancer. Cochrane Database Syst Rev. 2011. (8):CD007565.
23. Goff BA, Matthews BJ, Larson EH, Andrilla CH, Wynn M, Lishner DM, et al. Predictors of comprehensive surgical treatment in patients with ovarian cancer. Cancer. 2007. 109:2031–2042.
24. Giede KC, Kieser K, Dodge J, Rosen B. Who should operate on patients with ovarian cancer? An evidence-based review. Gynecol Oncol. 2005. 99:447–461.
25. Engelen MJ, Kos HE, Willemse PH, Aalders JG, de Vries EG, Schaapveld M, et al. Surgery by consultant gynecologic oncologists improves survival in patients with ovarian carcinoma. Cancer. 2006. 106:589–598.
26. Vergote I, Trope CG, Amant F, Kristensen GB, Ehlen T, Johnson N, et al. Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. N Engl J Med. 2010. 363:943–953.
27. Armstrong DK, Bundy B, Wenzel L, Huang HQ, Baergen R, Lele S, et al. Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med. 2006. 354:34–43.
28. Chi DS, Musa F, Dao F, Zivanovic O, Sonoda Y, Leitao MM, et al. An analysis of patients with bulky advanced stage ovarian, tubal, and peritoneal carcinoma treated with primary debulking surgery (PDS) during an identical time period as the randomized EORTC-NCIC trial of PDS vs neoadjuvant chemotherapy (NACT). Gynecol Oncol. 2012. 124:10–14.
29. Dewdney SB, Rimel BJ, Reinhart AJ, Kizer NT, Brooks RA, Massad LS, et al. The role of neoadjuvant chemotherapy in the management of patients with advanced stage ovarian cancer: survey results from members of the Society of Gynecologic Oncologists. Gynecol Oncol. 2010. 119:18–21.
30. Cornelis S, Van Calster B, Amant F, Leunen K, van der Zee AG, Vergote I. Role of neoadjuvant chemotherapy in the management of stage IIIC-IV ovarian cancer: survey results from the members of the European Society of Gynecological Oncology. Int J Gynecol Cancer. 2012. 22:407–416.
31. McGuire WP, Hoskins WJ, Brady MF, Kucera PR, Partridge EE, Look KY, et al. Cyclophosphamide and cisplatin compared with paclitaxel and cisplatin in patients with stage III and stage IV ovarian cancer. N Engl J Med. 1996. 334:1–6.
32. Piccart MJ, Bertelsen K, James K, Cassidy J, Mangioni C, Simonsen E, et al. Randomized intergroup trial of cisplatin-paclitaxel versus cisplatin-cyclophosphamide in women with advanced epithelial ovarian cancer: three-year results. J Natl Cancer Inst. 2000. 92:699–708.
33. Ozols RF, Bundy BN, Greer BE, Fowler JM, Clarke-Pearson D, Burger RA, et al. Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a Gynecologic Oncology Group study. J Clin Oncol. 2003. 21:3194–3200.
34. du Bois A, Luck HJ, Meier W, Adams HP, Mobus V, Costa S, et al. A randomized clinical trial of cisplatin/paclitaxel versus carboplatin/paclitaxel as first-line treatment of ovarian cancer. J Natl Cancer Inst. 2003. 95:1320–1329.
35. Vasey PA, Jayson GC, Gordon A, Gabra H, Coleman R, Atkinson R, et al. Phase III randomized trial of docetaxel-carboplatin versus paclitaxel-carboplatin as first-line chemotherapy for ovarian carcinoma. J Natl Cancer Inst. 2004. 96:1682–1691.
36. Bookman MA. The addition of new drugs to standard therapy in the first-line treatment of ovarian cancer. Ann Oncol. 2010. 21:Suppl 7. vii211–vii217.
37. Mobus V, Wandt H, Frickhofen N, Bengala C, Champion K, Kimmig R, et al. Phase III trial of high-dose sequential chemotherapy with peripheral blood stem cell support compared with standard dose chemotherapy for first-line treatment of advanced ovarian cancer: intergroup trial of the AGO-Ovar/AIO and EBMT. J Clin Oncol. 2007. 25:4187–4193.
38. Markman M, Liu PY, Wilczynski S, Monk B, Copeland LJ, Alvarez RD, et al. Phase III randomized trial of 12 versus 3 months of maintenance paclitaxel in patients with advanced ovarian cancer after complete response to platinum and paclitaxel-based chemotherapy: a Southwest Oncology Group and Gynecologic Oncology Group trial. J Clin Oncol. 2003. 21:2460–2465.
39. Markman M, Liu PY, Moon J, Monk BJ, Copeland L, Wilczynski S, et al. Impact on survival of 12 versus 3 monthly cycles of paclitaxel (175 mg/m2) administered to patients with advanced ovarian cancer who attained a complete response to primary platinum-paclitaxel: follow-up of a Southwest Oncology Group and Gynecologic Oncology Group phase 3 trial. Gynecol Oncol. 2009. 114:195–198.
40. Burger RA, Brady MF, Bookman MA, Fleming GF, Monk BJ, Huang H, et al. Incorporation of bevacizumab in the primary treatment of ovarian cancer. N Engl J Med. 2011. 365:2473–2483.
41. Perren TJ, Swart AM, Pfisterer J, Ledermann JA, Pujade-Lauraine E, Kristensen G, et al. A phase 3 trial of bevacizumab in ovarian cancer. N Engl J Med. 2011. 365:2484–2496.
42. Ledermann J, Harter P, Gourley C, Friedlander M, Vergote I, Rustin G, et al. Olaparib maintenance therapy in platinum-sensitive relapsed ovarian cancer. N Engl J Med. 2012. 366:1382–1392.
43. Alberts DS, Liu PY, Hannigan EV, O'Toole R, Williams SD, Young JA, et al. Intraperitoneal cisplatin plus intravenous cyclophosphamide versus intravenous cisplatin plus intravenous cyclophosphamide for stage III ovarian cancer. N Engl J Med. 1996. 335:1950–1955.
44. Markman M, Bundy BN, Alberts DS, Fowler JM, Clark-Pearson DL, Carson LF, et al. Phase III trial of standard-dose intravenous cisplatin plus paclitaxel versus moderately high-dose carboplatin followed by intravenous paclitaxel and intraperitoneal cisplatin in small-volume stage III ovarian carcinoma: an intergroup study of the Gynecologic Oncology Group, Southwestern Oncology Group, and Eastern Cooperative Oncology Group. J Clin Oncol. 2001. 19:1001–1007.
45. Nagao S, Fujiwara K, Ohishi R, Nakanishi Y, Iwasa N, Shimizu M, et al. Combination chemotherapy of intraperitoneal carboplatin and intravenous paclitaxel in suboptimally debulked epithelial ovarian cancer. Int J Gynecol Cancer. 2008. 18:1210–1214.
46. National Cancer Institute. NCI clinical announcement: intraperitoneal chemotherapy for ovarian cancer [Internet]. 2006. cited 2012 Dec 30. National Cancer Institute;Available from: http://ctep.cancer.gov/highlights/docs/clin_annc_010506.pdf.
47. Katsumata N, Yasuda M, Takahashi F, Isonishi S, Jobo T, Aoki D, et al. Dose-dense paclitaxel once a week in combination with carboplatin every 3 weeks for advanced ovarian cancer: a phase 3, open-label, randomised controlled trial. Lancet. 2009. 374:1331–1338.
48. Aghajanian C, Blank S, Goff B, et al. Results from a 2nd interim OS analysis in OCEANS, a randomized phase 3 trial of gemcitabine (G), carboplatin (C) and bevacizumab (BV) followed by BV to disease progression in patients with platinum-sensitive recurrent epithelial ovarian (OC), primary peritoneal (PPC), or fallopian tube cancer (FTC). In : The 2012 Society of Gynecologic Oncologists Annual Meeting; Abst 2289.
49. Parmar MK, Ledermann JA, Colombo N, du Bois A, Delaloye JF, Kristensen GB, et al. Paclitaxel plus platinum-based chemotherapy versus conventional platinum-based chemotherapy in women with relapsed ovarian cancer: the ICON4/AGO-OVAR-2.2 trial. Lancet. 2003. 361:2099–2106.
50. Pfisterer J, Plante M, Vergote I, du Bois A, Hirte H, Lacave AJ, et al. Gemcitabine plus carboplatin compared with carboplatin in patients with platinum-sensitive recurrent ovarian cancer: an intergroup trial of the AGO-OVAR, the NCIC CTG, and the EORTC GCG. J Clin Oncol. 2006. 24:4699–4707.
51. Pujade-Lauraine E, Wagner U, Aavall-Lundqvist E, Gebski V, Heywood M, Vasey PA, et al. Pegylated liposomal Doxorubicin and Carboplatin compared with Paclitaxel and Carboplatin for patients with platinum-sensitive ovarian cancer in late relapse. J Clin Oncol. 2010. 28:3323–3329.
52. Aghajanian C, Blank SV, Goff BA, Judson PL, Teneriello MG, Husain A, et al. OCEANS: a randomized, double-blind, placebo-controlled phase III trial of chemotherapy with or without bevacizumab in patients with platinum-sensitive recurrent epithelial ovarian, primary peritoneal, or fallopian tube cancer. J Clin Oncol. 2012. 30:2039–2045.
53. Gordon AN, Tonda M, Sun S, Rackoff W. Doxil Study 30-49 Investigators. Long-term survival advantage for women treated with pegylated liposomal doxorubicin compared with topotecan in a phase 3 randomized study of recurrent and refractory epithelial ovarian cancer. Gynecol Oncol. 2004. 95:1–8.
54. Markman M, Kennedy A, Webster K, Peterson G, Kulp B, Belinson J. Phase 2 trial of liposomal doxorubicin (40 mg/m(2)) in platinum/paclitaxel-refractory ovarian and fallopian tube cancers and primary carcinoma of the peritoneum. Gynecol Oncol. 2000. 78:369–372.
55. Gynecologic Oncology Group. Markman M, Blessing J, Rubin SC, Connor J, Hanjani P, et al. Phase II trial of weekly paclitaxel (80 mg/m2) in platinum and paclitaxel-resistant ovarian and primary peritoneal cancers: a Gynecologic Oncology Group study. Gynecol Oncol. 2006. 101:436–440.
56. Verschraegen CF, Sittisomwong T, Kudelka AP, Guedes Ed, Steger M, Nelson-Taylor T, et al. Docetaxel for patients with paclitaxel-resistant Müllerian carcinoma. J Clin Oncol. 2000. 18:2733–2739.
57. Coleman RL, Brady WE, McMeekin DS, Rose PG, Soper JT, Lentz SS, et al. A phase II evaluation of nanoparticle, albumin-bound (nab) paclitaxel in the treatment of recurrent or persistent platinum-resistant ovarian, fallopian tube, or primary peritoneal cancer: a Gynecologic Oncology Group study. Gynecol Oncol. 2011. 122:111–115.
58. Rose PG, Blessing JA, Mayer AR, Homesley HD. Prolonged oral etoposide as second-line therapy for platinum-resistant and platinum-sensitive ovarian carcinoma: a Gynecologic Oncology Group study. J Clin Oncol. 1998. 16:405–410.
59. Sehouli J, Stengel D, Harter P, Kurzeder C, Belau A, Bogenrieder T, et al. Topotecan weekly versus conventional 5-day schedule in patients with platinum-resistant ovarian cancer: a randomized multicenter phase II trial of the North-Eastern German Society of Gynecological Oncology Ovarian Cancer Study Group. J Clin Oncol. 2011. 29:242–248.
60. Mutch DG, Orlando M, Goss T, Teneriello MG, Gordon AN, McMeekin SD, et al. Randomized phase III trial of gemcitabine compared with pegylated liposomal doxorubicin in patients with platinum-resistant ovarian cancer. J Clin Oncol. 2007. 25:2811–2818.
61. Sorensen P, Høyer M, Jakobsen A, Malmstrom H, Havsteen H, Bertelsen K. Phase II study of vinorelbine in the treatment of platinum-resistant ovarian carcinoma. Gynecol Oncol. 2001. 81:58–62.
62. Miller DS, Blessing JA, Krasner CN, Mannel RS, Hanjani P, Pearl ML, et al. Phase II evaluation of pemetrexed in the treatment of recurrent or persistent platinum-resistant ovarian or primary peritoneal carcinoma: a study of the Gynecologic Oncology Group. J Clin Oncol. 2009. 27:2686–2691.
63. Cannistra SA, Matulonis UA, Penson RT, Hambleton J, Dupont J, Mackey H, et al. Phase II study of bevacizumab in patients with platinum-resistant ovarian cancer or peritoneal serous cancer. J Clin Oncol. 2007. 25:5180–5186.
64. Williams CJ. Tamoxifen for relapse of ovarian cancer. Cochrane Database Syst Rev. 2001. (1):CD001034.
65. Smyth JF, Gourley C, Walker G, MacKean MJ, Stevenson A, Williams AR, et al. Antiestrogen therapy is active in selected ovarian cancer cases: the use of letrozole in estrogen receptor-positive patients. Clin Cancer Res. 2007. 13:3617–3622.
66. Pujade-Lauraine E, Hilpert F, Weber B, Reuss A, Poveda A, Kristensen G, et al. AURELIA: a randomized phase III trial evaluating bevacizumab (BEV) plus chemotherapy (CT) for platinum (PT)-resistant recurrent ovarian cancer (OC). J Clin Oncol. 2012. 30:abstr LBA 5002.
67. Poveda AM, Selle F, Hilpert F, Reuss A, Pasic A, Savarese A, et al. Weekly paclitaxel (PAC), pegylated liposomal doxorubicin (PLD) or topotecan (TOP) ± bevacizumab (BEV) in platinum (PT)-resistant recurrent ovarian cancer (OC): analysis by chemotherapy (CT) cohort in the GCIG AURELIA randomised phase III trial. Ann Oncol. 2012. 23:Suppl 9. LBA26.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download