Abstract
Objective
The aim of this study is to determine the knowledge of the women living in the eastern region of Turkey about human papillomavirus (HPV) and cervix cancer and their approaches to HPV vaccine.
Methods
The questionnaire forms were distributed to 1,052 patients who applied to the Gynecology Department of Elazig Training and Research Hospital. The subjects were recruited from the general gynecology outpatient clinic of the hospital. The patients from sexually transmitted disease and oncology outpatient clinics were not included in the study. The information about 945 women who completely filled in the questionnaire form was included into the study. The questions set forth in the questionnaire form consisting of 20 questions were prepared by taking the studies previously performed as model.
Results
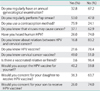
Ninety-five percent of the women were married and 83.5% were housewives (unemployed). Thirteen percent of the women were illiterate, only 12% were graduated from university. Seventy-four percent of the women did not hear about HPV, 78.4% did not know about HPV vaccine, 63% did not know about the fact that some viruses cause cancer, and 83% did not know about the relation between HPV and cervix cancer. According to the multivariate analysis, free-of-charge vaccination, vaccinated relatives or friends, graduation from university and being under the age of 25 predict to accept the vaccine for themselves.
Human papillomavirus (HPV) is one of the most frequent sexually transmitted diseases in both men and women throughout the world. It is known as the most frequent viral sexually transmitted diseases (STDs) in the USA. Since it is not obligatory to notify HPV, its current incidence and prevalence are unknown [1,2]. HPV carries on being an important factor for cervical cancer and the frequency of infection carries on increasing rapidly. Cervix cancer is frequently the most common cancer in the developing countries and forms 25% of the women's cancers [3]. Cervical cancer follows the breast cancer in cancer deaths worldwide [4]. It was notified that 1,500 new cervical cancer cases are added every year in the statistics of the Ministry of Health of the Republic of Turkey [5].
Although the incidence of HPV infection is not exactly known in Turkey, Inal et al. [6] informed in a study they performed that the prevalence of HPV infection is 2-7%. The use of HPV vaccine in protection against genital warts and preinvasive and invasive cervical cancers was approved in the USA and Europe since 2006 [7]. In Turkey, however, there are used two different vaccines since 2007.
In our country, the vaccine is recommended by the Ministry of Health, but not paid by the government and private health insurances. The vaccine is recommended in the age group of 9-26 years all around the world. In our country, the parents take the decision on the vaccination of preadolescents and adolescents. For this reason, the knowledge levels of parents and young women about the vaccine, cervical cancer and HPV are highly important in the expansion of the vaccination.
The purpose of this study is to determine the knowledge of the women living in the eastern region of Turkey about HPV and cervix cancer and their approaches to HPV vaccine.
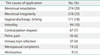
This study was carried out by the cooperation of Elazıg Research and Education Hospital and Zekai Tahir Burak Women's Health Research and Education Hospital. The questionnaire forms were prepared by the Oncology Clinic of Zekai Tahir Burak Women's Hospital. Ethics approval was obtained from the local research ethics committee prior to the study. The questionnaire forms were distributed to 1,052 patients who applied to the gynecology department of Elazig Training and Research Hospital for any reason between the dates of January-April 2010. The subjects were recruited from the general gynecology outpatient clinic of the hospital. The patients from STD and oncology outpatient clinics were not included in the study. The women were encouraged to fill in the forms in the waiting room. For those patients who are illiterate, the questions were read and the answers were marked by the secretary. All forms filled in were placed into a box in the secretariat. The information about 945 women who completely filled in the questionnaire form was included into the study.
The questions set forth in the questionnaire form consisting of 20 questions were prepared by taking the studies previously performed as model. The questionnaire form was composed of 3 main headings: 1) demographical data (Table 1), 2) knowledge of women about HPV and the relation between HPV and cervix cancer, and 3) attitude of women against HPV vaccine (Table 2).
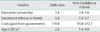
Data analysis was performed by using SPSS ver. 11.5 (SPSS Inc., Chicago, IL, USA). While, continuous data were expressed as mean±SD, otherwise, number of cases and percentages were used for categorical data. Categorical data were analyzed by Pearson chi-square test or univariate logistic regression analyses, where applicable. Multiple backward linear regression and logistic regression analyses were used for determining the predictors which mostly affected on dependent factors (e.g., acceptance HPV vaccine for her or children). Any variable whose univariate test had a p-value of < 0.25 was accepted as a candidate for the multivariable model along with all variables of known clinical importance. Odds ratio and 95% confidence intervals for each variables were also calculated. A p-value of less than 0.05 was considered statistically significant.
The mean age of the patients was 34.3±8.8 years (range, 18 to 66 years). Their mean parity was 2.3±1.5 (range, 0 to 9). Among them, 95% of the women were married and 83.5% were housewives (unemployed). The most frequently used contraception method was intra-uterine device (32.4%), where 20% of the women do not use any contraception method. Thirteen percent of the women were illiterate, only 12% were graduated from university. Fifty-three percent of the women had undergone regular gynecologic examination and cervicovaginal smear. Seventy-four percent of the women did not hear about HPV, 78.4% did not know about HPV vaccine, 63% did not know about the fact that some viruses cause cancer, and 83% did not know about the relation between HPV and cervical cancer. However, when they were asked whether they knew about the cervical cancer vaccine, 49% of the patients indicated that they knew. Forty point two percent of the patients accepted HPV vaccine for themselves, 36.3% for their daughters and 26% for their sons. Fifty-nine percent of the patients who accepted HPV vaccine were under the age of 35. Fifty percent of the women under the age of 25 accepted HPV vaccine. Eighty-eight percent of the women who did not accept HPV vaccine were unemployed. Fifty five point five percent of the employed women accepted the vaccine for themselves. For nulliparous women, the rate of accepting the vaccine for themselves was 3 times more than the women giving birth. Ninty nine point nine percent of the women whose education level is under university rejected HPV vaccine. Only for the women who were graduated from university, the rate of accepting HPV vaccine was more than the rate of rejecting it. Being graduated from university increased the acceptance of HPV vaccine 3.4 times more than being illiterate. Forty eight point nine percent of the women who accepted HPV vaccine had already undergone Pap smear and 29.4% undergone regular gynecological examination. Approximately 6% of the women who accepted HPV vaccine had vaccinated people around them. Ninty two point four percent of the women who accepted HPV vaccine desired to be vaccinated if it would be free-of-charge and this rate decreased to approximately half (49.5%) when they had to pay the vaccination charge. Twenty-two percent of the women who accepted HPV vaccine for their daughters were under the age of 25 and 20% were graduated from university. Only for these two parameters, the number of those who accepted HPV vaccine for their daughters was more than the half of those who did not accept. For all of the parameters, the number of those who did not accept HPV vaccine for their sons was more than that of those who accepted. Eighteen percent of the group under the age of 25 was graduated from university. Fifty eight point eight percent of the employed women were graduated from university.
According to the multivariate analysis, free-of-charge vaccination, vaccinated relatives or friends, graduation from university and being under the age of 25 predict to accept the vaccine for themselves (Table 3).
HPV is one of the most frequent sexually transmitted infections [8]. The relation of oncogenic genotypes with invasive and pre-invasive cervix cancer was finally determined [9]. For this reason, the prevention of HPV and the reduction of cervical cancers have come into prominence. After the molecular structure of HPV was identified, HPV vaccine was developed and introduced into the market.
There is lack of information about the adoption and acceptability
of HPV vaccine all around the world due to the reason that this vaccine is new. For this reason, questionnaire studies concerning HPV vaccine were carried out in the communities of various countries [10-16]. In our country, one of the studies that were performed with regard to this matter is Ankara-centered and included socio-economically developed 4 provinces. The other study, however, was Istanbul-centered and included 2 provinces [11,15]. As Turkey is a cosmopolite country, we carried out this study in an underdeveloped province in terms of socio-economy from the eastern region of Turkey in consideration of that these studies performed in developed provinces would not reflect the whole of Turkey.
The results of 2 studies performed in Turkey were similar to the results of the studies performed in other developed countries. In these studies, the rate of knowing about HPV was 45% [10], 40% [16], 89% [17] whereas this rate was 26% in our study. The rate of knowing the relation between HPV and cervical cancer was 16.8% in our study, whereas this rate was 40%, 47.8%, and 54.3% in other studies [10,16,17]. The most important reason for this difference is that 72% of the group participated in our study were illiterate or graduated from primary school (up to 11 years old). In another two studies performed in our country, the low education level was notified as 18% and 2.4% [10,15].
In our study group, the rate of graduation from university was a low rate equal to 12%. In the group graduated from university, the rates of knowing HPV, HPV vaccine and the relation between HPV and cervical cancer were 78%, 58%, and 70% and similar to the results of the studies carried out in developed provinces and other countries. The high education level is strongly correlated with the knowledge of HPV and cervical cancer [18].
The rates of knowing HPV (26%), HPV vaccine (21%) and the relation between HPV and cervical cancer (16.8%) are low due to the low education level of our study group. However, the study group's rate of knowing cervical cancer vaccine is 49%. This means that half of the women know the vaccine when talked about cervical cancer vaccine, but this rate decreases to one to five when talked about HPV vaccine. Furthermore, 75% of the women in this group use valid contraception and 53% underwent regular Pap smear. The reason for this inconsistent situation is that 83.8% of the group is housewives. For housewives, the rate of watching TV is very high. In the women programs called "morning program" in the TV channels in our country, the issues about health and sexuality are discussed and such information that will raise the awareness of the audience on this matter is given. For this reason, the women's health is more prior among the housewives. The introduction of HPV vaccine and the increase of its acceptance can be ensured by including these subjects into these programs much more.
The general rate of accepting HPV vaccine is 40%, whereas this rate is 60% for the women who are graduated from university. The rates of knowledge about HPV show great difference in these two groups, but the difference is not very high in the acceptance of the vaccine. In addition, the rates of the women's using of contraception, undergoing regular Pap smear and undergoing regular gynecological examination are similar with the rates of the women who are graduated from university (75.9% vs. 71.8%, 53% vs. 66%, 32% vs. 39%). This indicates that those who are graduated from university have the knowledge, but this knowledge does not lead to behavioral change. However, the general study group makes more efforts in terms of women's health in spite of less information. This indicates that the visual media and probably the other environmental factors have more influences on the behavioral change.
HPV vaccine's being of free-of-charge has become a significant parameter. If the vaccination is free-of-charge, the acceptance of the vaccine is 92%, but the rate of vaccination with charge decreases to the half. The reason for this is that 83.8% of our study group is unemployed so that they are dependent on their husbands in terms of economy. In addition, the expenses of the house are covered by the income of the one person employed; it is difficult to allocate resources for this matter. The province where the study was performed is not a rich region in terms of socio-economy and this might have caused that the fee has become a significant parameter in the acceptance of the vaccine. However, 45% of the participants in the study performed in Belgium accepted vaccine provided that the vaccine fee will be taken back. Also in the study performed by Dursun et al. [10], 88% of the participants request for the payment of the vaccine by the Social Security Agency. Accordingly, the vaccination fee always constitutes a barrier for the vaccination program.
A vaccinated relative or friend increases the rate of acceptance of HPV vaccine 2.8 times more. Our study group has low education level. In the societies with low socioculture and education level, getting information based on mainly environmental factors rather than books and training devices and the expert of the matter. For this reason, hearing about existence of the vaccine, the reason for vaccination, the side effects of it, and the manner of vaccination from a vaccinated person, increases the acceptance of the vaccine. However, 79% of the participants notified that they desired to get information from the family practice in the study carried out in Australia [12].
For the women in our study group, the rate of accepting HPV vaccine for themselves and requesting for their daughters are quite similar (40% and 36.3%). However, this rate decreased to 26% in the vaccination of the male children. In other studies carried out in Turkey, the rate of vaccination for the male children is high as much as 59% and 89% [10,15]. The reason for this is that the province where our study was performed has a male-dominant social structure that gives more importance and protects the male child.
The married and single women in our study group accepted HPV vaccine at similar rates. In the study performed by Dursun et al. [10], this rate was in favor of the single women (70% vs. 30%). In the eastern region of our country, there is a general acceptance about that the single women in the society cannot have sexual lives and that the sexual life will start after marriage. For this reason, the married and single women considered HPV vaccine in similar way.
The rate of knowing about HPV and accepting HPV vaccine in the age group of 25 was higher than the other age groups. The study carried out by Tiro et al. [16] supported our results. However, this age group-as unexpected by the researchers- was found less-informed about HPV and less sensitive to vaccine in the study carried out in Belgium. However, this group has higher education level as in our study [11].
In our study, the education levels, employment status, knowledge about HPV of the women in the group under the age of 25 was always higher than the other age groups. For this reason, this age group has become a predictive factor in the acceptance of HPV.
The subjects were recruited from the general gynecology outpatient clinic of the hospital. The patients from STD and oncology outpatient clinics were not included in the study. The range of age (18 to 66 years) is wide enough to stand for the general population and the subjects are not very different from healthy population as shown in the causes of application in Table 4. Table 5 summarizes the recent studies on the HPV knowledge and acceptability across the different regions of the world.
In conclusion, the young population and the women who graduated from university seem to be more well-informed about HPV and more sensitive about being vaccinated. However, the state-of-the-art means of communication such as social environment and visual media come into prominence in ensuring information and behavioral change in both this population and other women groups. The more efficient use of these means of communications will ensure the awareness-raising of the community about HPV and HPV vaccine. In addition, free vaccination-for at least the lowest economic group-as required by the social state will ensure the expansion of the vaccine.
Figures and Tables
References
1. Burd EM. Human papillomavirus and cervical cancer. Clin Microbiol Rev. 2003. 16:1–17.
2. Cates W Jr. Estimates of the incidence and prevalence of sexually transmitted diseases in the United States: American Social Health Association Panel. Sex Transm Dis. 1999. 26:S2–S7.
3. Harro CD, Pang YY, Roden RB, Hildesheim A, Wang Z, Reynolds MJ, et al. Safety and immunogenicity trial in adult volunteers of a human papillomavirus 16 L1 virus-like particle vaccine. J Natl Cancer Inst. 2001. 93:284–292.
4. Jin XW, Cash J, Kennedy AW. Human papillomavirus typing and the reduction of cervical cancer risk. Cleve Clin J Med. 1999. 66:533–539.
5. Tuncer M. Cancer control in Turkey. 2008. Ankara: Ministry of Health Publication.
6. Inal MM, Kose S, Yildirim Y, Ozdemir Y, Toz E, Ertopcu K, et al. The relationship between human papillomavirus infection and cervical intraepithelial neoplasia in Turkish women. Int J Gynecol Cancer. 2007. 17:1266–1270.
7. Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER, et al. Quadrivalent human papillomavirus vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2007. 56:1–24.
8. Koutsky L. Epidemiology of genital human papillomavirus infection. Am J Med. 1997. 102:3–8.
9. Slomovitz BM, Sun CC, Frumovitz M, Soliman PT, Schmeler KM, Pearson HC, et al. Are women ready for the HPV vaccine? Gynecol Oncol. 2006. 103:151–154.
10. Dursun P, Altuntas B, Kuscu E, Ayhan A. Women's knowledge about human papillomavirus and their acceptance of HPV vaccine. Aust N Z J Obstet Gynaecol. 2009. 49:202–206.
11. Donders GG, Gabrovska M, Bellen G, Van Keirsbilck J, Van Den Bosch T, Riphagen I, et al. Knowledge of cervix cancer, human papilloma virus (HPV) and HPV vaccination at the moment of introduction of the vaccine in women in Belgium. Arch Gynecol Obstet. 2008. 277:291–298.
12. Giles M, Garland S. A study of women's knowledge regarding human papillomavirus infection, cervical cancer and human papillomavirus vaccines. Aust N Z J Obstet Gynaecol. 2006. 46:311–315.
13. Oren A, Skjeldestad FE. Little knowledge about human papillomavirus among young Norwegian women. Tidsskr Nor Laegeforen. 2006. 126:2101–2103.
14. Moreira ED Jr, Oliveira BG, Ferraz FM, Costa S, Costa Filho JO, Karic G. Knowledge and attitudes about human papillomavirus, Pap smears, and cervical cancer among young women in Brazil: implications for health education and prevention. Int J Gynecol Cancer. 2006. 16:599–603.
15. Baykal C, Al A, Ugur MG, Cetinkaya N, Attar R, Arioglu P. Knowledge and interest of Turkish women about cervical cancer and HPV vaccine. Eur J Gynaecol Oncol. 2008. 29:76–79.
16. Tiro JA, Meissner HI, Kobrin S, Chollette V. What do women in the U.S. know about human papillomavirus and cervical cancer? Cancer Epidemiol Biomarkers Prev. 2007. 16:288–294.
17. Dempsey AF, Zimet GD, Davis RL, Koutsky L. Factors that are associated with parental acceptance of human papillomavirus vaccines: a randomized intervention study of written information about HPV. Pediatrics. 2006. 117:1486–1493.
18. Massad LS, Verhulst SJ, Hagemeyer M, Brady P. Knowledge of the cervical cancer screening process among rural and urban illinois women undergoing colposcopy. J Low Genit Tract Dis. 2006. 10:252–255.
19. Weisberg E, Bateson D, McCaffery K, Skinner SR. HPV vaccination catch up program: utilisation by young Australian women. Aust Fam Physician. 2009. 38:72–76.
20. Kwan TT, Chan KK, Yip AM, Tam KF, Cheung AN, Lo SS, et al. Acceptability of human papillomavirus vaccination among Chinese women: concerns and implications. BJOG. 2009. 116:501–510.
21. Oh H. Knowledge about HPV, and the attitudes toward HPV vaccination among adult women in Asian countries: a literature review. J Korean Oncol Nurs. 2011. 11:171–178.
22. Di Giuseppe G, Abbate R, Liguori G, Albano L, Angelillo IF. Human papillomavirus and vaccination: knowledge, attitudes, and behavioural intention in adolescents and young women in Italy. Br J Cancer. 2008. 99:225–229.
23. Pelucchi C, Esposito S, Galeone C, Semino M, Sabatini C, Picciolli I, et al. Knowledge of human papillomavirus infection and its prevention among adolescents and parents in the greater Milan area, Northern Italy. BMC Public Health. 2010. 10:378.
24. Perkins RB, Langrish SM, Stern LJ, Burgess JF, Simon CJ. Impact of patient adherence and test performance on the cost-effectiveness of cervical cancer screening in developing countries: the case of Honduras. Womens Health Issues. 2010. 20:35–42.
25. Litton AG, Desmond RA, Gilliland J, Huh WK, Franklin FA. Factors associated with intention to vaccinate a daughter against HPV: a statewide survey in Alabama. J Pediatr Adolesc Gynecol. 2011. 24:166–171.
26. DiAngi YT, Panozzo CA, Ramogola-Masire D, Steenhoff AP, Brewer NT. A cross-sectional study of HPV vaccine acceptability in Gaborone, Botswana. PLoS One. 2011. 6:e25481.
27. Do YK, Wong KY. Awareness and acceptability of human papillomavirus vaccine: an application of the instrumental variables bivariate probit model. BMC Public Health. 2012. 12:31.
28. Becker-Dreps S, Otieno WA, Brewer NT, Agot K, Smith JS. HPV vaccine acceptability among Kenyan women. Vaccine. 2010. 28:4864–4867.
29. Sauvageau C, Duval B, Gilca V, Lavoie F, Ouakki M. Human papilloma virus vaccine and cervical cancer screening acceptability among adults in Quebec, Canada. BMC Public Health. 2007. 7:304.
30. Manhart LE, Burgess-Hull AJ, Fleming CB, Bailey JA, Haggerty KP, Catalano RF. HPV vaccination among a community sample of young adult women. Vaccine. 2011. 29:5238–5244.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download