Abstract
Objective
Little is known regarding cervical cancer survivors' employment status, which represents social integration of cancer survivors as a pivotal domain of long-term quality of life. The goal of this study was to assess the correlates of unemployment and evaluate the impact on the comprehensive quality of life in cervical cancer survivors.
Methods
We enrolled 858 cervical cancer survivors from the gynecologic oncology departments of multi-centers in Korea. Factors associated with unemployment were identified using multivariate logistic regression analyses. We assessed different health-related quality of life domains with multivariate-adjusted least-square means between cervical cancer survivors who currently work and do not.
Results
After diagnosis and treatment, the percentage of unemployed survivors increased from 50.6% to 72.8%. Lower income (adjusted odds ratio [aOR], 1.97; 95% confidence interval [CI], 1.38 to 2.81), medical aid (aOR, 1.58; 95% CI, 1.05 to 2.38), two or more comorbidities (aOR, 1.80; 95% CI, 1.12 to 2.90), current alcohol drinkers (aOR, 2.33; 95% CI, 1.54 to 3.52), and employed at the time of diagnosis (aOR, 10.72; 95% CI, 7.10 to 16.16) were significantly associated with unemployment. Non-working groups showed significant differences with respect to physical functioning, role functioning, depression, and existential well-being.
Conclusion
The proportion of unemployed cervical cancer survivors seems to increase, with low-income status and the presence of medical aid negatively being associated with employment, in addition to other comorbidities and previous working status. Effort should be made to secure the financial status of cervical cancer survivors.
Despite high mortality rates, advances in the treatment and early detection of cancer have allowed patients live longer and overcome their disease. Cancer survivorship, as a holistic approach for cancer survivors, has been suggested that long-term management of physical, psychological, and social needs should receive more attention. Among these, social rehabilitation is more important than dealing with only physical and psychosocial problems because most cancer survivors are young enough to return to work after treatment. Employment is the key indicator of restoration of social roles [1] and is known to maintain emotional function and self-esteem in cancer survivors [1,2], as well as reduce the economical burden on society.
Currently, most cancer survivors desire and are able to return to work, with the percentage ranging from 27% to 95% [3,4]. However, some cancer survivors are observed as having a higher risk for unemployment than the general population or patients with other morbidities [5]. To predict those who may lose jobs and plan intervention for those groups accordingly, several studies have attempted to identify the correlates of unemployment. As a result, disease-related factors such as cancer site [6], stage [7], type of treatment [5] , as well as socio-demographic factors such as age [5], marital status [8], and income [9] were reported to be associated with unemployment as much as work-related factors such as workplace atmosphere [6] or type of work [6,7].
Gender, one of the socio-demographic factors, has been reported to change the unemployment rate among cancer survivors [9,10]. Women with cancer possess a higher risk of losing their jobs than men with cancer. However, only a few studies have focused on the fact that women may be vulnerable to unemployment and examined the reason for higher risk [10]. In addition, most previous studies that investigated unemployment in female cancer survivors were conducted with the breast cancer survivors [7,11]. Survivors of cervical cancer, the fifth most common cancer in women, have their own complications caused by different type of treatment such as pelvic surgery, which is more extensive than mastectomy, and may have different consequences on quality of life [12]. Nevertheless, little is known regarding cervical cancer survivors' employment status, although a few qualitative studies were conducted to explain work-related difficulties that cervical cancer survivors may experience [13].
The goal of this study was to assess the correlates of unemployment and evaluate the impact on the comprehensive quality of life in cervical cancer survivors.
From 1983 through 2004, 7028 women from the gynecological oncology departments in six hospitals in South Korea were identified who met the following criteria: patients who 1) had been diagnosed with and treated for cervical cancer (stage I to IVA), 2) had no current evidence of disease, 3) were not currently undergoing cancer treatment, and 4) had not been diagnosed with other cancers. Participants were excluded if they did not answer either of two work-related questions: previous working status and current working status.
Of 7,028 potentially eligible participants, 1,085 (15.4%) died. Of the remaining participants, 3,127 (44.55%) could not be contacted (predominantly because of a change of address or phone number), 927 (13.19%) refused enrollment on the phone, and 898 (12.78%) returned incomplete questionnaires due to being busy, inconvenience, or concerns about providing personal information. After reviewing the collected questionnaires, 38 women whose disease had recurred or who were undergoing current treatment, were excluded. Another 2 women did not complete the work-related questions; therefore, a total of 858 women were included in the analyses (response rate, 14.44%). These recruitment and enrollment procedures were described in a previously published study [14].
Participants were contacted by telephone, and sent the questionnaire and written informed consent form after they agreed to participate in the study. Cancer-related and clinical information including stage, type of treatment, and time from treatment was collected from the hospital cancer registries. Other socio-demographic, clinical data, and quality of life-related questions were asked in the questionnaire form that was used in our previous study [14]. The Institutional Review Board of the Korean National Cancer Center approved all documents sent to participants.
We defined 'working' as being employed or self-employed regardless of job type and the number of working hours, and 'non-working' as being retired or a homemaker. We investigated the difficulties frequently experienced while working, to the women who answered 'working' and doing housework to those who were 'non-working,' with multiple-choice items. The questions for the work-related difficulties involved non-attendance at work in the last year and working limitations because of the disease. Questions regarding housework-related difficulties included physical functional limitations, easily fatigued or exhausted, and emotional distress (such as depression or anxiety). If participants experienced other kinds of difficulties not included in the choices, they were asked to write it in.
Age at the time of survey (<50 years vs. ≥50 years), marital status (married vs. widowed/divorced/separated/single), educational level (not a high school graduate vs. high school graduate or more), the presence of religion (yes vs. no), monthly household income (<$3,000 vs. ≥$3,000), and type of insurance (medical aid vs. health insurance) were assessed.
Questions were asked about menopausal status (yes vs. no), the number of comorbidities (≤1 vs. ≥2, including coronary artery disease, diabetes, chronic lung disease, musculoskeletal disease, or gastrointestinal disease), regular physical activity (yes vs. no), current smoking (yes vs. no), and alcohol consumption (yes vs. no). Cancer-related characteristics including stage (I-IIA vs. IIB-IVA), time since treatment (<5 years vs. ≥5 years), history of chemotherapy (yes vs. no) and type of local treatment (surgery only vs. surgery+radiotherapy vs. radiotherapy only) were asked and evaluated in the same manner.
The European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire Core 30 (QLQ-C30) was used to measure the general health-related quality of life in cancer patients. It is composed of 30 items that are grouped into 5 functional domains, 3 symptom domains, and several single questions [15]. The Korean version has been validated [16].
The Hospital Anxiety and Depression Scale (HADS) was a tool for identifying anxiety and depression among hospitalized patients without psychiatric illness [17]. It has been used previously in many studies involving Korean cancer patients [18]. The anxiety and depression subscales have 7 questions respectively in mixed order.
The existential well-being of cancer survivors was assessed by the Korean version of McGill Quality of Life Questionnaire, which is useful for measuring existentiality and support from the environment, particularly in terminally-ill patients, and was validated with the original author's approval [19].
We used descriptive statistics to explain socio-demographic and clinical variables. To examine which factors have statistical significance for unemployment, we conducted univariate logistic regression analyses and included the significant variables in multivariate logistic regression analyses. We reported the results as odd ratios (ORs) with 95% confidence intervals (CIs). For comparisons of HRQoL between cervical cancer survivors who currently work and those who do not, we created a generalized linear model and used analyses of covariance to calculate multivariate-adjusted means of HRQoL including EORTC QLQ-C30, HADS, and existential QoL. We scored the QLQ-C30 and QLQ-CX24 items according to the EORTC scoring manual. We linearly transformed the QLQ-C30 and QLQ-CX24 data to yield scores from 0 to 100; a higher score represented a better level of functioning or a higher level of symptoms, respectively. We handled incomplete questionnaires according to the developers' recommendations; when we had values for at least half the items in a scale, we recorded the missing values as their mean. All statistical tests were two-tailed. We used SAS ver. 9.3 (SAS Institute, Cary, NC, USA).
Table 1 shows the characteristics of cervical cancer survivors. At the time of diagnosis, 424 women (49.4%) were working, and 434 (50.6%) were not working. After diagnosis and treatment, the percentage of non-working women increased from 50.6% to 72.8%. Among non-working women, the proportion of unemployed or retired women increased more (16.4% to 20.5%) than the proportion of homemakers (83.6% to 79.5%).
In the univariate analyses, younger age (p<0.001) lower educational background (p=0.034), lower household income status (p=0.002), medical aid (p=0.001), menopause (p=0.002), multiple comorbidities (p=0.002), less than 5 years since treatment (p=0.012), and a history of surgery and radiotherapy (p=0.027) was correlated with a high risk of unemployment. Women who currently drink alcohol (p<0.001) were also highly likely to be unemployed. Above all, previous employment status (p<0.001) was the most significant factor (Table 2).
With the statistically significant factors from the univariate results, multivariate logistic regression analyses were performed using a stepwise selection method (p<0.05). Such analyses showed that having lower income (adjusted odds ratio [aOR], 1.97; 95% CI, 1.38 to 2.81), receiving medical aid (aOR, 1.58; 95% CI, 1.05 to 2.38), having two or more comorbidities (aOR, 1.80; 95% CI, 1.12 to 2.90), drinking alcohol currently (aOR, 2.33; 95% CI, 1.54 to 3.52), and working at the time of diagnosis (aOR, 10.72; 95% CI, 7.10 to 16.16) were significantly associated with unemployment in cervical cancer survivors (Table 3).
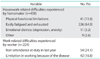
Among the 224 survivors who answered the work-related difficulties questionnaire, 24.1% experienced non-attendance on duty in last year, and 18.8% had limitations in working because of the disease. For homemakers who do not have a job outside the home, 64.9% were easily fatigued and exhausted, 11.8% had limitation in physical, and 3.2% were distressed emotionally (Table 4).
Fig. 1 presents the multivariate-adjusted least-square mean scores for EORTC QLQ-C30, HADS-A, HAD-D, and the McGill Quality of Life Questionnaire existential and support scales in cancer survivors by current working status. There were statistically significant differences in physical functioning, role functioning, depression, and existential well-being between working and non-working groups.
To our knowledge, this is the first study investigating factors that influence cervical cancer survivors' unemployment risk and impact quality of life. Cervical cancer survivors with lower income, who were previously unemployed, and have other comorbidities are at a higher risk of unemployment. In addition, cervical cancer survivors' unemployment was associated with an impaired quality of life, including physical functioning, role functioning, depression, and existential well-being.
Among 858 cervical cancer survivors, 54.9% of the 424 women who previously worked remained employed after cancer treatment. Although this is retrospective data acquired in a cross-sectional study, it shows a similar result with previous data: 58.9% of Korean breast cancer survivors who were employed before their cancer diagnosis returned to work [20]. A previous study found 61.1% returned to work [21]. However, our results showed lower percentage of return to work compared with a study conducted with breast cancer survivors in European countries that found 75% to 85% of survivors returned to work [22]. These results could reflect findings that Western females are more likely to want to return to work compared to Asian females [21].
Compared to the previous studies that reported the return to work rate in cervical cancer survivors, our results demonstrated lower rate of return to work [23,24]. Supported by the data indicating cervical cancer survivors could not share their worries with others [25], it implies that Korean cervical cancer survivors may be intimidated to speak out to their workers about their disease and be fragile when adapting to new circumstances. Moreover, because no systematic research has been conducted specifically focused on cervical cancer, our results could be unique and reliable.
Some of the correlates observed in this study were consistent with other studies. Our finding that low-income affected cervical cancer survivors' unemployment is consistent with those of previous studies [9,11] as well as with what has been reported in Korea [20,21]. It is possible that low-income is both a cause and a result of unemployment because of the study design as cross- sectional one. Regardless, unemployed cancer survivors with low-income status have a worse quality of life compared to the employed [20]. People with higher incomes usually represent higher positions in the workplace and seem relatively well-treated compared with lower income [26]. In addition, cervical cancer survivors who receive medical aid also seem to be at higher risk compared with patients who have health insurance. In contrast to a country such as the United States in which an unemployed person has to deal with all healthcare costs, Korea has a national insurance system. Therefore, in the Korean population, the presence of medical aid reflects a level of income rather than the drive against fear of losing a job [20,21]. If a person has an income status slightly above the qualifications for medical aid, it would be better not to work because most medical services for cancer survivors can be supported by medical aid.
Survivors with two or more comorbidities seemed not to return to work compared to patients with less than two comorbidities. This is consistent with findings in other studies [5,27,28].
The correlation of drinking alcohol with employment status was unexpected. Among clinical factors specifically representing lifestyle, drinking alcohol is usually thought to decrease working ability. However, females drink less than males. In addition, cancer survivors have lower or similar rates of drinking alcohol than populations without cancer [29]. In Korea, it is common to have dinner after work with their colleagues, where alcohol is consumed frequently. Additionally, there is a widespread belief among Koreans that someone who "drinks well" is also good at social relationships in the workplace. No alcohol because of physical difficulties such as nausea and vomiting, which are pelvic surgery-induced complications, may influence the image of the survivor to the co-workers and make workplace relationships more difficult. As a cross-sectional study, however, it is possible that working people have a higher chance to drink compared to non-working individuals. Although lifestyle-related factors such as exercise, drinking, and smoking influence the quality of life in cancer survivors [28], few studies have discussed alcohol consumption as one of the factors affecting employment [30]. Our results require further investigation regarding possible associations between drinking and social pressure in the workplace.
Survivors who previously worked were less likely to be unemployed than non-working survivors. Because our study was conducted with survivors regardless of the presence of job, we hypothesize that people who did not work previously will be hard to get a job after the cancer diagnosis and treatment.
Previous studies agreed with our finding that employment status is associated with health-related quality of life, particularly physical function, role function, depression, and existentiality. Decreased physical function in cancer survivors has been reported in many studies [31], suggesting that non-working survivors may do less physical activity.
As mentioned in previous studies on other cancer types, including thyroid cancer [32], employment seems essential to maintain role function. Moreover, it was reported that role function specifically related to work was decreased in cervical cancer survivors [13].
In the general population, paid work has seemed to decrease the risk of depression [33]. Other studies have focused on high prevalence of depression in cancer survivors [34]. However, little is known about the impact of unemployment on depression in cancer survivors. Alternatively, depression may be the cause of unemployment [35]. More evidence is necessary to determine the association of depression with employment status [36]. Similar to the previous studies in Korea and Japan [37,38], employment outcome was related to existential well-being.
This study has several limitations. First, although work-related factors are known to affect employment of cancer survivors, they were not discussed in depth in this study. A comprehensive study is needed. Second, we defined working status as binomial groups ('working' and 'non-working'), which do not completely consider the comprehensive work-related outcome. Despite our effort to measure which kind of work-related difficulties were observed by cancer survivors, we still need to measure different types of work outcomes, such as working hours, work effort, work limitations, or work performance. Third, it is possible that reverse causality remains due to the cross- sectional study design. In particular, the cause-and-effect relationship between employment and HRQoL domains could be flexibly reversed in the one that working has impact on HRQoL in cervical cancer survivors. In addition to studies that report HRQoL affects working status in people with cancer [39], more studies should investigate whether employment improves health or vice versa, or both [40]. Fourth, although cervical cancer usually develops at a relatively young age, it is possible that 66.9% of women who were older than 50 years old in our study population might already be retired due to their age. Fifth, the population analyzed in our study might not represent general population of cervical cancer survivors. Finally, as we discussed previously, the low response rate might have resulted in potential biases [14].
Despite these limitations, our study demonstrates that cervical cancer survivors with lower income, who were previously unemployed, and have other comorbidities are at a higher risk of unemployment and decreased HRQoL. Because employment is related to HRQoL, we should provide more support to help cancer survivors return to work as soon as possible. Cancer survivors at higher risks should be the critical targets for active intervention in the search for employment.
As mentioned in A National Action Plan for Cancer Survivorship: Advancing Public Health Strategies by the United States Centers for Disease Control, reducing the financial burden should be prioritized to help cancer survivors cope with their own economic activity.
This study also addresses the question of what cervical cancer survivors who are at a risk of being unemployed can do for a living, despite poor conditions that interfere with their ability to return to work. It may not be appropriate for them to have a physically challenging job, like other survivors who easily return to work. We suggest that they need to share what they have learned from experiences by making a health partnership with cancer patients. In this way, cancer survivors can be benefited from the relationship to return to their respective social roles and improve their economic status. We suggest that national programs of employment support are needed for women who want to return to work.
Figures and Tables
 | Fig. 1Least-squares mean scores from (A) European Organisation for Research and Treatment of Cancer Quality of Life Questionaire Core 30 (0 to 80), (B) Hospital Anxiety and Depression Score (0 to 50), (C) McGill Quality of Life Questionnaire existentiality and support (0 to 8) (adjusted for age, marital status, educational level, monthly income, religion, previous employment status, menopausal status, time since treatment, comorbidities, regular physical activity, current smoking, current drinking alcohol). *p<0.05. |
Table 2
Univariate results of relationship between employment status and patient characteristics in cervical cancer survivors

Table 3
Adjusted odds ratio of employment status among cancer-survivors (n=841)
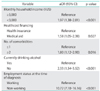
Multiple logistic regression analysis including variables identified as statistically significant predictors in univariate analysis of correlates of not working (adjusted for age, educational level, monthly income, healthcost financing, menopausal status, comorbidites, previous employment status, currently drinking alcohol, time since treatment, type of local treatment). aOR, adjusted odds ratio.
ACKNOWLEDGMENTS
This research was supported by National Cancer Center (Korea) Grant 04101502 and partially by the Korean National Cancer Control Program by the Korean Ministry for Health and Welfare Affairs.
References
1. Peteet JR. Cancer and the meaning of work. Gen Hosp Psychiatry. 2000; 22:200–205.
2. Rasmussen DM, Elverdam B. The meaning of work and working life after cancer: an interview study. Psychooncology. 2008; 17:1232–1238.
3. Bergman B, Sorenson S. Return to work among patients with small cell lung cancer. Eur J Respir Dis. 1987; 70:49–53.
4. Rieker PP, Fitzgerald EM, Kalish LA, Richie JP, Lederman GS, Edbril SD, et al. Psychosocial factors, curative therapies, and behavioral outcomes: a comparison of testis cancer survivors and a control group of healthy men. Cancer. 1989; 64:2399–2407.
5. Mols F, Thong MS, Vreugdenhil G, van de Poll-Franse LV. Long-term cancer survivors experience work changes after diagnosis: results of a population-based study. Psychooncology. 2009; 18:1252–1260.
6. Taskila T, Lindbohm ML. Factors affecting cancer survivors' employment and work ability. Acta Oncol. 2007; 46:446–451.
7. Bouknight RR, Bradley CJ, Luo Z. Correlates of return to work for breast cancer survivors. J Clin Oncol. 2006; 24:345–353.
8. Nagarajan R, Neglia JP, Clohisy DR, Yasui Y, Greenberg M, Hudson M, et al. Education, employment, insurance, and marital status among 694 survivors of pediatric lower extremity bone tumors: a report from the childhood cancer survivor study. Cancer. 2003; 97:2554–2564.
9. Torp S, Nielsen RA, Fossa SD, Gudbergsson SB, Dahl AA. Change in employment status of 5-year cancer survivors. Eur J Public Health. 2013; 23:116–122.
10. Gudbergsson SB, Fossa SD, Dahl AA. Are there sex differences in the work ability of cancer survivors? Norwegian experiences from the NOCWO study. Support Care Cancer. 2011; 19:323–331.
11. Drolet M, Maunsell E, Brisson J, Brisson C, Masse B, Deschenes L. Not working 3 years after breast cancer: predictors in a population-based study. J Clin Oncol. 2005; 23:8305–8312.
12. Greimel E, Thiel I, Peintinger F, Cegnar I, Pongratz E. Prospective assessment of quality of life of female cancer patients. Gynecol Oncol. 2002; 85:140–147.
13. Frazier LM, Miller VA, Horbelt DV, Delmore JE, Miller BE, Averett EP. Employment and quality of survivorship among women with cancer: domains not captured by quality of life instruments. Cancer Control. 2009; 16:57–65.
14. Park SY, Bae DS, Nam JH, Park CT, Cho CH, Lee JM, et al. Quality of life and sexual problems in disease-free survivors of cervical cancer compared with the general population. Cancer. 2007; 110:2716–2725.
15. Coates A, Porzsolt F, Osoba D. Quality of life in oncology practice: prognostic value of EORTC QLQ-C30 scores in patients with advanced malignancy. Eur J Cancer. 1997; 33:1025–1030.
16. Yun YH, Park YS, Lee ES, Bang SM, Heo DS, Park SY, et al. Validation of the Korean version of the EORTC QLQ-C30. Qual Life Res. 2004; 13:863–868.
17. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res. 2002; 52:69–77.
18. Shim EJ, Hahm BJ. Anxiety, helplessness/hopelessness and desire for hastened death in Korean cancer patients. Eur J Cancer Care (Engl). 2011; 20:395–402.
19. Kim SH, Gu SK, Yun YH, Lee CG, Choi YS, Lee WS, et al. Validation study of the Korean version of the McGill Quality of Life Questionnaire. Palliat Med. 2007; 21:441–447.
20. Ahn E, Cho J, Shin DW, Park BW, Ahn SH, Noh DY, et al. Impact of breast cancer diagnosis and treatment on work-related life and factors affecting them. Breast Cancer Res Treat. 2009; 116:609–616.
21. Park JH, Park EC, Park JH, Kim SG, Lee SY. Job loss and re-employment of cancer patients in Korean employees: a nationwide retrospective cohort study. J Clin Oncol. 2008; 26:1302–1309.
22. Hoving JL, Broekhuizen ML, Frings-Dresen MH. Return to work of breast cancer survivors: a systematic review of intervention studies. BMC Cancer. 2009; 9:117.
23. Greenwald HP, McCorkle R, Fennie K. Health status and adaptation among long-term cervical cancer survivors. Gynecol Oncol. 2008; 111:449–454.
24. Nachreiner NM, Ghebre RG, Virnig BA, Shanley R. Early work patterns for gynaecological cancer survivors in the USA. Occup Med (Lond). 2012; 62:23–28.
25. Wenzel L, DeAlba I, Habbal R, Kluhsman BC, Fairclough D, Krebs LU, et al. Quality of life in long-term cervical cancer survivors. Gynecol Oncol. 2005; 97:310–317.
26. Taskila-Brandt T, Martikainen R, Virtanen SV, Pukkala E, Hietanen P, Lindbohm ML. The impact of education and occupation on the employment status of cancer survivors. Eur J Cancer. 2004; 40:2488–2493.
27. Munir F, Yarker J, McDermott H. Employment and the common cancers: correlates of work ability during or following cancer treatment. Occup Med (Lond). 2009; 59:381–389.
28. Beesley VL, Eakin EG, Janda M, Battistutta D. Gynecological cancer survivors' health behaviors and their associations with quality of life. Cancer Causes Control. 2008; 19:775–782.
29. Grimmett C, Bridgewater J, Steptoe A, Wardle J. Lifestyle and quality of life in colorectal cancer survivors. Qual Life Res. 2011; 20:1237–1245.
30. Bifulco G, De Rosa N, Tornesello ML, Piccoli R, Bertrando A, Lavitola G, et al. Quality of life, lifestyle behavior and employment experience: a comparison between young and midlife survivors of gynecology early stage cancers. Gynecol Oncol. 2012; 124:444–451.
31. Mahar KK, BrintzenhofeSzoc K, Shields JJ. The impact of changes in employment status on psychosocial well-being: a study of breast cancer survivors. J Psychosoc Oncol. 2008; 26:1–17.
32. Lee JI, Kim SH, Tan AH, Kim HK, Jang HW, Hur KY, et al. Decreased health-related quality of life in disease-free survivors of differentiated thyroid cancer in Korea. Health Qual Life Outcomes. 2010; 8:101.
33. Glass J, Fujimoto T. Housework, paid work, and depression among husbands and wives. J Health Soc Behav. 1994; 35:179–191.
34. Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004; 32:57–71.
35. Steiner JF, Cavender TA, Nowels CT, Beaty BL, Bradley CJ, Fairclough DL, et al. The impact of physical and psychosocial factors on work characteristics after cancer. Psychooncology. 2008; 17:138–147.
36. Ell K, Sanchez K, Vourlekis B, Lee PJ, Dwight-Johnson M, Lagomasino I, et al. Depression, correlates of depression, and receipt of depression care among low-income women with breast or gynecologic cancer. J Clin Oncol. 2005; 23:3052–3060.
37. Shin HW, Noh DY, Lee ES, Nam SJ, Park BW, et al. Correlates of existential well-being and their association with health-related quality of life in breast cancer survivors compared with the general population. Breast Cancer Res Treat. 2009; 118:139–150.
38. Kobayashi K, Morita S, Shimonagayoshi M, Kobayashi M, Fujiki Y, Uchida Y, et al. Effects of socioeconomic factors and cancer survivors' worries on their quality of life (QOL) in Japan. Psychooncology. 2008; 17:606–611.
39. Spelten ER, Verbeek JH, Uitterhoeve AL, Ansink AC, van der Lelie J, de Reijke TM, et al. Cancer, fatigue and the return of patients to work-a prospective cohort study. Eur J Cancer. 2003; 39:1562–1567.
40. Ross CE, Mirowsky J. Does employment affect health? J Health Soc Behav. 1995; 36:230–243.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download