Abstract
Objective
Intraperitoneal (IP) chemotherapy in women with optimally debulked stage III ovarian cancer has been reported to prolong overall survival, but has not been widely adopted due to concerns about its toxicity, inconvenience and acceptability to patients. The purposes of this study were to determine the regimen's feasibility, adverse events, catheter-related complications, progression-free survival, health-related quality of life (HRQL), and patients' preferences for IP versus intravenous (IV) chemotherapy.
Methods
We conducted a single arm, multi-center study of IP chemotherapy with IV paclitaxel 135 mg/m2 (D1) over 3 hours, IP cisplatin 75 mg/m2 (D2), and IP paclitaxel 60 mg/m2 (D8) for 6 cycles in women with optimally debulked stage III ovarian or related cancers.
Results
Thirty-eight eligible patients were recruited from 12 sites between July 2007 and December 2009. Seventy-one percent (n=27) completed at least 4 cycles and 63% (n=24) completed all 6 cycles. Grade 3 or 4 adverse events included nausea (n=2), vomiting (n=2), abdominal pain (n=2), and diarrhea (n=1), but not febrile neutropenia, neurotoxicity, or nephropathy. There were no treatment-related deaths. Catheter-related complications were the most frequent cause of early discontinuation of treatment (16 patients, 21%). Apart from neurotoxicity HRQL which worsened over time, HRQL was stable or improved with time. Most patients (≥50%) judged moderate benefits (e.g., an extra 6 months survival time or a 5% improvement in survival rates) necessary to make IP chemotherapy worthwhile.
Ovarian cancer is the leading cause of gynaecological cancer death with an estimated 225,500 new cases and 140,200 deaths worldwide in 2008 [1]. Most patients with ovarian cancer present with the epithelial histological subtype (90%) and advanced disease (International Federation of Gynecology and Obstetrics [FIGO] stage III or IV) (75%) at initial diagnosis [2].
The standard adjuvant treatment of patients with optimally debulked advanced ovarian cancer is intravenous (IV) chemotherapy with a platinum and taxane for 6 cycles [3,4]. The median progression-free survival (PFS) is 16 months and the median overall survival (OS) is 40 months. Patients with no macroscopic residual disease after surgery have better OS than patients with <1 cm residual disease, with a 5-year OS of approximately 50% versus 30%, respectively. These OS figures show that there is room for improvement in the management of these patients, including more effective adjuvant systemic therapy [4,5].
Advanced ovarian cancer is ideally suited to treatment with intraperitoneal (IP) chemotherapy because the tumor is commonly confined to the peritoneal cavity [6]. The potential advantage of IP chemotherapy over IV chemotherapy is that IP chemotherapy exposes tumor cells within the peritoneal cavity to much higher concentrations of cytotoxic drugs, as well as these being absorbed into the systemic circulation.
Results of randomized trials and meta-analyses show a survival benefit of a combination of IP and IV chemotherapy, over IV chemotherapy alone, in patients with optimally debulked advanced ovarian cancer [7-11]. The Gynecologic Oncology Group (GOG) 172 trial [9] compared IV paclitaxel (135 mg/m2 over 24 hours, day 1) with either IP cisplatin (100 mg/m2, day 2) and IP paclitaxel (60 mg/m2, day 8) or IV cisplatin (75 mg/m2, day 2). The median PFS was 18 months in the IV arm and 24 months in the IP arm, and the absolute median OS benefit was 16 months (66 months versus 50 months, p=0.03) favoring the IP arm. The results of GOG 172 led to an National Cancaer Institute clinical announcement recommending that patients with optimally debulked FIGO stage III ovarian cancer should be considered for IP chemotherapy [12].
IP chemotherapy, however, is more toxic and inconvenient than IV chemotherapy. It causes more gastrointestinal toxicity, pain, fever and infection [13], and has the additional burden of an IP catheter with the consequent risk of catheter-related complications [10]. This toxicity was evident in the GOG 172 trial, where only 42% of patients completed all 6 cycles of IP chemotherapy due to toxicity and catheter-related complications.
The uptake of IP chemotherapy into routine clinical practice has been limited, perhaps reflecting clinicians' doubts about whether the benefits of IP chemotherapy outweigh its harms. There are no data regarding how patients or clinicians judge the trade-off between the potential survival benefits versus the additional toxicity and inconvenience of IP chemotherapy. Studies of preferences can quantify these judgements by determining the survival benefits needed to make the harms and inconveniences of a treatment worthwhile [14]. Patients with early breast and colon cancer generally consider small survival benefits (e.g., an extra 1 month survival time or an extra 1% survival rate) to make adjuvant IV chemotherapy worthwhile [15-18], but patients' preferences for adjuvant IP chemotherapy in advanced ovarian cancer have not been previously reported.
We conducted a single arm study of IP chemotherapy with a modified GOG 172 regimen of paclitaxel and cisplatin in women with optimally-debulked ovarian, peritoneal and fallopian tube cancers to assess the feasibility, toxicity, quality of life, and the survival benefits participating in women judged necessary to make the harms and inconveniences of IP chemotherapy worthwhile.
Women aged between 18 and 75 years were eligible for enrollment if they had FIGO stage III, optimally-debulked (residual disease ≤1 cm) ovarian cancer, primary peritoneal or fallopian tube cancers ('related cancers'), an IP catheter in-situ and were able to start IP chemotherapy within 6 weeks of their primary surgery. Eligible patients had to have an Eastern Cooperative Oncology Group (ECOG) performance score of 0 (fully active) to 2 (ambulatory and capable of self-care more than 50% of waking hours); adequate hematologic, renal and hepatic function; and a negative chest X-ray or computed tomography (CT) within 1 month of surgery.
The trial was conducted by the Australia New Zealand Gynaecologic Oncology Group and the National Health and Medical Research Council (NHMRC) Clinical Trials Centre, Sydney at 12 centers in Australia and New Zealand. Ethical approval was obtained by all centers and all participants provided written informed consent. Patients had an IP catheter inserted either during their primary debulking surgery, or as a second procedure following their surgery up to 6 weeks later. Patients were registered for the trial from 1 to 6 weeks after insertion of the IP catheter and began treatment within 1 week of registration.
The IP chemotherapy regimen was a modification of that used in the GOG 172 trial: IV paclitaxel 135 mg/m2 (over 3 hours) on day 1, IP cisplatin 75 mg/m2 on day 2, and IP paclitaxel 60 mg/m2 on day 8, all repeated 3-weekly for 6 cycles. Patients who were unable to complete all 6 cycles of IP chemotherapy could switch to IV chemotherapy to complete their total of 6 cycles. Dose delays and dose reductions for treatment toxicity were according to prespecified modifications.
Disease was assessed at baseline with history and physical examination, measurement of the serum concentration of cancer antigen 125 (CA-125), and an X-ray of the chest or CT chest within 1 month prior to surgery. CA-125 was repeated prior to each cycle of chemotherapy. After treatment, patients were reviewed at three months and then every 3 months for 2 years. Imaging was performed when clinically indicated.
Health-related quality of life (HRQL) was assessed by the Functional Assessment of Cancer Therapy-Ovary (FACT-O) [19] and the Patient Disease and Treatment Assessment Form (Pt DATA Form) [20]. Patients completed these questionnaires at baseline, on day 1 before each cycle of treatment, and then every 6 months for 2 years. The outcome measures were the FACT-O Trial Outcome Index (TOI) which includes the physical, functional, and ovarian sub-scales of the FACT-O; neurotoxicity, emotional, and social subscales of the FACT-O, and specific aspects of HRQL from the Pt DATA Form.
Preferences were assessed with a study-specific questionnaire. The questionnaire was based on a validated format using the time trade-off technique to determine the minimum improvements in survival time and in survival rates that participants judged sufficient to make IP chemotherapy worthwhile [17]. The questionnaire included 4 scenarios predicated on baseline survival times of 3 years and 5 years and baseline survival rates of 50% at 3 years and 5 years. The assessment of preferences was added to the study protocol 9 months after the trial opened. Preferences were elicited at baseline (before starting IP chemotherapy) and 9 months later (several months after completing IP chemotherapy).
The primary endpoint was the proportion of patients completing four or more cycles of IP chemotherapy. Secondary end-points were the proportion of patients experiencing grade 3 or worse toxicities [21], the proportion of patients stopping treatment due to catheter-related toxicities, PFS, and average scores for aspects of HRQL during and after treatment. PFS was measured from registration to progression, assessed using the Gynecologic Cancer Intergroup (GCIG) criteria for CA-125 progression and imaging, or to death for participants who died without evidence of progression; participants alive and progression-free at last follow-up were considered in remission [22].
The design and sample size were based on the premise that the regimen would be worth pursuing if the proportion of participants completing at least 4 cycles was 70% or higher, but not if it were 45% or lower. A minimum sample size of 35 patients was determined using Simon's two-stage optimum design with a type 1 error of 5% and a type two error of 10%, with an allowance of 5% for missing data.
Analyses of efficacy were by intention-to-treat and analyses of toxicity, safety and HRQL included all participants who received study treatment. Patients' preferences were described using the minimum extra survival benefit judged sufficient to make IP chemotherapy worthwhile in each of the 4 scenarios. Associations between preferences and baseline characteristics were assessed with Spearman's rank correlation. Reported p-values and confidence intervals are two-sided.
Thirty-nine patients were recruited over 26 months from June 2007 to December 2009. The median age was 54 years (range, 24 to 75 years), and median CA-125 at baseline was 124 U/mL (range, 12 to 2,261 U/mL). The median time from surgery to registration was 4 weeks, and from registration to the start of treatment was 1 week. One patient progressed prior to commencing treatment and was excluded from all analyses.
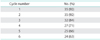
Twenty-seven of the 38 participants (71%; 95% confidence interval [CI], 55 to 83) met the primary feasibility endpoint by completing at least 4 cycles of IP chemotherapy; 24 patients (63%; 95% CI, 47 to 77) completed 6 cycles of chemotherapy (Table 1). Half of the participants completed 4 cycles and 11 patients (29%) completed 6 cycles without any dose modifications. The mean number of completed cycles by all patients was 4.7.
Dose modifications (delays, reductions, omissions) were required by 23 patients (61%). Table 2 reports the frequency of dose modifications required for the IP regimen. Cycles of chemotherapy were delayed due to hematologic toxicity (3% of total number of chemotherapy cycles), intraperitoneal complications (3%), and other causes (including peripheral venous access line infection, neuropathy, gastrointestinal toxicity, and constipation; 3%). Chemotherapy doses were reduced due to hematologic toxicity (8% of total number of chemotherapy cycles) and neurologic toxicity (5%). Chemotherapy was stopped prior to 6 cycles in 16 patients (42% of eligible patients) due to catheter-related complications (8 patients, 21%), toxicity (5 patients, 13%), and patient request (3 patients, 8%).
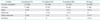
Table 3 reports the grade 3 or 4 toxicities experienced by all patients. Grade 3 or 4 gastrointestinal toxicities (nausea, vomiting, diarrhea, abdominal pain) occurred in 7 patients (19%). There was no grade 3 or 4 neuropathy, nephropathy or febrile neutropenia. There were 17 serious adverse events but no treatment-related deaths. Catheter-related complications occurred in 18 patients (47%) and included infection (2 patients, 5%), blockage (4 patients, 11%), leakage (8 patients, 21%), inability to access catheter (5 patients, 13%), and other such as abdominal pain, pain at catheter site, difficulty with needles, catheter removal (7 patients, 18%).
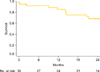
At a median follow-up of 25 months, 16 patients had developed progressive disease. Median PFS had not been reached. The PFS rate at 6 months was 0.92 (95% CI, 0.83 to 1.00) (Fig. 1).
Compliance for HRQL assessments was high whilst patients were on treatment (range, 89% to 90%), but lower during follow-up (48% to 58%). The mean on-treatment HRQL scores are reported in Table 4. With the exception of neurotoxicity, HRQL improved or was stable over time. The mean TOI (71 at baseline [95% CI, 66 to 76] to 85 at 12 months [95% CI, 79 to 91]) and emotional well-being (15 at baseline [95% CI, 14 to 16] to 18 at 12 months [95% CI, 16 to 21]) improved over time. Social/family well-being was stable over time (25 at baseline [95% CI, 24 to 26] to 25 at 12 months [95% CI, 23 to 26]). Neurotoxicity worsened from baseline (2.0 [95% CI, 1.2 to 2.8]) to 6 months after treatment (9.9 [95% CI, 5.2 to15]) and then improved but persisted at 12 months (7.3 [95% CI, 3.2 to 11]).
At baseline, the median survival benefits judged necessary to make IP chemotherapy worthwhile (n=20) were an extra 6 months beyond survival times of either 3 years or 5 years with IV chemotherapy and an extra 5% beyond survival rates of 50% at either 3 years or 5 years with IV chemotherapy (Fig. 2). The benefits judged sufficient by all patients ranged widely from as little as 1 day or 0.1% to as much as 15 years or 50%. Age was the only baseline characteristic associated with preferences: younger participants judged smaller benefits sufficient to make IP chemotherapy worthwhile (r=0.46, p=0.04). At 9 months, the median survival benefits judged necessary to make IP chemotherapy worthwhile (n=11) were an extra 1 month beyond survival times of either 3 years or 5 years with IV chemotherapy; and an extra 3% beyond survival rates of 50% at either 3 years or 5 years with IV chemotherapy. There was no significant difference between patients' preferences elicited at baseline and at 9 months (p=0.06 to 0.8).
Adjuvant IP chemotherapy in optimally debulked patients with advanced ovarian cancer has not been widely accepted despite its demonstrated survival benefits. Possible reasons for this include increased toxicity and inconvenience, catheter complications and the perception that patients would find these to be unacceptable and not worthwhile. We found that a modified IP regimen was feasible, tolerable, had acceptable HRQL and that most patients judged moderate survival benefits would make IP chemotherapy worthwhile.
Aspects of the design of the three large IP chemotherapy trials have been criticized and may have contributed to the slow uptake of IP chemotherapy into routine clinical practice. Alberts et al. [7] compared IV cyclophosphamide (600 mg/m2) and IP cisplatin (100 mg/m2) for 6 cycles with IV cyclophosphamide (600 mg/m2) and IV cisplatin (100 mg/m2) for 6 cycles in patients with maximally debulked stage III ovarian cancer. The control arm of this trial did not include paclitaxel and so is not consistent with current standard of care. Markman et al. [8] compared IV carboplatin (area under curve 9) every 28 days for 2 cycles followed by IP cisplatin (100 mg/m2) for 6 cycles with IV paclitaxel (135 mg/m2 over 24 hours) and IV cisplatin (75 mg/m2) for 6 cycles. The combination of high dose IV carboplatin and IP chemotherapy in the experimental arm makes it difficult to distinguish which of these was responsible for the OS benefit seen in this trial. The GOG 172 study [9] had the largest absolute OS benefit of all the trials, however, the dose and schedule of chemotherapy differed between the two arms. The cisplatin dose was 75 mg/m2 in the IV arm but 100 mg/m2 in the IP arm. Paclitaxel was given on day 8 in the IP arm, but not the IV arm. The GOG 172 IP chemotherapy regimen was also much more toxic and inconvenient making many clinicians reluctant to use this IP regimen in clinical practice.
We used a modified version of the IP chemotherapy regimen from GOG 172 in our study, to improve its convenience and tolerability and for consistency with the practice of other gyneoncology groups [23]. The IV paclitaxel was shortened from a 24-hour infusion to a 3-hour infusion [24] and the IP cisplatin dose was reduced from 100 mg/m2 to 75 mg/m2. No changes were made to the IP paclitaxel.
The modified regimen was feasible with 71% of patients completing at least 4 cycles of treatment and 63% of patients completing 6 cycles of treatment. These results are better than the GOG 172 trial (52% completed at least 4 cycles and 42% of patients completed 6 cycles) and similar to a recently published single-institution retrospective study using the same modified regimen (80% of patients completed at least 4 cycles and 55% completed 6 cycles) [25].
The modified regimen was reasonably well tolerated. All grade 3 or 4 toxicities occurred less frequently than in the GOG 172 trial. There was no grade 3 or 4 neurotoxicity in our study, a major dose-limiting and HRQL concern when cisplatin and paclitaxel are used in the same chemotherapy regimen. Like in GOG 172, however, catheter-related complications were frequent (18 patients, 47%) and were the most frequent cause of early discontinuation of treatment (8 patients, 21%) despite our efforts to prevent catheter-related complications through education and training workshops prior to opening the study. Rates of catheter-related complications should improve as centers gain more experience in administering IP chemotherapy [26,27].
The mean on-treatment scores of patients' HRQL were skewed towards better HRQL and generally improved or were stable over time. Neurotoxicity, however, deteriorated during treatment and persisted at a level worse than baseline at 12 months, and this was similar to the HRQL results from the GOG 172 trial [28]. This likely reflects the chronicity of chemotherapy-induced neurotoxicity in a distinct proportion of patients. Hair loss was rated as the most troublesome specific aspect of HRQL, a reminder to clinicians that toxicities that they might consider to be 'less-serious' may matter the most to patients.
Most patients judged moderate survival benefits judged necessary to make adjuvant IP chemotherapy worthwhile (an extra 6 months and an extra 5%) although the preferences of all patients varied widely across the range of possible benefits, and age was the only predictor of preferences. These results suggest that it is difficult to know an individual patient's preferences for IP chemotherapy without specifically eliciting them during the decision-making process. Patients' judged larger benefits for IP chemotherapy in the present study than those judged by patients for adjuvant chemotherapy in our previous breast cancer and colon cancer studies using similar methodology [17,18]. Reasons for these differences include the additional toxicity and inconvenience of IP chemotherapy, the overall worse prognosis of patients with advanced ovarian cancer, and methodological reasons such as the timing of elicitation of patients' preferences [29]. The main limitation of these preference data was the small numbers (n=20 before, n=11 after) and consequent low power for detecting predictors of preferences and any changes over time.
Strengths of our study include demonstrating that it was feasible to administer the modified IP regimen on an outpatient basis. The limitations of our study are that it was a small, non-randomized, phase II trial that established the feasibility and tolerability, but not the efficacy, of the modified IP chemotherapy regimen. The efficacy of the regimen needs to be investigated in a randomized, phase III trial and indeed this regimen is now being used by the GOG in their current trials (e.g., GOG 252).
More generally, it is uncertain how IP chemotherapy fits into the current first-line systemic treatment landscape for patients with advanced ovarian cancer. Other available options include neoadjuvant IV chemotherapy [30], the addition of bevacizumab to IV chemotherapy [31,32], and dose-dense IV chemotherapy [33,34], all of which do not require the additional care and expertise of an IP catheter. The difficulty for clinicians is that these approaches have not been directly compared in randomized, phase III clinical trials. In addition to patient and disease factors, it is likely that first-line treatment selection will be influenced by clinicians' experiences with each approach, funding of more expensive drugs, and, ideally, patients' preferences for the treatments.
We recently surveyed all the major gynecologic cancer centers throughout Australia to determine how many centers were using IP chemotherapy and the approximate number of patients treated with IP chemotherapy over the last year. An email survey was sent to the head of each gynecologic cancer centers (n=14) and to the corresponding lead medical oncologist. The response rate was 85% (25/30) with 3 incomplete responses. Half the centers recommended IP chemotherapy to optimally debulked patients. The number of patients treated in the last year ranged from 2 to 20. Almost all patients were treated in tertiary hospital and not in regional or rural settings. The most common reasons for not offering IP chemotherapy routinely to all patients were concerns about toxicity of the treatment and logistical reasons. Many centers were quite selective in whom they offered IP chemotherapy to and based decisions on a patient's age, extent of surgery, predicted toxicity and their treatment preferences. Of those sites that used IP chemotherapy, all but one used the modified IP regimen used in our study with the remaining center using the GOG172 protocol. The most common reasons for not using IP chemotherapy were concerns about the superiority of IP chemotherapy, logistics of offering IP chemotherapy, and that 'dose-dense' intravenous chemotherapy was a better alternative. Most of the centers not using IP chemotherapy were using dose dense chemotherapy based on the Japanese Gynecologic Oncology Group (JGOG) protocol [33].
In conclusion, a modified IP chemotherapy regimen was feasible and tolerable, apart from neurotoxicity HRQL which remains an important survivorship issue. IP catheter-related complications were high despite training and reflect limited experience with IP chemotherapy. Patients' preferences for IP chemotherapy should be elicited during the decision-making process as it is apparent many patients are prepared to accept potentially more toxic regimens for a relatively modest increase in survival. Substudies of patients' preference should arguably be included in all randomized trials comparing different treatment regimens because they can help determine acceptability and likely uptake of the regimens.
Figures and Tables
Fig. 2
Cumulative proportions of patients considering whether intraperitoneal (IP) chemotherapy would be worthwhile for various improvements in (A) survival times of 3 and 5 years and (B) survival rates of 50% at 3 years and 5 years (n=20).

References
1. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011; 61:69–90.
2. American Joint Committee on Cancer. AJCC cancer staging manual. 7th ed. New York: Springer;2010.
3. du Bois A, Luck HJ, Meier W, Adams HP, Mobus V, Costa S, et al. A randomized clinical trial of cisplatin/paclitaxel versus carboplatin/paclitaxel as first-line treatment of ovarian cancer. J Natl Cancer Inst. 2003; 95:1320–1329.
4. Ozols RF, Bundy BN, Greer BE, Fowler JM, Clarke-Pearson D, Burger RA, et al. Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a Gynecologic Oncology Group study. J Clin Oncol. 2003; 21:3194–3200.
5. Bookman MA, Brady MF, McGuire WP, Harper PG, Alberts DS, Friedlander M, et al. Evaluation of new platinum-based treatment regimens in advanced-stage ovarian cancer: a Phase III Trial of the Gynecologic Cancer Intergroup. J Clin Oncol. 2009; 27:1419–1425.
6. Cannistra SA. Cancer of the ovary. N Engl J Med. 2004; 351:2519–2529.
7. Alberts DS, Liu PY, Hannigan EV, O'Toole R, Williams SD, Young JA, et al. Intraperitoneal cisplatin plus intravenous cyclophosphamide versus intravenous cisplatin plus intravenous cyclophosphamide for stage III ovarian cancer. N Engl J Med. 1996; 335:1950–1955.
8. Markman M, Bundy BN, Alberts DS, Fowler JM, Clark-Pearson DL, Carson LF, et al. Phase III trial of standard-dose intravenous cisplatin plus paclitaxel versus moderately high-dose carboplatin followed by intravenous paclitaxel and intraperitoneal cisplatin in small-volume stage III ovarian carcinoma: an intergroup study of the Gynecologic Oncology Group, Southwestern Oncology Group, and Eastern Cooperative Oncology Group. J Clin Oncol. 2001; 19:1001–1007.
9. Armstrong DK, Bundy B, Wenzel L, Huang HQ, Baergen R, Lele S, et al. Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med. 2006; 354:34–43.
10. Jaaback K, Johnson N, Lawrie TA. Intraperitoneal chemotherapy for the initial management of primary epithelial ovarian cancer. Cochrane Database Syst Rev. 2011; (11):CD005340.
11. Hess LM, Benham-Hutchins M, Herzog TJ, Hsu CH, Malone DC, Skrepnek GH, et al. A meta-analysis of the efficacy of intraperitoneal cisplatin for the front-line treatment of ovarian cancer. Int J Gynecol Cancer. 2007; 17:561–570.
12. Cancer Therapy Evaluation Program. NCI clinical announcement on intraperitoneal therapy for ovarian cancer [Internet]. Cancer Therapy Evaluation Program;2006. cited 2012 Jul 28. Available from: http://ctep.cancer.gov/highlights/20060105_ovarian.htm.
13. Australian Institute of Health and Welfare. Australian cancer incidence and mortality (ACIM) books [Internet]. Canberra: Australian Institute of Health and Welfare;2012. cited 2013 Aug 7. Available from: http://www.aihw.gov.au/acim-books/.
14. Blinman P, King M, Norman R, Viney R, Stockler MR. Preferences for cancer treatments: an overview of methods and applications in oncology. Ann Oncol. 2012; 23:1104–1110.
15. Slevin ML, Stubbs L, Plant HJ, Wilson P, Gregory WM, Armes PJ, et al. Attitudes to chemotherapy: comparing views of patients with cancer with those of doctors, nurses, and general public. BMJ. 1990; 300:1458–1460.
16. Duric V, Stockler M. Patients' preferences for adjuvant chemotherapy in early breast cancer: a review of what makes it worthwhile. Lancet Oncol. 2001; 2:691–697.
17. Blinman P, Duric V, Nowak AK, Beale P, Clarke S, Briscoe K, et al. Adjuvant chemotherapy for early colon cancer: what survival benefits make it worthwhile? Eur J Cancer. 2010; 46:1800–1807.
18. Duric VM, Stockler MR, Heritier S, Boyle F, Beith J, Sullivan A, et al. Patients' preferences for adjuvant chemotherapy in early breast cancer: what makes AC and CMF worthwhile now? Ann Oncol. 2005; 16:1786–1794.
19. Basen-Engquist K, Bodurka-Bevers D, Fitzgerald MA, Webster K, Cella D, Hu S, et al. Reliability and validity of the functional assessment of cancer therapy-ovarian. J Clin Oncol. 2001; 19:1809–1817.
20. Stockler MR, O'Connell R, Nowak AK, Goldstein D, Turner J, Wilcken NR, et al. Effect of sertraline on symptoms and survival in patients with advanced cancer, but without major depression: a placebo-controlled double-blind randomised trial. Lancet Oncol. 2007; 8:603–612.
21. Cancer Therapy Evaluation Program. Common terminology criteria for adverse events v3.0 (CTCAE) [Internet]. Cancer Therapy Evaluation Program;2006. cited 2013 Aug 7. Available from: http://http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf.
22. Rustin GJ. Use of CA-125 to assess response to new agents in ovarian cancer trials. J Clin Oncol. 2003; 21:10 Suppl. 187s–193s.
23. Fujiwara K. Three ongoing intraperitoneal chemotherapy trials in ovarian cancer. J Gynecol Oncol. 2012; 23:75–77.
24. Eisenhauer EA, ten Bokkel Huinink WW, Swenerton KD, Gianni L, Myles J, van der Burg ME, et al. European-Canadian randomized trial of paclitaxel in relapsed ovarian cancer: high-dose versus low-dose and long versus short infusion. J Clin Oncol. 1994; 12:2654–2666.
25. Barlin J, Dao F, Zgheib NB, Ferguson S, Sabbatini P, Hensley M, et al. Progression-free and overall survival of a modified outpatient regimen of primary intravenous/intraperitoneal paclitaxel and intraperitoneal cisplatin is comparable to results from GOG 172. Gynecol Oncol. 2012; 125:Suppl 1. S36–S37.
26. Barlin JN, Dao F, Zgheib NB, Ferguson SE, Sabbatini PJ, Hensley ML, et al. Progression-free and overall survival of a modified outpatient regimen of primary intravenous/intraperitoneal paclitaxel and intraperitoneal cisplatin in ovarian, fallopian tube, and primary peritoneal cancer. Gynecol Oncol. 2012; 125:621–624.
27. Bunting M, Chan W, Brand A, Blomfield P. Intraperitoneal chemotherapy for advanced epithelial ovarian malignancy: lessons learned. Aust N Z J Obstet Gynaecol. 2009; 49:667–671.
28. Wenzel LB, Huang HQ, Armstrong DK, Walker JL, Cella D. Gynecologic Oncology Group. Health-related quality of life during and after intraperitoneal versus intravenous chemotherapy for optimally debulked ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol. 2007; 25:437–443.
29. Stiggelbout AM, de Haes JC. Patient preference for cancer therapy: an overview of measurement approaches. J Clin Oncol. 2001; 19:220–230.
30. Vergote I, Trope CG, Amant F, Kristensen GB, Ehlen T, Johnson N, et al. Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. N Engl J Med. 2010; 363:943–953.
31. Burger RA, Brady MF, Bookman MA, Fleming GF, Monk BJ, Huang H, et al. Incorporation of bevacizumab in the primary treatment of ovarian cancer. N Engl J Med. 2011; 365:2473–2483.
32. Perren TJ, Swart AM, Pfisterer J, Ledermann JA, Pujade-Lauraine E, Kristensen G, et al. A phase 3 trial of bevacizumab in ovarian cancer. N Engl J Med. 2011; 365:2484–2496.
33. Katsumata N, Yasuda M, Takahashi F, Isonishi S, Jobo T, Aoki D, et al. Dose-dense paclitaxel once a week in combination with carboplatin every 3 weeks for advanced ovarian cancer: a phase 3, open-label, randomised controlled trial. Lancet. 2009; 374:1331–1338.
34. Katsumata N, Yasuda M, Isonishi S, Takahashi F, Michimae H, Kimura E, et al. Long-term results of dose-dense paclitaxel and carboplatin versus conventional paclitaxel and carboplatin for treatment of advanced epithelial ovarian, fallopian tube, or primary peritoneal cancer (JGOG 3016): a randomised, controlled, open-label trial. Lancet Oncol. 2013; 14:1020–1026.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download