Abstract
Objective
The purpose of the present study was to evaluate treatment outcomes and prognostic factors in cervical cancer patients with isolated para-aortic lymph node (PALN) metastases. We especially tried to evaluate PALN factors such as size, site and number.
Methods
From August 1994 to December 2009, 40 cervical cancer patients with isolated PALN node metastases at initial diagnosis were selected for analysis. Patients underwent both extended field external beam and intracavitary brachytherapy. Fourteen patients received 5-fluorouracil and cisplatin (FP) and 16 patients received weekly concurrent cisplatin. Information of PALN, such as size, site, and number, was founded before PALN radiotherapy.
Results
The median follow-up time after primary treatment was 28.5 months (range, 2 to 213 months). The 3-year overall and progression-free survival rate after primary treatment was 44.3% and 31.3%, respectively. In multivariate analysis including tumor stage, performance status, and chemotherapy, FP regimen concurrent chemoradiotherapy was more effective than radiotherapy alone (p=0.030). The 3-year progression-free survival rate was 41.9% and 11.1% in patients with PALN numbers of ≤1 and ≥2, respectively (p=0.008). The 3-year progression-free survival rate was 42.1% and 19.2% in patients with PALN size of <1.5 cm and ≥1.5 cm, respectively (p=0.031).
Conclusion
The radiologic features of PALN, such as number or size, can be used to determine prognosis in PALN metastatic cervical cancer patients. Furthermore, FP regimen concurrent chemoradiotherapy was associated with better patient survival than radiotherapy alone. However, more studies are required to confirm possible different treatment outcomes between FP and weekly cisplatin regimens.
Although cervical cancer is curable after definitive treatment, it is still the major cause of cancer death in women worldwide [1]. The prognosis is worse in patients with distant metastases and the para-aortic lymph node (PALN) is frequently observed as a metastatic site. Although it has been classified as stage IVB according to the International Federation of Gynecology and Obstetrics (FIGO) staging system, the para-aortic region is a small area and localized treatment is possible. The 2013 National Comprehensive Cancer Network (NCCN) guideline recommends cisplatin based chemotherapy with PALN extended field radiation therapy (RT) in patients presenting with isolated PALN metastases [2].
Cervical cancer has been reported to spread more widely by the lymphatic pathway than by the hematogenous pathway [3]. The PALN may be an important prognostic factor, but studies about the correlation between treatment outcome and PALN factors are rare. The aim of the present study was to analyze the correlation between prognosis and PALN factors after definitive RT with or without chemotherapy in cervical cancer patients with isolated PALN metastases. Failure pattern and treatment outcomes were also analyzed.
From August 1994 to December 2009, 935 patients with cervical cancer were treated in the Department of Radiation Oncology. Among 935 patients, 240 were treated in adjuvant setting after surgery. Forty patients with isolated PALN node metastases at initial diagnosis were selected for analysis. Median age was 48.5 years (range, 28 to 78 years). Patient characteristics are listed in Table 1.
The external beam RT was delivered using 10-15MV photons. The delivered radiation dose to PALN was 44.2 Gy (range, 32.4 to 53 Gy), given at a dose of 1.7-2.0 Gy per fraction. In 6 patients, RT field was modified at a dose of 40-45 Gy depending on tumor response and tolerance. Patients underwent both extended field external beam RT and high dose rate intracavitary brachytherapy. The median radiation dose to the whole pelvis was 55 Gy and midline block was applied at a dose of 36-45 Gy depending on reduction of tumor size. HDR brachytherapy (Iridium-192, Microselectron, Nucletron, Veenendaal, Netherlands) was applied with point A dose of median 24 Gy (4 or 5 Gy per fractions, twice a week). The upper border of radiation field was extended as high as the T12 or L1 vertebra. Thirty-two patients received chemotherapy. Fourteen patients received 2-4 cycles of cisplatin (75 mg/m2) and 5-fluorouracil (5-FU, 1,000 mg/m2) during and after RT. Sixteen patients received weekly concurrent cisplatin (40 mg/m2) for a total 4-6 cycles. Seven patients were found to have PALN metastases in a radical hysterectomy with PALN biopsy and received postoperative extended field irradiation.
The patients' follow-up consisted of the following: every 1-3 months during the first year, and every 3-6 months thereafter. The primary cervix was evaluated by pelvic exam and pap smear. The PALN was evaluated mostly by follow-up computed tomography (CT). Although positron emission tomography (PET) CT has been used often since 2000 in our institution, it was applied widely at diagnosis and follow-up since 2008. A complete response (CR) and partial response of PALN was defined as the complete disappearance and decrease in tumor diameter exceeding 50% of the visible node in the follow-up CT.
In 32 patients, information of PALN, such as size, site, and number, was found through MRI or CT before PALN RT. Although all patients underwent radiologic study such as MRI or CT before treatment, it was impossible to gain detailed information of radiologic study in 8 patients because old radiologic image data was discarded. PALN ≥1 cm in CT or MRI was counted and location was classed as vertebra level. The longest diameter of PALN was measured on the CT or MRI.
Examinations of tumor markers, such as squamous cell carcinoma antigen (SCC Ag) and Cyfra 21-1, were performed regularly before and after primary treatment. Analysis of SCC Ag and Cyfra 21-1 was excluded in patients with adenocarcinoma. Toxicity was evaluated with use of the Radiation Therapy Oncology Group and the European Organization for Research and Treatment of Cancer [4].
Overall survival (OS) after primary treatment was the primary end point of this study. OS was calculated from the date of radiotherapy initiation until the date of death or the last follow-up. Progression-free survival (PFS) was calculated from the date of radiotherapy initiation until the date of occurrence of disease progression or death. The disease progression was evaluated with imaging, pap smear, and clinical examination. Failure was defined as either disease progression or recurrence of disease. The Kaplan-Meier estimator was used to derive estimates of survival rates. Log-rank tests and the Cox proportional hazard model were used to compare each prognostic factors. A p<0.05 was considered statistically significant. All statistical analyses were performed with IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA).
The median follow-up time after primary treatment was 28.5 months (range, 2 to 213 months). In five patients, no study was performed to find recurrent sites, and one patient died soon after completion of concurrent chemoradiotherapy (CCRT). Twenty-three of 34 patients were found to have treatment failure. On initial failure, three patients relapsed only in pelvis while 13 patients experienced distant metastases only. Both pelvic and distant metastases were found in seven patients (Table 2). The supra-clavicular lymph node (SCLN), lung, and PALN were involved in eight, five, and five patients, respectively. Of these, isolated SCLN recurrence occurred in three patients. The in-RT-field control rate was 78.1% at first year, and 48.1% at third year. The out-RT-field control rate was 42.4% at first year, and 38.7% at third year.
After PALN RT, CT was performed during follow-up in 32 patients to evaluate PALN treatment response. CR and non-CR were found in 18 and 14 patients, respectively. Primary cervical mass was evaluated by pelvic exam in all patients. CR and non-CR were found in 27 and 13 patients, respectively. Thirty-five patients were evaluated by pap smear with 34 patients showing no evidence of disease.
Acute maximum toxicity was grade 3 in four patients, and grade 4 in two patients. Hematologic toxicity occurred in three patients and all patients received cisplatin and 5-FU CCRT. Genitourinary toxicity was found in three patients. One patient expired soon after completion of CCRT due to septic shock following pneumonia and urinary tract infection. The patient had grade 2 leukopenia during treatment and treatment response was good. Pelvic RT was held at 44.2 Gy due to poor performance. Grade 2 upper gastrointestinal toxicity was found in 14 patients. No patients had severe gastrointestinal toxicity.
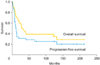
The 3-year OS and PFS rate after primary treatment was 44.3% (median, 29 months) and 31.3% (median, 11 months), respectively (Fig. 1). Prognostic factors for OS and PFS are shown in Table 3. Variables analyzed included chemotherapy, Eastern Cooperative Oncology Group (ECOG) performance status, tumor stage, tumor marker and PALN factors. The 3-year OS rate was 70.7%, 31.3%, and 37.5% in patients who received 5-fluorouracil and cisplatin (FP), weekly cisplatin, and RT alone, respectively (p=0.028). The 3-year OS rate was 63.5%, 46.2%, and 23.1% at a SCC Ag level of <6, 6-30, and >30 ng/mL, respectively (p=0.048). The 3-year OS rate was 56.3% and 16.7% in patients with an ECOG performance status of 0/1 and 2, respectively (p=0.006). The 3-year OS rate was 56.3%, 46.7%, 66.7%, and 11.1% in patients with tumor stage I, II, III, and IVA, respectively (p=0.009). Significant prognostic factors are listed in Table 3. Operation (p=0.068), parametrial involvement (p=0.085), cervical mass size (p=0.142), and Cyfra 21-1 (p=0.200) were not statistically significant. In multivariate analysis including tumor stage, ECOG performance status, and chemotherapy, FP regimen CCRT was more effective than RT alone (relative risk [RR]=4.0, p=0.030). The difference between FP and weekly cisplatin regimen was not statistically significant due to poor performance status in weekly cisplatin patients (RR=2.8, p=0.108). In univariate analysis for PFS, only ECOG performance status was statistically significant (p=0.025).
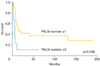
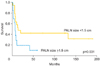
Regarding PALN factors, the number of PALNs was shown to correlate with OS. The 3-year OS rate was 55.4% and 22.2% with a PALN number of ≤ 1 and ≥ 2, respectively (p=0.044). The number and size of PALN were shown to correlate with PFS. The 3-year PFS rate was 41.9% and 11.1% in patients with PALN numbers of ≤1 and ≥2, respectively (p=0.008) (Fig. 2). The 3-year PFS rate was 42.1% and 19.2% in patients with PALN of <1.5 cm and ≥1.5 cm, respectively (p=0.031) (Fig. 3). The location and treatment response of PALN were not prognostic for OS and PFS (Table 4). In multivariate analysis including the number, size, and ECOG performance status, only the number of PALNs was statistically significant (RR=2.0, p=0.025).
The lymphatic metastatic route is more dominant than the hematogenous route in cervical cancer [3]. The PALN may be a valuable prognostic factor for survival or disease progression in patients with PALN metastases. The presented study analyzed the outcome and prognostic factors after definitive radiotherapy in cervical cancer with isolated metastatic PALN. We especially tried to find the correlation between disease progression and radiologic features of the PALN such as size, site, number, and treatment response.
Singh et al. [5] reported the correlation between number of PALN and survival in 14 isolated PALN recurrent cervical cancer patients and found it to be significant (p=0.02). They also reported no correlation between PALN diameter and survival. Rajasooriyar et al. [6] reported the number of nodes seems to be an independent predictor of relapse in 39 patients with common iliac or PALN metastases (p=0.046). The 5-year relapse-free rate was 34.5% among the patients with 1 to 3 involved nodes and 5.3% for patients with ≥4 involved node. In our study, we enrolled patients initially presenting with isolated PALN metastases and found a correlation between PALN number and disease progression (p=0.008). PALN size also correlated with disease progression (p=0.031). This implies that PALN factors are also valuable in patients initially presenting as well as recurrent patients. Treatment response of PALN showed no correlation with survival and treatment failure. It is possible that visible PALN after RT may be deactivated debris and PET-CT may help to discriminate the activity of PALN in these patients. In most patients, the PALN was located at level 3 and/or 4 of the lumbar vertebra, so we classified sites into ≥ level 3 and ≤ level 4. We could find no correlation between PALN location and survival.
In the Gynecologic Oncology Group (GOG) study [7], 95 patients with stage I-IVA cervical carcinoma and PALN metastases were analyzed. Histologic or cytologic confirmation of metastases to the PALN was performed. Recurrence was observed in 64.0% after FP regimen CCRT. As the cause of initial recurrence, distant metastases only and pelvis only were noted in 31.4% and 20.9% patients, respectively. There was no follow-up due to absence of reliable methods to assess PALN. In the Radiation Therapy Oncology Group (RTOG) study [8], 30 patients with clinical Stage I-IV carcinoma of the cervix with biopsy-proven PALN metastases were analyzed. The locoregional control rate and probability of disease failure was 50% and 63% at 3 years, respectively. This result was similar with our study recurrence rate of 67.6%. As first failure site, out-RT-field failure only was more frequent than in-RT-field failure only. In 14 patients who were treated by FP regimen CCRT, recurrence was noted in 57.1% of patients.
In the RTOG study [8], the median OS of cervical cancer with metastatic PALN was 23 months after FP regimen CCRT. The 3-year and 4-year OS rate were 33% and 29%, respectively. In the GOG study [7], the 3-year OS and median OS were 39% and 27.1 months after FP regimen CCRT. In our study, 32 and eight patients were treated by CCRT and RT alone, respectively. The survival outcome was similar with our study. The median, 3-year, and 5-year OS rate were 29 months, 44.3%, and 39.1%, respectively. Recently, some studies reported comparisons of monthly FP and weekly cisplatin CCRT in locally advanced cervical cancer [9,10]. They reported similar survival and better tolerance in weekly cisplatin. However, there has been no report in PALN metastatic cervical cancer. In univariate analysis of our study, FP regimen CCRT was associated with better survival in patients than weekly cisplatin regimen CCRT or RT alone (p=0.028). Because patients with worse performance and advanced disease were treated by RT alone or weekly cisplatin, we performed multivariate analysis of tumor stage, ECOG performance status, and chemotherapy. In multivariate analysis, FP regimen CCRT was more effective than RT alone and statistically significant (RR=4.0, p=0.030). FP regimen CCRT also showed better outcome than weekly cisplatin regimen CCRT. However, it was not statistically significant due to poor performance status in weekly cisplatin patients (RR=2.8, p=0.108). Although previous studies reported similar outcomes between FP and weekly cisplatin regimen CCRT in locally advanced cervical cancer, more studies in PALN metastatic cervical cancer are needed.
Zighelboim et al. [11] reported that the use of radiotherapy and multi-agent chemotherapy in patients with stage IVB cervical cancer and good performance status were well tolerated and resulted in higher survival rates. The 2013 NCCN guideline also recommends cisplatin based chemoradiation therapy in isolated PALN metastatic cervical cancer [2]. In our study, ECOG performance 0/1 was a statistically significant prognostic factor (p=0.006). However, in multivariate analysis including tumor stage, ECOG performance status, and chemotherapy, ECOG performance was not statistically significant (p=0.796).
Micke et al. [12] reported that the SCC Ag level correlated with prognosis in patients with cervical carcinoma treated with radiotherapy or chemoradiotherapy. Hong et al. [13] reported that SCC Ag levels higher than 10 ng/mL is an independent predictor for poor prognosis. In our study, SCC Ag was a statistically significant prognostic factor (p=0.048). Generally, SCC Ag and Cyfra 21-1 are both evaluated before and after treatment in our institution. Although Cyfra 21-1 was not statistically significant (p=0.200) in this study, normal SCC Ag and increased Cyfra 21-1 were checked in four patients. It appears that Cyfra 21-1 can be used as an adjuvant for SCC Ag.
Present study has a limitation of small group of patients from one institution with various treatment modalities due to patients' condition over the years. However, this study confirmed long-term progression free survival rate of over 30% in patients with PALN metastasis at presentation. Notably, patients with smaller sized or single PALN metastasis showed better survival as long as primary tumor control was achieved.
In Summary, the radiologic features of PALN metastasis, such as involved number of nodes or nodal size, can be a prognostic factor in patients with cervical cancer who has PALN metastasis at presentation. Furthermore, concurrent chemo-radiotherapy was associated with good long-term progression free survival with tolerable side effects. The results from current study suggest that early detection of PALN involvement with advanced radiologic studies is important for better survival even with metastatic disease based on recent FIGO staging system.
References
1. Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001; 94:153–156.
2. National Comprehensive Cancer Network (NCCN). NCCN clinical practice guidelines in Oncology [Internet]. Fort Washington, PA: NCCN;2013. cited 2013 May 20. Available from: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
3. Sakurai H, Mitsuhashi N, Takahashi M, Akimoto T, Muramatsu H, Ishikawa H, et al. Analysis of recurrence of squamous cell carcinoma of the uterine cervix after definitive radiation therapy alone: patterns of recurrence, latent periods, and prognosis. Int J Radiat Oncol Biol Phys. 2001; 50:1136–1144.
4. Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995; 31:1341–1346.
5. Singh AK, Grigsby PW, Rader JS, Mutch DG, Powell MA. Cervix carcinoma, concurrent chemoradiotherapy, and salvage of isolated paraaortic lymph node recurrence. Int J Radiat Oncol Biol Phys. 2005; 61:450–455.
6. Rajasooriyar C, Van Dyk S, Bernshaw D, Kondalsamy-Chennakesavan S, Barkati M, Narayan K. Patterns of failure and treatment-related toxicity in advanced cervical cancer patients treated using extended field radiotherapy with curative intent. Int J Radiat Oncol Biol Phys. 2011; 80:422–428.
7. Varia MA, Bundy BN, Deppe G, Mannel R, Averette HE, Rose PG, et al. Cervical carcinoma metastatic to para-aortic nodes: extended field radiation therapy with concomitant 5-fluorouracil and cisplatin chemotherapy: a Gynecologic Oncology Group study. Int J Radiat Oncol Biol Phys. 1998; 42:1015–1023.
8. Grigsby PW, Heydon K, Mutch DG, Kim RY, Eifel P. Long-term follow-up of RTOG 92-10: cervical cancer with positive para-aortic lymph nodes. Int J Radiat Oncol Biol Phys. 2001; 51:982–987.
9. Kim YS, Shin SS, Nam JH, Kim YT, Kim YM, Kim JH, et al. Prospective randomized comparison of monthly fluorouracil and cisplatin versus weekly cisplatin concurrent with pelvic radiotherapy and high-dose rate brachytherapy for locally advanced cervical cancer. Gynecol Oncol. 2008; 108:195–200.
10. Kong TW, Chang SJ, Paek J, Yoo SC, Yoon JH, Chang KH, et al. Comparison of concurrent chemoradiation therapy with weekly cisplatin versus monthly fluorouracil plus cisplatin in FIGO stage IIB-IVA cervical cancer. J Gynecol Oncol. 2012; 23:235–241.
11. Zighelboim I, Taylor NP, Powell MA, Gibb RK, Rader JS, Mutch DG, et al. Outcomes in 24 selected patients with stage IVB cervical cancer and excellent performance status treated with radiotherapy and chemotherapy. Radiat Med. 2006; 24:625–630.
12. Micke O, Bruns F, Schafer U, Prott FJ, Willich N. The impact of squamous cell carcinoma (SCC) antigen in patients with advanced cancer of uterine cervix treated with (chemo-)radiotherapy. Anticancer Res. 2005; 25:1663–1666.
13. Hong JH, Tsai CS, Chang JT, Wang CC, Lai CH, Lee SP, et al. The prognostic significance of pre- and posttreatment SCC levels in patients with squamous cell carcinoma of the cervix treated by radiotherapy. Int J Radiat Oncol Biol Phys. 1998; 41:823–830.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download