Abstract
Objective
To analyze patterns of abdominopelvic failures and to define subgroups for the use of adjuvant radiotherapy in the International Federation of Gynecology and Obstetrics (FIGO) stage III epithelial ovarian cancer (EOC).
Methods
We reviewed 149 patients treated with debulking surgery followed by intravenous taxane and platinum chemotherapy between 1999 and 2008. Patient characteristics, patterns of failure, abdominopelvic failure APF-free survival (APFFS) and overall survival (OS) were analyzed.
Results
The median age of the patients was 51 years. Thirty-two patients (21.5%) were found to have residuum >2 cm after surgery. The median pretreatment CA-125 was 604 and 54.4% of patients had a decline in CA-125 ≥90% between pretreatment and at postoperative 1 month. With a median follow-up of 50 months, 79 patients (53.0%) experienced abdominopelvic failure (APF). The 5-year APF-free survival rate was 41.1%. Lymph node metastasis, size of residual disease, and decline in CA-125 were found to be significant prognostic factors for APF upon multivariate analysis. The group of patients in whom abdominopelvic irradiation was indicated as definitive postoperative treatment comprised 55% of the overall patient population and their 5-year survival rate was 68%.
Conclusion
The stratification was suggested to predict APF based on lymph node metastasis, size of residual tumor, and decline in CA-125. Adjuvant radiotherapy covering the whole abdominopelvis using the intensity modulation technique may be considered to reduce APF in FIGO stage III EOC patients with intermediate risk.
The standard management of advanced epithelial ovarian cancer (EOC) is staging laparotomy with resection of gross disease, followed by first-line adjuvant chemotherapy composed of intravenous (IV) taxane and a platinum-based regimen. Even though cytoreductive surgery and adjuvant IV chemotherapy have achieved a considerably high clinical complete response rate (up to 50%), many responding patients suffer from abdominopelvic failures (APF) with a median progression-free survival of 15.5-22 months [1-3]. Unfortunately, patients with macroscopic residual disease or APF after initial treatment usually cannot maintain disease-free status in spite of further chemotherapy. Therefore, effective adjuvant locoregional treatment to consolidate or maintain the response achieved by maximal debulking surgery and adjuvant IV chemotherapy is required for patients at a high risk for APF [4].
Whole abdominal radiotherapy (WART) has also been used as consolidation treatment after cytoreductive surgery and adjuvant chemotherapy, but its clinical significance has been controversial [5]. Even though many studies have suggested a possible benefit of WART for patients with tumors in complete pathologic remission or with minimal residual disease, the therapy has some limitations that prevent it from being adopted as one of the standard treatment modalities for advanced stage EOC. The purpose of this study was to analyze patterns of APF in International Federation of Gynecology and Obstetrics (FIGO) stage III EOC patients treated with cytoreductive surgery and intravenous adjuvant taxane-platinum chemotherapy and to define subgroups for which WART will be beneficial as a consolidation therapy.
Between 1999 and 2008, a total of 572 women were pathologically diagnosed with epithelial ovarian malignancy at Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. Among them, 325 patients had proven FIGO stage III EOC, and 176 of them were excluded because of intraperitoneal taxane and platinum-based chemotherapy (n=79), neoadjuvant chemotherapy before surgery (n=21), double primary malignancy (n=15), postoperative adjuvant radiotherapy (n=14), loss to follow-up (n=14), or second-look operation (n=1). Therefore, 149 patients were eligible for this analysis.
Patients who were suspected to have ovarian malignancy underwent a thorough history and full physical and pelvic examination. Complete blood count, chemistries, urinalysis and chest X-rays were also routinely evaluated. Pelvic ultrasound was initially used to evaluate a suspicious adnexal mass. To identify tumor extent, abdominopelvic computed tomography (CT), magnetic resonance imaging or positron emission tomography (PET), or PET/CT were analyzed. Patients with clinical indication were further examined with mammography, upper gastrointestinal endoscopy, or colonoscopy. Tumor markers were evaluated for differential diagnosis between non-epithelial and epithelial tumors and for a definitive diagnosis of an epithelial tumor. The difference in CA-125 level before treatment and postoperative 1 month was calculated as follows: CA-125 decline (%)=(pretreatment value-postoperative 1 month value)/pretreatment value×100. We defined the optimal cut-off value for survival as that which gave the greater degree of sensitivity and specificity to dichotomize patients in univariate analysis, even though there were several cut-off values that impacted survival.
All patients underwent staging laparotomy which included cytologic examination of ascites or peritoneal washings, intact tumor removal, thorough inspection of the abdomen and pelvis, total abdominal hysterectomy, bilateral salpingo-oophorectomy, partial or total omentectomy, pelvic node dissection, para-aortic lymph node sampling, and targeted biopsies of suspected peritoneal metastases. All surgical specimens were examined using the same pathologic protocol. Surgical information included the maximum size of largest residual tumor at the surgery. The histological classification and grade of ovarian malignancy were based on the World Health Organization classifications. The FIGO classification system was used to determine pathological staging of the tumors.
For all patients, chemotherapy was started within approximately 2 weeks after surgery. The regimen was a combination of one taxane and one platinum derivative. Taxane derivatives included paclitaxel (175 mg/m2) and docetaxel (75 mg/m2), and the platinum derivative was either cisplatin (70 mg/m2) or carboplatin (target area under the curve [AUC] of 5). After completion of chemotherapy, patients underwent physical examination, CA-125, and CT or PET/CT scan of the abdomen and pelvis for clinical restaging. Only patients with no clinical, radiographic, or biochemical (CA-125<35 U/mL) evidence of disease were recommended to periodical routine check-up; those with residual or progressive disease after chemotherapy underwent second line chemotherapy at the discretion of their physician.
We classified patterns of treatment failure into APF and distant metastasis. APF included intraperitoneal, retroperitoneal space and the pelvic cavity. Distant metastasis was defined as recurrence in solid organs such as bones, lungs, liver, or brain. APF-free survival (APFFS) and overall actuarial survival (OS) rates were calculated using the Kaplan-Meier method, and differences were compared using the log-rank test. Univariate analysis was used to define the prognostic factors influencing APF and OS. The relative importance of the covariates in determining prognostic factors was also assessed by a multivariate Cox proportional hazards model. A p-value ≤0.05 was considered significant.
After completion of chemotherapy, patients were followed at the Women's Cancer Clinic at Hospital every three months during the first two years, every six months during the next three years, and then every year afterwards. Patients were examined at each visit, utilizing a complete history taking/physical examination. The follow-up evaluations included CA-125, CT scans of the chest and abdomen, and [18F]fludeoxyglucose (FDG) PET/CT. Generally, CA-125 and abdomen CT were performed every 6 months during first 3 years and annually during the next 2 years. FDG PET/CT was performed after last cycle of first-line chemotherapy, and then annually. Recurrence was treated by salvage chemotherapy, surgery, or radiotherapy.
Patient characteristics and clinical profiles are listed in Table 1. The ages of the patients ranged from 18 to 77 years (median, 51 years). Serous adenocarcinoma accounted for four fifths of all tumors, and 73 tumors (49.0%) were poorly differentiated. Thirty two patients (21.5%) had larger than 2 cm sized gross residual disease after cytoreductive surgery, and malignant cells were found in peritoneal washing cytology in 95 patients (63.8%). One hundred and forty patients (94.0%) received systematic lymphadenectomy. The median number of dissected nodes was 24 (range, 2 to 70). The incidence of pathologic node positivity was 60.4% (n=90), and the median number of resected metastatic nodes was 3 (range, 1 to 45), which were found in the pelvis (n=48, 32.2%), para-aortic lymph nodes (n=14, 9.4%), or both (n=28, 18.8%). The median pretreatment CA-125 level was 604 (range, 12.5 to 12,000). CA-125 level declined by more than 90% in 81 patients after surgery.
Chemotherapeutic regimens were comprised as follows: paclitaxel and carboplatin in 94 patients (63.1%), paclitaxel and cisplatin in 22 patients (14.8%), docetaxel and carboplatin in 20 patients (13.4%), docetaxel+cisplatin in 8 patients (5.4%), and paclitaxel+carboplatin/cisplatin in 5 patients (3.4%). Most patients received at least six cycles. However, 15 patients did not finish six cycles of adjuvant chemotherapy due to chemotherapy-related toxicity.
During the median follow-up duration of 50 months (range, 0 to 136.5 months), 83 patients (55.7%) experienced treatment failure. Of these 83 patients, 70 patients (47.0%) had APF only, 9 patients (6.0%) had APF with distant metastasis, and 4 patients (2.7%) had distant metastasis only as the first site of failure. Survival analysis showed that the 5-year APFFS and OS were 41.1% and 56.7%, respectively. The sites of distant metastasis were the liver (n=6, 4.0%), supraclavicular-mediastinal lymph node (n=4, 2.7%), lung (n=3, 2.0%), and brain (n=2, 1.3%).
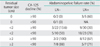
According to univariate analysis, the significant prognostic indicators for APFFS were age, grade, peritoneal washing cytology, peritoneal metastasis, lymph node involvement, residual disease, and percentage of CA-125 decline (Table 2). They were also significantly prognostic for OS. Cox regression analysis identified lymph node involvement, residual disease and percentage of CA-125 decline as independent prognostic factors for APFFS. For OS, age, grade, peritoneal washing cytology, and percentage of CA-125 decline retained significance in multivariate analysis (Table 3).
We divided the patients into subgroups according to three risk factors which were identified from multivariate analysis for APFFS, such as residual tumor size, decline in CA-125, and lymph node involvement (Table 4). The steps of the classification process were as follows: In patients with no residual tumor size, even though it was difficult to compare because of the small numbers, lymph node (LN) negative patients did not fail regardless of decline in CA-125. However, LN positive patients demonstrated a 60% APF rate. In patients with a residual tumor size of less than 2 cm and a decline in CA-125 over 90%, although 3 out of 22 LN negative patients (13.6%) failed regardless of decline in CA-125, LN positive patients demonstrated an APF rate of 30% (9/30). In patients with a residual tumor size of less than 2 cm and a decline in CA-125 of less than 90%, APF rates were much higher compared with the over 90% decline patients. In patients with residual tumor size larger than 2 cm, at least two thirds of the patients of all subgroups failed in the abdominopelvic spaces. Subgroups with a similar risk were gathered and their overall APF rate was calculated (Fig. 1). The intermediate and high risk groups comprised 55% and 43% of the overall patient population and their APF rates were 30% and 77%, respectively. The 5-year APFFS and OS according to risk subgroups are shown in Fig. 2.
Our data demonstrated that APF was the predominant pattern of treatment failure in EOC patients treated with definitive and adjuvant therapy, and failure sites were almost evenly distributed within the abdominopelvic cavity. While distant metastasis alone was observed in only four patients, more than a half of EOC patients experienced APF as the first failure within the first two years. Because APF eventually progresses to a fatal outcome in most patients, it is important to decide which consolidation therapy should be used to prevent APF.
To decrease the incidence of APF, intraperitoneal chemotherapy and WART have been used and tested in clinical settings. Two recent meta-analyses provided supportive data for intraperitoneal chemotherapy with intravenous chemotherapy [6,7]. WART has also been considered to be one of the possible adjuvant therapies in EOC patients. The randomized trial by Sobre et al. [8] indicated that patients treated with consolidation WART had a significant better disease-free and overall survival in the subgroup with complete surgical and pathologic remission compared with patients treated with consolidation chemotherapy. Additionally, WART has some theoretical and practical advantages over other intraperitoneal approaches as follows: a more homogeneous dose distribution, better coverage of retroperitoneal lymph nodes, and the ability to treat all peritoneal surfaces without limitations from the presence of postoperative adhesions [9].
However, many oncologists have been hesitant to use WART for several reasons. First, only a few trials have demonstrated any positive clinical benefits of WART for the management of EOC, although WART as an adjuvant treatment has been compared with chemotherapy in a small number of trials [5]. The combination of taxane and platinum, the current standard combination chemotherapy regimen, has shown superior therapeutic efficacy compared with previous chemotherapy regimens, and is generally acknowledged as the only adjuvant therapy. Second, the open-field technique has been conventionally preferred to WART in gynecologic cancer patients. Acute and late treatment-related complications were found to be significant problems in some trials. At present, novel radiation oncological approaches consider the statification of patients with high risk clinicopathologic factors of APF, and more such approaches are being developed to deliver WART more safely and effectively.
Even though the implication of clinicopathologic factors may be different from one another, tumor stage, size of residual disease, histologic type and grade, surgical factors including tumor spillage, cytologically malignant ascites, and CA-125 have been generally accepted as significant prognostic factors for EOC [10]. Until now, the prognostic classification of the Princess Margaret Hospital has been most frequently used to define the application of WART. Their multivariate analysis of prognostic factors showed stage, residuum and tumor grade and histological subtype were significantly independent predictors of relapse and survival. Based upon three variables, outcome was evaluated using a matrix to allow for the division of patients into two subgroups according to risk of relapse after WART [11]. The intermediate-risk subgroup comprised one third of all patients and showed a 5-year survival rate over 70% when treated with WART that was significantly better compared with other treatment modalities. The high risk subgroup, 15% of total patient population, showed recurrence of 80% and survival rate of 30% at 5-year. The classification proved to be valid by subsequent studies [12,13] and has been adopted through several modifications in most studies [14]. However, this risk estimation might be different for current standard treatments, because the classification was founded on data from patients who had not undergone chemotherapy or been treated with platinum-based chemotherapy. Finally, new changes in treatment modalities should be considered for prognostic classifications, such as estimation of tumor bulkiness and response monitoring using CA-125, as well as the combination of taxane and platinum.
In our study, patients were classified on the basis of this tumor burden category using three significant risk factors for APFFS as these seem to be primary consideration for consolidation WART. Because the low risk group had no APF in this study, no further consolidation treatment would be needed after primary surgery and adjuvant chemotherapy for these patients. High risk patients might be thought to not only have too large tumors of to be completely removed by surgery, but also to have aggressive biologic features which may lead to recurrence in a short period despite the use of current adjuvant therapy. For these patients, new approaches should be considered in view of biological aspects. Patients with intermediate risk may be considered to receive adjuvant WART. In our data, these population included patients with no residual size and positive LN regardless of status of decline of CA-125, patients with residual tumor less than 2 cm and negative LN irrespective of status of decline of CA-125 and patients with residual tumor less than 2 cm, positive LN and decline of CA-125 over than 90%. If disease-free status can be consolidated by WART as an adjuvant locoregional therapy, it can improve clinical outcomes and the quality of life of EOC patients.
In addition to accurate identification of intermediate risk group based upon operative and pathologic findings, careful response evaluation after adjuvant chemotherapy is important to decide further treatment policy. In the past, second-look operation (SLO) was mainly performed to detect residual disease after primary treatment for EOC. However, even if stage III patients had negative in SLO, the recurrence substantially developed up to 30% at 2 year and 50% at 5 year [15]. Moreover, Gynecologic Oncologic Group analysis showed SLO was not associated with longer survival of optimally resected stage III ovarian cancer in nonrandomized comparison [16]. Remarkable improvement of imaging technology has gradually replaced SLO. PET/CT before SLO showed high sensitivity from 78% to 93% when correlated with histologic findings after SLO [17,18]. Additionally, the combination of CA-125 and PET/CT has improved the identification of patients with recurrent disease [19]. Therefore, PET/CT is considered to be more suitable modality than SLO after adjuvant chemotherapy because of avoiding small bowel complication from additional operation.
One of the most challenging toxicities, in addition to small bowel toxicity, is to spare the hematopoietic function of bone marrow, because salvage chemotherapy plays a critical role in reducing tumor size and prolonging survival in recurrent EOC. Several investigators reported that helical tomotherapy is feasible and fast for WART with excellent coverage of the planning target size and effective sparing of bone marrow organs at risk [20,21]. Recently, the Heidelberg group performed a phase I clinical trial to assess the feasibility and toxicity of consolidative intensity-modulated WART (30 Gy/15 fractions) after surgery and chemotherapy in high-risk patients with advanced ovarian cancer. The treatment was well tolerated and late complications were manageable [22]. IMRT and helical tomotherapy make it technically possible to deliver high-dose radiation to a risky area for better tumor control without raising WART dose using a simultaneous integrated boost technique. However, the caution is needed in the use of those techniques because of uncertainties in radiation dose delivery induced by intrafraction abdominal organ motion. To minimize those uncertainties, a planning four-dimensional CT scan with/without patient immobilization is recommended.
In conclusions, our data showed that APF is the dominant pattern of failures in EOC patients. Size of residual disease, LN involvement and decline in CA-125 were significantly prognostic factors of APF after primary treatment. Even though more analyses are needed to validate this stratification, WART using the IMRT technique may be considered to reduce APF in FIGO stage III EOC patients with intermediate risk. Further analyses are needed to define the subgroup for which WART can be applied as a consolidation for EOC patients.
Figures and Tables
Fig. 1
The definition of patient subgroups according to residual tumor size, decline in CA-125 and lymph node (LN) involvement.
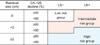
Fig. 2
The 5-year abdominopelvic failure-free (A) and overall actuarial survival (B) rates according to risk group.

ACKNOWLEDGMENTS
This study was supported by a faculty research grant of Yonsei University College of Medicine for 2008(6-2008-0106).
References
1. McGuire WP, Hoskins WJ, Brady MF, Kucera PR, Partridge EE, Look KY, et al. Cyclophosphamide and cisplatin compared with paclitaxel and cisplatin in patients with stage III and stage IV ovarian cancer. N Engl J Med. 1996. 334:1–6.
2. Muggia FM, Braly PS, Brady MF, Sutton G, Niemann TH, Lentz SL, et al. Phase III randomized study of cisplatin versus paclitaxel versus cisplatin and paclitaxel in patients with suboptimal stage III or IV ovarian cancer: a gynecologic oncology group study. J Clin Oncol. 2000. 18:106–115.
3. Piccart MJ, Bertelsen K, James K, Cassidy J, Mangioni C, Simonsen E, et al. Randomized intergroup trial of cisplatin-paclitaxel versus cisplatin-cyclophosphamide in women with advanced epithelial ovarian cancer: three-year results. J Natl Cancer Inst. 2000. 92:699–708.
4. Pectasides D, Pectasides E. Maintenance or consolidation therapy in advanced ovarian cancer. Oncology. 2006. 70:315–324.
5. Dembo AJ. Radiotherapeutic management of ovarian cancer. Semin Oncol. 1984. 11:238–250.
6. Jaaback K, Johnson N. Intraperitoneal chemotherapy for the initial management of primary epithelial ovarian cancer. Cochrane Database Syst Rev. 2006. (1):CD005340.
7. Hess LM, Benham-Hutchins M, Herzog TJ, Hsu CH, Malone DC, Skrepnek GH, et al. A meta-analysis of the efficacy of intraperitoneal cisplatin for the front-line treatment of ovarian cancer. Int J Gynecol Cancer. 2007. 17:561–570.
8. Sorbe B. Swedish-Norwegian Ovarian Cancer Study Group. Consolidation treatment of advanced (FIGO stage III) ovarian carcinoma in complete surgical remission after induction chemotherapy: a randomized, controlled, clinical trial comparing whole abdominal radiotherapy, chemotherapy, and no further treatment. Int J Gynecol Cancer. 2003. 13:278–286.
9. Cardenes H, Randall ME. Integrating radiation therapy in the curative management of ovarian cancer: current issues and future directions. Semin Radiat Oncol. 2000. 10:61–70.
10. Barakat RR, Markman M, Randall ME. Principles and practice of gynecologic oncology. 2009. 5th ed. Philadelphia: Lippincott Williams & Wilkins.
11. Dembo AJ. Abdominopelvic radiotherapy in ovarian cancer: a 10-year experience. Cancer. 1985. 55:9 Suppl. 2285–2290.
12. Goldberg N, Peschel RE. Postoperative abdominopelvic radiation therapy for ovarian cancer. Int J Radiat Oncol Biol Phys. 1988. 14:425–429.
13. Carey MS, Dembo AJ, Simm JE, Fyles AW, Treger T, Bush RS. Testing the validity of a prognostic classification in patients with surgically optimal ovarian carcinoma: a 15-year review. Int J Gynecol Cancer. 1993. 3:24–35.
14. Dinniwell R, Lock M, Pintilie M, Fyles A, Laframboise S, Depetrillo D, et al. Consolidative abdominopelvic radiotherapy after surgery and carboplatin/paclitaxel chemotherapy for epithelial ovarian cancer. Int J Radiat Oncol Biol Phys. 2005. 62:104–110.
15. Rubin SC, Randall TC, Armstrong KA, Chi DS, Hoskins WJ. Ten-year follow-up of ovarian cancer patients after second-look laparotomy with negative findings. Obstet Gynecol. 1999. 93:21–24.
16. Greer BE, Bundy BN, Ozols RF, Fowler JM, Clarke-Pearson D, Burger RA, et al. Implications of second-look laparotomy in the context of optimally resected stage III ovarian cancer: a non-randomized comparison using an explanatory analysis: a Gynecologic Oncology Group study. Gynecol Oncol. 2005. 99:71–79.
17. Chung HH, Kang WJ, Kim JW, Park NH, Song YS, Chung JK, et al. Role of [18F]FDG PET/CT in the assessment of suspected recurrent ovarian cancer: correlation with clinical or histological findings. Eur J Nucl Med Mol Imaging. 2007. 34:480–486.
18. Sironi S, Messa C, Mangili G, Zangheri B, Aletti G, Garavaglia E, et al. Integrated FDG PET/CT in patients with persistent ovarian cancer: correlation with histologic findings. Radiology. 2004. 233:433–440.
19. Pan HS, Lee SL, Huang LW, Chen YK. Combined positron emission tomography-computed tomography and tumor markers for detecting recurrent ovarian cancer. Arch Gynecol Obstet. 2011. 283:335–341.
20. Rochet N, Sterzing F, Jensen A, Dinkel J, Herfarth K, Schubert K, et al. Helical tomotherapy as a new treatment technique for whole abdominal irradiation. Strahlenther Onkol. 2008. 184:145–149.
21. Kim YB, Kim JH, Jeong KK, Seong J, Suh CO, Kim GE. Dosimetric comparisons of three-dimensional conformal radiotherapy, intensity-modulated radiotherapy, and helical tomotherapy in whole abdominopelvic radiotherapy for gynecologic malignancy. Technol Cancer Res Treat. 2009. 8:369–377.
22. Rochet N, Sterzing F, Jensen AD, Dinkel J, Herfarth KK, Schubert K, et al. Intensity-modulated whole abdominal radiotherapy after surgery and carboplatin/taxane chemotherapy for advanced ovarian cancer: phase I study. Int J Radiat Oncol Biol Phys. 2010. 76:1382–1389.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download