Abstract
Objective
In the present study, we evaluated changes in CA-125 cut-off values predictive of complete interval debulking surgery (IDS) after neoadjuvant chemotherapy (NAC) using receiver operating characteristic (ROC) analysis.
Methods
This retrospective single-institution study included patients with International Federation of Gynecology and Obstetrics (FIGO) stage III epithelial ovarian cancer and a pre-NAC serum CA-125 level of greater than 40 U/mL who were treated with neoadjuvant platinum-based chemotherapy followed by IDS between 1994 and 2009. Logistic regression analysis was used to evaluate univariate and independent multivariate associations with the effect of clinical, pathological, and CA-125 parameters on complete IDS, and ROC analysis was used to determine potential cut-off values of CA-125 for prediction of the possibility of complete IDS.
Results
Seventy-five patients were identified. Complete IDS was achieved in 46 (61.3%) patients and non-complete IDS was observed 29 (38.7%). Median pre-NAC CA-125 level was 639 U/mL (range, 57 to 6,539 U/mL) in the complete IDS group and 1,427 U/mL (range, 45 to 10,989 U/mL) in the non-complete IDS group. Median pre-IDS CA-125 level was 15 U/mL (range, 2 to 60 U/mL) in the complete IDS group and 53 U/mL (range, 5 to 980 U/mL) in the non-complete IDS group (p<0.001). Multivariate analyses performed with complete IDS as the endpoint revealed only pre-IDS CA-125 as an independent predictor. The odds ratio of non-complete IDS was 10.861 when the pre-IDS CA-125 level was greater than 20 U/mL.
Ovarian cancer is increasing annually in Japan [1] and the total number of ovarian cancer cases in 2006 was 7,913 [2]. Standard therapy for ovarian cancer consists of primary surgical cytoreduction followed by platinum-based chemotherapy, but 25% to 90% of cases of ovarian cancer are diagnosed in progress [3]. Primary optimal cytoreduction performed for patients with advanced stage ovarian cancer can be complicated, requiring extensive bowel resection and blood loss, with a high risk of morbidity. Another obstacle to optimal cytoreduction is the individual patient's medical condition. Neoadjuvant chemotherapy (NAC) is therefore often performed for patients with advanced ovarian cancer, with interval debulking surgery (IDS) performed after NAC when possible. Paclitaxel and carboplatin as 1st line chemotherapy are administered to patients with ovarian cancer, and overall response rates of 59% [4] and 68% [5] have been reported in studies in which paclitaxel (175-185 mg/m2) and carboplatin (area under the curve; 5-6) were administered every 3 weeks. Many authors reported rates of optimal IDS after NAC ranging from 77% to 94% [6,7]. Imaging devices can be used to determine whether a tumor can be completely removed after NAC. Computed tomography (CT) is a standard device of evaluating tumor spread, although the sensitivity for peritoneal metastases of 1 cm or smaller in maximum diameter is only 25% to 50% and significantly lower than the overall sensitivity of 85% to 93% using spiral CT [8]. Even when using multidetector CT, sensitivity is only 64% [3]. In some cases, therefore, complete cytoreduction may not be achieved with IDS, even when complete resection is predicted by imaging devices such as CT. In addition to imaging devices, however, CA-125 levels may help to predict complete resection after NAC [9]. One report concluded that patients with preoperative CA-125 levels of less than 100 U/mL were highly likely to be cytoreduced with no residual disease [9]. In our experience, however, peritoneal dissemination is often observed and thus complete cytoreduction cannot be achieved when IDS is performed in patients with CA-125 levels of less than 100 U/mL after NAC. Therefore, in the present study, we evaluated the changes in CA-125 levels in patients with advanced ovarian cancer and determined the CA-125 cut-off values predictive of complete cytoreduction after NAC using receiver operating characteristic (ROC) analysis.
Eligible patients had biopsy-proven with International Federation of Gynecology and Obstetrics (FIGO) stage III epithelial ovarian cancer with pre-NAC CA-125 levels of greater than 40 U/mL, and were treated in our institution with neoadjuvant platinum-based chemotherapy followed by IDS between 1994 and 2009. Patients who had an initial laparotomy with minimal or no debulking (e.g., omentectomy only or biopsy only) were included. Subsequently, patients underwent three cycles of platinum-based NAC and then IDS. Complete IDS was defined as no residual tumor and no peritoneal dissemination at completion of the surgical procedure. Non-complete IDS was defined as visible residual tumor, including peritoneal dissemination, at completion of the surgical procedure. After IDS, all patients received 3 to 6 cycles of adjuvant chemotherapy.
Serum CA-125 levels were measured by a commercially available radioimmunoassay and CA-125 levels from pre-NAC to pre-IDS were recorded. Rates of changes in CA-125 levels were calculated as follows: (pre-NAC CA-125 - pre-2nd NAC CA-125) / pre-NAC CA-125, (pre-NAC CA-125 - pre-3rd NAC CA-125) / pre-NAC CA-125. Pre-NAC CA-125 represents CA-125 level before administering 1st NAC, pre-2nd NAC CA-125 represents CA-125 level before administering 2nd NAC, and pre-3rd NAC CA-125 represents CA-125 level before administering 3rd NAC.
All statistical analyses were conducted using SPSS ver. 17 (SPSS Inc., Chicago, IL, USA). Probability values of less than 0.05 were considered to indicate statistical significance. The Mann-Whitney and chi-square tests were used to test for correlations between patients'characteristics and complete or non-complete IDS. Logistic regression analysis was used to evaluate univariate and independent multivariate associations with the effect of clinical or pathological parameters and rates of changes in CA-125 levels on complete IDS. ROC analysis was used to determine potential cut-off values of CA-125 levels for prediction of the possibility of complete IDS. Overall survival was estimated by the Kaplan-Meier method and compared using the log-rank test.
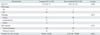
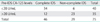
We identified 75 patients that fulfilled the above criteria. Median follow-up was 40 months (range, 5 to 121 months). Complete IDS was achieved in 46 of 75 (61.3%) patients and non-complete IDS was observed in 29 of 75 (38.7%). Patient characteristics are presented in Table 1.
IDS was complete in 43 (93.5%) and non-complete in 27 (93.1%) FIGO stage IIIC patients. In the complete IDS group, 31 (67.4%) patients had serous adenocarcinoma and 9 (19.6%) had endometrioid adenocarcinoma. In the non-complete group, 20 (70.0%) had serous adenocarcinoma and 5 (17.2%) had endometrioid adenocarcinoma. In the complete IDS group, 28 (60.9%) received taxane and platinum-based NAC and 18 (39.1%) received platinum-based NAC. In the non-complete group, 18 (62.1%) received taxane and platinum-based NAC and 11 (37.9%) received platinum-based NAC. Median pre-NAC CA-125 level was 639 U/mL (range, 57 to 6,539 U/mL) in the complete IDS group and 1,427 U/mL (range, 45 to 10,989 U/mL) in the non-complete IDS group, with no significant difference between groups.
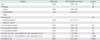
Median pre-IDS CA-125 level was 15 U/mL (range, 2 to 60 U/mL) in the complete IDS group and lower than that of 53 U/mL (range, 5 to 980 U/mL) in the non-complete IDS group (p<0.001). In the univariate logistic analysis, factors significantly associated with the possibility of complete IDS were (pre-NAC CA-125 - pre-2nd NAC CA-125) / pre-NAC CA-125, (pre-NAC CA-125 - pre-3rd NAC CA-125) / pre-NAC CA-125, and pre-IDS CA-125 (Table 2). Multivariate analysis performed with complete IDS as an endpoint revealed that the only independent predictor was pre-IDS CA-125 level (p<0.001) (Table 3).
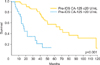
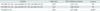
Subsequently, ROC analysis demonstrated that pre-IDS CA-125 level indicated good discrimination capability between the complete and non-complete IDS group. Based on ROC analysis, the cut-off value of the pre-IDS CA-125 level to predict the possibility of complete IDS was 20 U/mL. The sensitivity and specificity of pre-IDS CA-125 were 0.744 and 0.821, respectively. Table 4 shows relation between pre-IDS CA-125 levels of greater than 20 U/mL with non-complete IDS and the odds ratio was 10.861 with a 95% confidence interval of 2.972 to 34.498. Overall survival was a significantly different between those with pre-IDS CA-125 levels of less than 20 U/mL and those with pre-IDS CA-125 of greater than 20 U/mL (p<0.001). Median overall survival was 71 months in the group with pre-IDS CA-125 levels of less than 20 U/mL and 18 months in the group with pre-IDS CA-125 levels greater than 20 U/mL (Fig. 1).
Ovarian cancer is usually diagnosed in an advanced stage. In the advanced stage, many patients have multiple tumor deposits throughout the peritoneum (peritonitis carcinomatosa), making it difficult to completely debulk tumors in these patients. Therefore, NAC is often administered to decrease the tumor size before attempting IDS. Based on a previous report in which optimal cytoreduction was defined as a residual tumor of less than 1 cm and only patients receiving primary cytoreduction were included, preoperative CA-125 level of 500 U/mL was determined to be critical for discriminating patients who might achieve optimal cytoreduction [10]. Another report discussed similar results [11]. In contrast, another report of patients receiving primary cytoreduction [12] concluded that preoperative CA-125 level was not a predictor of optimal cytoreduction. In patients receiving NAC, a pre-IDS CA-125 level of less than 100 U/mL could be predictive of complete cytoreduction [9]. We have often found peritoneal dissemination when operating on patients with CA-125 levels of less than 100 U/mL after NAC. The findings of the present study suggest that pre-IDS CA-125 levels of less than 20 U/mL could be a predictor of complete IDS. Many studies have reported a relation between CA-125 level and cytoreduction. The reason for this may be that patients with stage III have variable disease spread from a solitary lesion to diffuse mesenteric or peritoneal dissemination. A solitary lesion, even if it is large, can be resected completely. In contrast, complete resection of peritoneal dissemination can be difficult. Furthermore, operations are performed by surgeons with various levels of experience and different techniques, so the rates of optimal surgery also vary among surgeons [13]. The present study was a single institution study and operations were performed by only two surgeons, so the potential for a surgeon bias is small. The relation between the pattern of the CA-125 response and overall survival in patients with ovarian cancer undergoing three cycles of NAC followed by IDS and three more cycles of chemotherapy has been reported [14]; CA-125 normalization, defined as a value of 35 U/mL after NAC, was not an independent predictor of either progression-free or overall survival, but CA-125 at the end of chemotherapy was an independent predictor of overall survival. Therefore, less residual tumor at the end of first treatment contributes overall survival for advanced ovarian cancer. CA-125 level can predict chemotherapeutic sensitivity and a tumor volume decrease by IDS, leading to a prolonged prognosis. Based on the findings of the present study, the frequency of complete IDS might be increased by performing more aggressive surgery, such as liver resection and pelvic exenteration, in patients with pre IDS CA-125 levels greater than 20 U/mL. Aggressive surgery, however, may cause intraoperative and postoperative morbidity. The risk of morbidity, such as the need for unplanned readmission, any complication requiring reoperation, deep venous thrombosis, sepsis, major cardiac events, or pneumonia, varies progressively during the first 30 postoperative days, depending on complexity of surgery [15]. Patient treatment should be based on consideration of both the quality of life and the quality of treatment. Limitations of the present study include the relatively small sample size and the fact that it is a retrospective study.
In conclusion, the findings of the present study suggest that in the setting of IDS after three cycles of platinum-based NAC for advanced ovarian cancer, a pre-IDS CA-125 level of less than 20 U/mL was an independent predictor of complete IDS outcome. By monitoring the CA-125 level after three cycles of NAC, the risk of morbidity can be reduced in patients with advanced ovarian cancer when IDS is performed.
Figures and Tables
Fig. 1
Kaplan-Meier estimates of overall survival in 2 groups. The median overall survival was 71 months in the pre-interval debulking surgery (IDS) CA-125 less than 20 U/mL group and 18 months in the pre-IDS CA-125 greater than 20 U/mL group.
References
1. Ushijima K. Current status of gynecologic cancer in Japan. J Gynecol Oncol. 2009. 20:67–71.
2. Matsuda T, Marugame T, Kamo K, Katanoda K, Ajiki W, Sobue T, et al. Cancer incidence and incidence rates in Japan in 2006: based on data from 15 population-based cancer registries in the monitoring of cancer incidence in Japan (MCIJ) project. Jpn J Clin Oncol. 2012. 42:139–147.
3. Metser U, Jones C, Jacks LM, Bernardini MQ, Ferguson S. Identification and quantification of peritoneal metastases in patients with ovarian cancer with multidetector computed tomography: correlation with surgery and surgical outcome. Int J Gynecol Cancer. 2011. 21:1391–1398.
4. Vasey PA, Jayson GC, Gordon A, Gabra H, Coleman R, Atkinson R, et al. Phase III randomized trial of docetaxel-carboplatin versus paclitaxel-carboplatin as first-line chemotherapy for ovarian carcinoma. J Natl Cancer Inst. 2004. 96:1682–1691.
5. du Bois A, Luck HJ, Meier W, Adams HP, Mobus V, Costa S, et al. A randomized clinical trial of cisplatin/paclitaxel versus carboplatin/paclitaxel as first-line treatment of ovarian cancer. J Natl Cancer Inst. 2003. 95:1320–1329.
6. Giannopoulos T, Butler-Manuel S, Taylor A, Ngeh N, Thomas H. Clinical outcomes of neoadjuvant chemotherapy and primary debulking surgery in advanced ovarian carcinoma. Eur J Gynaecol Oncol. 2006. 27:25–28.
7. Chan YM, Ng TY, Ngan HY, Wong LC. Quality of life in women treated with neoadjuvant chemotherapy for advanced ovarian cancer: a prospective longitudinal study. Gynecol Oncol. 2003. 88:9–16.
8. Coakley FV, Choi PH, Gougoutas CA, Pothuri B, Venkatraman E, Chi D, et al. Peritoneal metastases: detection with spiral CT in patients with ovarian cancer. Radiology. 2002. 223:495–499.
9. Rodriguez N, Rauh-Hain JA, Shoni M, Berkowitz RS, Muto MG, Feltmate C, et al. Changes in serum CA-125 can predict optimal cytoreduction to no gross residual disease in patients with advanced stage ovarian cancer treated with neoadjuvant chemotherapy. Gynecol Oncol. 2012. 125:362–366.
10. Vorgias G, Iavazzo C, Savvopoulos P, Myriokefalitaki E, Katsoulis M, Kalinoglou N, et al. Can the preoperative Ca-125 level predict optimal cytoreduction in patients with advanced ovarian carcinoma? A single institution cohort study. Gynecol Oncol. 2009. 112:11–15.
11. Eltabbakh GH, Mount SL, Beatty B, Simmons-Arnold L, Cooper K, Morgan A. Factors associated with cytoreducibility among women with ovarian carcinoma. Gynecol Oncol. 2004. 95:377–383.
12. Memarzadeh S, Lee SB, Berek JS, Farias-Eisner R. CA125 levels are a weak predictor of optimal cytoreductive surgery in patients with advanced epithelial ovarian cancer. Int J Gynecol Cancer. 2003. 13:120–124.
13. Ibeanu OA, Bristow RE. Predicting the outcome of cytoreductive surgery for advanced ovarian cancer: a review. Int J Gynecol Cancer. 2010. 20:Suppl 1. S1–S11.
14. Le T, Faught W, Hopkins L, Fung-Kee-Fung M. Importance of CA125 normalization during neoadjuvant chemotherapy followed by planned delayed surgical debulking in patients with epithelial ovarian cancer. J Obstet Gynaecol Can. 2008. 30:665–670.
15. Aletti GD, Dowdy SC, Podratz KC, Cliby WA. Relationship among surgical complexity, short-term morbidity, and overall survival in primary surgery for advanced ovarian cancer. Am J Obstet Gynecol. 2007. 197:676.e1–676.e7.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download