Abstract
Objective
To evaluate the clinical outcome and parameters related to coexisting endometrial carcinoma in women with tissue-diagnosed endometrial hyperplasia.
Methods
Between January 1991 and December 2009, three hundred and eighty-six patients with the presumptive diagnosis of endometrial hyperplasia were retrieved. Among these, one hundred and twenty-five patients were identified as having coexisting endometrial carcinoma in hysterectomy specimens. The three hundred and eighty-six patients were divided into two groups: the hyperplasia-benign group (261 cases) and the hyperplasia-malignant group (125 cases). Several clinical parameters including age, menopausal status, history of abnormal uterine bleeding, obstetrical history, medical history of diabetes and hypertension, BMI, and preoperative pathologic results were investigated.
Results
Age ≥53 (odds ratio [OR], 2.40; 95% confidence interval [CI], 1.26 to 4.57), menopausal status (OR, 2.07; 95% CI, 1.14 to 3.76), diabetes history (OR, 7.33; 95% CI, 2.79 to 19.26), abnormal uterine bleeding (OR, 3.99; 95% CI, 1.22 to 13.02), atypical endometrial hyperplasia (OR, 7.38; 95% CI, 4.03 to 13.49), and body mass index ≥27 (OR, 3.24; 95% CI, 1.76 to 5.97) were independent risk factors for prediction of endometrial hyperplasia coexisting with endometrial carcinoma. The diagnostic efficacy of atypical endometrial hyperplasia to predict the endometrial hyperplasia coexisting with endometrial carcinoma was better than or similar to those of other independent factors and combinations of these factors.
The endometrioid neoplastic lesions of the endometrium have been proposed to be the end point of a continuum of morphologically hyperplastic lesions [1]. According to the World Health Organization classification system in 1994 (WHO94), endometrial hyperplasia can be divided into four categories: simple hyperplasia, complex hyperplasia, simple hyperplasia with atypia, and complex hyperplasia with atypia [2]. Endometrial hyperplasia is defined as a proliferation of glands of irregular size and shape with an increase in the glands/stroma ratio [3]. It is typically diagnosed by endometrial biopsy or curettage when a woman is noted as suffering from abnormal uterine bleeding.
Atypical endometrial hyperplasia (AEH) has been strongly associated with endometrial carcinoma [2]. Therefore, hysterectomy would be recommended for postmenopausal women with cytologic atypia because of the high risk of coexisting endometrial carcinoma and progression to cancer [3]. In Taiwan, operation would be suggested to the women with cytologic atypia, including postmenopausal women and those without fertility intention. High-dose progestin therapy (megestrol acetate, 160 to 320 mg/day) would be given to those cytologic atypia cases with fertility desire. Therapy would be continued for 2 to 3 months, and endometrial evaluation would be performed 3 to 4 weeks after completion of treatment. Periodic endometrial biopsy or transvaginal ultrasonography would be arranged after progestin therapy for atypical hyperplasia. Hysterectomy would also be recommended for these patients after completion of fertility concern.
However, the WHO94 criteria are largely subjective and have been criticized for low reproducibility [4]. One pathologic review by the Gynecology Oncology Group (GOG) also failed to demonstrate the consistency of differentiation between AEH and carcinoma [1]. Even though the Endometrial Collaborative Group has suggested a new concept, endometrial intraepithelial neoplasia (EIN), for superior reproducibility, the system has not undergone evaluation with regards to reproducibility and prospective assessment [4,5]. Therefore, more investigations should be explored for coexisting endometrial carcinoma in patients with endometrial hyperplasia.
The reported rate of coexisting endometrial carcinoma with the initial attempt to treat AEH is increasing [1,6]. Other clinical parameters for endometrial hyperplasia patients coexisting with endometrial carcinoma were not well analyzed. Our previous investigation has shown that cytologic atypia and high body mass index (BMI) are both independent factors for coexisting endometrial carcinoma in endometrial hyperplasia women [7]. Therefore, we submitted this current study to the Taiwanese Gynecologic Oncology Group (TGOG) for a retrospective multi-center investigation to evaluate the clinical outcome and parameters related to coexisting endometrial carcinoma in women with tissue-diagnosed endometrial hyperplasia. Then, a more suitable management modality could then be proposed for these endometrial hyperplasia patients with coexisting endometrial carcinoma.
We retrospectively reviewed the cases undergoing indicated hysterectomies for gynecologic tumors between January 1991 and December 2009 in TGOG database. Among these women, three hundred and eighty-six patients with preoperative diagnosis of endometrial hyperplasia were identified before hysterectomies. Two hundred and eighty-three patients were diagnosed as endometrial hyperplasia by the dilation and curettage, 71 cases by the pipelle biopsy, and 32 women by hysteroscopic biopsy. One hundred and twenty-five of the 386 cases had been diagnosed as endometrial carcinoma, but the other 261 women did not have malignant components in their hysterectomy specimens. In all hospitals, the institutional review boards approved this multi-center retrospective study.
Depending on the final pathologic results of hysterectomy, we divided the 386 patients into two groups: the hyperplasia-benign, i.e. hyperplasia without malignancy (261 cases) and the hyperplasia-malignant, i.e. hyperplasia with malignancy (125 cases). Several clinical parameters including age, menopausal status, history of abnormal uterine bleeding, obstetrical history, medical history of diabetes and hypertension, BMI and preoperative pathologic results were reviewed and investigated for these studied population. The clinical and pathologic characteristics of the 125 patients diagnosed as having endometrial carcinoma postoperatively were also reviewed. The histological grading of endometrial carcinoma was based on International Federation of Gynecology and Obstetrics (FIGO) definitions proposed in 1988 [8].
For most of the patients with endometrial carcinoma, periodic examinations during follow-up included history taking, pelvic examinations, regional lymph nodes palpation and vault smear. Tumor markers, such as cancer antigen 125 (CA-125) and carcinoembryonic antigen (CEA), were also tested. Computed tomography or magnetic resonance imaging was performed for suspected disease recurrence. Abnormal findings of imaging studies, elevated tumor marker (≥2 folds of upper normal limits) of two consecutive tests in 2 week-interval, positive aspiration cytology, or tissue proven from biopsy was defined as recurrence.
Statistical analyses were performed using SAS ver. 9.2 (SAS Institute Inc., Cary, NC, USA). The demographic and clinical parameters including age, gravidity, parity, menopause status, hypertension history, diabetes history, bleeding history, preoperation pathology and BMI from 261 benign hyperplasia and 125 malignant hyperplasia patients were first screened by simple logistic regression analysis. Selected parameters were further analyzed by multiple logistic regression to obtain for prediction of coexisting endometrial carcinoma in endometrial hyperplasia. Finally, the diagnostic efficacies of each independent parameter and combinations of these factors were analyzed by receiver operating characteristic (ROC) curve. All tests were two-sided, and statistical significance was accepted for p<0.05.
In our survey, the mean age of this studied population was 48.98 years. These 386 patients were divided into two groups: the hyperplasia-benign group (261 cases) and the hyperplasia-malignant group (125 cases). The mean follow-up period of the hyperplasia-malignant group was 54.9 months. As shown in Table 1, when referenced with those cases in the hyperplasia-benign group, the women with age ≥53 (odds ratio [OR], 1.57; 95% confidence interval [CI], 1.38 to 3.86), menopausal status (OR, 2.40; 95% CI, 1.48 to 3.88), diabetes history (OR, 6.03; 95% CI, 2.68 to 13.54), abnormal uterine bleeding (OR, 4.24; 95% CI, 1.76 to 10.22), atypical endometrial hyperplasia (AEH; OR, 6.99; 95% CI, 4.21 to 11.59), and BMI ≥24, BMI 24-26.9 (OR, 1.79; 95% CI, 1.01 to 3.19), and BMI ≥27 (OR, 4.33; 95% CI, 2.59 to 7.24) in the hyperplasia-malignant group had statistically higher risks of being diagnosed as coexisting endometrial carcinoma by simple logistic regression model. In addition, our results showed that cases in the hyperplasiamalignant group with gravity ≥1 (OR, 0.61; 95% CI, 0.33 to 1.10) or parity ≥1 (OR, 0.70; 95% CI, 0.39 to 1.26) had reduced risks of coexisting endometrial carcinoma, which were not with statistical significance.
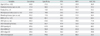
After adjusting the potential confounders by multiple logistic regression analysis in Table 2, age ≥53 (OR, 2.40; 95% CI, 1.26 to 4.57), menopausal status (OR, 2.07; 95% CI, 1.14 to 3.76), diabetes history (OR, 7.33; 95% CI, 2.79 to 19.26), abnormal uterine bleeding (OR, 3.99; 95% CI, 1.22 to 13.02), AEH (OR, 7.38; 95% CI, 4.03 to 13.49), and BMI ≥27 (OR, 3.24; 95% CI, 1.76 to 5.97) were demonstrated to be independent risk factors for prediction of endometrial hyperplasia coexisting with endometrial carcinoma in our study. Furthermore, parity ≥1 (OR, 0.43; 95% CI, 0.20 to 0.93) was an independent factors for negatively predicting coexisting endometrial carcinoma in patients with endometrial hyperplasia.
We further evaluated the diagnostic efficacies of each independent parameter and combinations of these factors to predict the endometrial hyperplasia patients coexisting with endometrial carcinoma by the ROC curves. As shown in Table 3, the area under curve (AUC) of ROC curve of AEH was highest (71.8%) among these factors. The AEH had better sensitivity (80.0%) and specificity (63.6%) for predicting coexisting endometrial carcinoma than those of other parameters. The positive predictive value (PPV) and negative predictive value (NPV) of AEH for coexisting endometrial carcinoma in endometrial hyperplasia were 54.5% and 49.6%, respectively.
As shown in Table 3, the combination of atypical hyperplasia and abnormal uterine bleeding had better sensitivity (76.8%) and specificity (66.7%) for predicting coexisting endometrial carcinoma in endometrial hyperplasia patients than those of other combinations. The PPV and NPV of this combination for coexisting endometrial carcinoma in endometrial hyperplasia were 47.4% and 52.6%, respectively. However, the AUC of ROC curve of AEH and history of abnormal uterine bleeding was 72.0%, which was similar to that of AEH (71.8%) (Fig. 1). Therefore, the diagnostic efficacy of AEH to predict the endometrial hyperplasia coexisting with endometrial carcinoma was better than or similar to those of other independent factors and combinations of these factors in our analysis.
The clinical and pathologic characteristics of the 125 women diagnosed as having endometrial carcinoma postoperatively were reviewed. The histological subtype of one hundred and fourteen patients (114/125, 91.2%) was endometrioid adenocarcinoma. Ninety-four patients had grade 1 disease and twenty-three had grade 2. Most cases (106/125, 84.8%) had less than one-half myometrial invasion. In our study, none of the 125 patients underwent re-staging surgery for the carcinoma. Twenty-three patients received adjuvant radiotherapy for incomplete disease staging. Six (4.8%) of the 125 women had disease relapse during the follow-up period.
The endometrial hyperplasia usually evolves by the result of protracted estrogenic stimulation without progestin influence. However, the simple hyperplasia without atypia is similar to the normal proliferative endometrium and the complex hyperplasia with nuclear atypia resembles the well differentiated endometrioid adenocarcinoma [9]. Therefore, many previous studies have exhibited that the coexisting rate of endometrial carcinoma in patients with AEH varies from 15% to 54% [7,10-13]. In our study, 100 (51.3%) out of 195 women with AEH were diagnosed as endometrial carcinoma after hysterectomy but only 25 (13.1%) out of 191 with endometrial hyperplasia without nuclear atypia had coexisting endometrial carcinoma after hysterectomy (Table 1).
In addition to low reproducibility among pathologists [1,4], complex atypical hyperplasia and well differentiated endometrioid adenocarcinoma share some molecular characteristics such as microsatellite instability and mutation of PTEN, CTNNB1, and K-ras [8,14,15]. It is difficult to definitely separate these two entities by one or a combination of these molecular markers. Furthermore, the coexisting endometrial carcinoma in patients with endometrial hyperplasia may result in inadequate surgical staging for these patients. For patient safety, more clinical information should be identified to make the physician aware of the possibility of coexisting endometrial carcinoma in patients with endometrial hyperplasia. In our study, advanced age, menopausal status, diabetes history, abnormal uterine bleeding, AEH and high BMI were independent risk factors for predicting the coexisting endometrial carcinoma (Table 2).
Previous studies have demonstrated that weight-related abnormalities, such as obesity, diabetes, and menstrual dysfunction would increase the risk of endometrial cancer [16-18]. In our study, these parameters were demonstrated to be independent risk factors for predicting the coexisting endometrial carcinoma (Table 2), but their diagnostic efficacies to predict coexisting endometrial carcinoma in endometrial hyperplasia were not adequate (Table 3). Although AEH could predict most of the endometrial hyperplasia patients with coexisting endometrial carcinoma in our analysis (Table 3), more precise biomarkers should be explored to identify this problem before hysterectomy. Recently, endometrial carcinoma has been shown to be a complex disease driven by abnormal genetic; therefore, the investigations of epigenetic and microRNAs regulation of gene expression in endometrial lesion might provide a new method to precisely identify these patients having coexisting endometrial carcinoma in endometrial hyperplasia [19,20].
In previous studies, the histology of all the patients with coexisting endometrial carcinoma in endometrial hyperplasia would be endometrioid adenocarcinoma without grade 3 disease [3,10]. However, 114 (91.2%) patients were endometrioid adenocarcinoma and 4 patients had grade 3 disease in our series. In keeping with a previous report [1], most cases (106/125, 84.8%) had less than one-half myometrial invasion. Trimble et al. [1] demonstrated that all of these cases had a good prognosis without recurrence. In our current study, 6 (4.8%) of the 125 cancer patients had disease relapse during the follow-up period, which was consistent with our previous data [7].
In this multi-center investigation, the pathologic review was the important part. Because the studied period was long (from 1991 to 2009), the qualities of some tissue samples of the studied population were not suitable for pathologic reading. Therefore, the pathologic accuracy could not be evaluated adequately. Only the risk factor analysis of coexisting endometrial carcinoma in patients with endometrial hyperplasia was presented in this study based on the medical records. This might be the reason that the numbers of hyperplasia-malignant group in non-AEH or AEH sub-groups were higher than those of published literature. It was also the limitation of this study.
In conclusion, the prognosis of coexisting endometrial carcinoma in women with endometrial hyperplasia was relatively good with a low recurrence rate. Physicians should consider the possibility of coexisting malignancy when examining endometrial hyperplasia patients with the related risk factors, especially AEH.
Figures and Tables
Fig. 1
The area under curve (AUC) of receiver operating characteristic (ROC) curve of atypical endometrial hyperplasia (AEH) was 71.8%. The AUC of ROC curve of AEH and history of abnormal uterine bleeding was 72.0%.
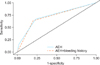
Table 1
Patient characteristics
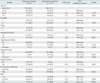
AEH, atypical endometrial hyperplasia; BMI, body mass index.
*Three missing data. †There are different criteria for applying the definition of obesity among adults in Taiwan. Using BMI categories defined by the Department of Health in Taiwan, overweight is defined as BMI ≥24, and obese is defined as BMI ≥27 (http://obesity.bhp.gov.tw/cht/index.php?code=list&ids=82).
References
1. Trimble CL, Kauderer J, Zaino R, Silverberg S, Lim PC, Burke JJ 2nd, et al. Concurrent endometrial carcinoma in women with a biopsy diagnosis of atypical endometrial hyperplasia: a Gynecologic Oncology Group study. Cancer. 2006. 106:812–819.
2. Kurman RJ, Kaminski PF, Norris HJ. The behavior of endometrial hyperplasia: a long-term study of "untreated" hyperplasia in 170 patients. Cancer. 1985. 56:403–412.
3. Montgomery BE, Daum GS, Dunton CJ. Endometrial hyperplasia: a review. Obstet Gynecol Surv. 2004. 59:368–378.
4. Baak JP, Mutter GL, Robboy S, van Diest PJ, Uyterlinde AM, Orbo A, et al. The molecular genetics and morphometry-based endometrial intraepithelial neoplasia classification system predicts disease progression in endometrial hyperplasia more accurately than the 1994 World Health Organization classification system. Cancer. 2005. 103:2304–2312.
5. Mutter GL. The Endometrial Collaborative Group. Endometrial intraepithelial neoplasia (EIN): will it bring order to chaos? Gynecol Oncol. 2000. 76:287–290.
6. Shutter J, Wright TC Jr. Prevalence of underlying adenocarcinoma in women with atypical endometrial hyperplasia. Int J Gynecol Pathol. 2005. 24:313–318.
7. Chen YL, Cheng WF, Lin MC, Huang CY, Hsieh CY, Chen CA. Concurrent endometrial carcinoma in patients with a curettage diagnosis of endometrial hyperplasia. J Formos Med Assoc. 2009. 108:502–507.
8. Announcements: FIGO stages 1988 revision. Gynecol Oncol. 1989. 35:125–126.
9. Soslow RA. Problems with the current diagnostic approach to complex atypical endometrial hyperplasia. Cancer. 2006. 106:729–731.
10. Merisio C, Berretta R, De Ioris A, Pultrone DC, Rolla M, Giordano G, et al. Endometrial cancer in patients with preoperative diagnosis of atypical endometrial hyperplasia. Eur J Obstet Gynecol Reprod Biol. 2005. 122:107–111.
11. Dunton CJ, Baak JP, Palazzo JP, van Diest PJ, McHugh M, Widra EA. Use of computerized morphometric analyses of endometrial hyperplasias in the prediction of coexistent cancer. Am J Obstet Gynecol. 1996. 174:1518–1521.
12. Kurman RJ, Norris HJ. Evaluation of criteria for distinguishing atypical endometrial hyperplasia from well-differentiated carcinoma. Cancer. 1982. 49:2547–2559.
13. Widra EA, Dunton CJ, McHugh M, Palazzo JP. Endometrial hyperplasia and the risk of carcinoma. Int J Gynecol Cancer. 1995. 5:233–235.
14. Mylonas I, Makovitzky J, Richter DU, Jeschke U, Briese V, Friese K. Expression of the inhibin-alpha subunit in normal, hyperplastic and malignant endometrial tissue: an immunohistochemical analysis. Gynecol Oncol. 2004. 93:92–97.
15. Matias-Guiu X, Catasus L, Bussaglia E, Lagarda H, Garcia A, Pons C, et al. Molecular pathology of endometrial hyperplasia and carcinoma. Hum Pathol. 2001. 32:569–577.
16. Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003. 348:1625–1638.
17. Sjostrom L, Narbro K, Sjostrom CD, Karason K, Larsson B, Wedel H, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007. 357:741–752.
18. Fader AN, Arriba LN, Frasure HE, von Gruenigen VE. Endometrial cancer and obesity: epidemiology, biomarkers, prevention and survivorship. Gynecol Oncol. 2009. 114:121–127.
19. Tao MH, Freudenheim JL. DNA methylation in endometrial cancer. Epigenetics. 2010. 5:491–498.
20. Cohn DE, Fabbri M, Valeri N, Alder H, Ivanov I, Liu CG, et al. Comprehensive miRNA profiling of surgically staged endometrial cancer. Am J Obstet Gynecol. 2010. 202:656.e1–656.e8.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download