Abstract
Objective
This study was designed to compare survival outcomes of patients with uterine papillary serous carcinoma (UPSC) or clear cell carcinoma (CC) to those of patients with grade 3 endometrioid carcinoma (G3EC) according to 1988 and 2009 International Federation of Gynecology and Obstetrics (FIGO) staging systems.
Methods
We retrospectively reviewed all patients with endometrial cancer treated at a single institution between 1995 and 2009. Among the 647 patients with endometrial cancer, 51 with G3EC and 46 with UPSC and CC histology were confirmed.
Results
1988 FIGO stage, 2009 FIGO stage, and extrauterine metastasis were significantly different between the UPSC and CC group and G3EC group (p=0.002, p=0.041, and p=0.020, respectively). Restaging from the 1988 FIGO to the 2009 FIGO criteria increased the number of stage I cases by 10 (11.0%). Overall, 8 in the UPSC and CC and 2 in the G3EC group were down-staged to stage I. In the UPSC and CC group, the 3-year overall survival for 1988 FIGO stage I was 92.9%. When UPSC and CC patients were restaged using the 2009 staging system, the 3-year overall survival of 2009 FIGO stage I dropped to 81.6%. UPSC and CC was associated with poor OS outcome compared with G3EC, after adjustment for 2009 FIGO stage and other clinicopathologic factors.
Endometrial carcinoma (EC) is the seventh most common malignancy in the world. Annually, EC develops in about 142,000 women and causes about 42,000 deaths [1]. Although the incidence of EC accounted for approximately 16% of gynecologic malignancies in Korea, its incidence has dramatically increased [2]. There were 132 registered cases of EC in 1991, 239 in 1994, 425 in 2000 and 862 in 2004 [2]. Moreover, the incidence of uterine papillary serous carcinoma (UPSC) and clear cell carcinoma (CC) has increased; its incidence accounted for 4% of all ECs in 2004 [3].
Bokhman [4] suggested that there are 2 different clinicopathologic types of EC. Type I ECs are represented by endometrioid carcinomas, which represent approximately 80% of all ECs. These tumors are estrogen related, occur in younger patients, and are associated with good prognosis. Type II ECs include poorly differentiated endometrioid adenocarcinomas, clear cell and serous cell types. These tumors are not estrogen related, are seen in older patients, and carry poor prognosis.
UPSC, CC, and grade 3 endometrioid carcinomas (G3EC) are all considered high-grade endometrial carcinomas. Although high-grade ECs are less common than low-grade ECs, they account for a disproportionate number of deaths resulting from EC [5]. Regarding survival outcomes in patients with UPSC, CC, or G3EC, previous comparison studies between these histologic types have shown disagreement. Some studies have shown that UPSC and CC is associated with an unfavorable prognosis compared with G3EC [6,7]. In contrast, a recent clinicopathologic analysis revealed no difference in outcome between UPSC and CC, and G3EC [8,9]. This dichotomy likely stems from the limited and conflicting data available.
Recently, the International Federation of Gynecology and Obstetrics (FIGO) committee reviewed 20 years of data and revised the staging criteria for carcinoma of the endometrium [10]. In two large, register-based studies from USA, the 2009 revised FIGO staging system proved to be highly prognostic with appropriate changes [11,12]. Thus, we performed restaging of the high-grade ECs from 1988 FIGO to those of 2009 FIGO and compared the clinicopathological data and the survival outcomes in patients with UPSC and CC, and G3EC.
After Institutional Review Board approval, we retrospectively reviewed electronic medical records to identify patients who underwent treatment for FIGO stage IA-IV uterine cancers at Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea between November 1995 and September 2009. A total of 647 patients with endometrial cancer were treated during this time period. Patients with histologic types of G3EC, UPSC, and CC were selected. Endometrial carcinomas of mixed subtype were excluded from this study. We grouped the population into 2 histologic groups (I-II). Group I comprised 46 cases with UPSC and CC; group II comprised 51 cases with G3EC. All patients underwent simple hysterectomy, bilateral salpingo-oophorectomy. Comprehensive surgical staging, defined as pelvic washing, removal of all gross disease implants, omentectomy (in UPSC and CC), and systematic pelvic with or without paraaortic lymphadenectomy, was performed. Stage assignment was performed according to the revised FIGO surgical staging criteria reported in 2009 [13]. Information regarding treatment, including surgery, chemotherapy and/or radiation therapy and follow-up was collected.
Adjuvant radiotherapy or adjuvant chemotherapy was used for cases with intermediate to high risk factors depending on patient preference and physician discretion. Radiotherapy was performed using vaginal brachytherapy alone (2.5 Gy in 5 fractions), whole pelvic external beam radiation alone (50.4 Gy in 28 fractions), or a combination of the two. Chemotherapy consisted of a platinum-based regimen for four to six cycles. No patients received chemotherapy or radiotherapy before surgery.
Progression-free survival (PFS) was defined as the period between initial treatment and the occurrence of pathologically-confirmed relapse. In cases where tissue sample collection was difficult, recurrence was clinically assumed when the imaging studies highly suggested recurrence and tumor markers were elevated from the basal level. Overall survival (OS) was measured from the date of surgery until death caused by the disease.
Frequency distributions between categorical variables among the groups were compared using the chi-square test. The Fisher's exact test was used if the expected frequency was <5. After the normality of the data was assessed, a two-sample t-test or Mann-Whitney test was used for the analysis of differences, depending on the distribution of the continuous variables. The survival curves were calculated according to the Kaplan-Meier method with the log-rank test. The Cox proportional-hazards model was used for the multivariable analyses. Statistical analyses were performed with SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). A p<0.05 was considered statistically significant, and all p-values were two-sided.
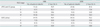
Ninety-seven cases of high-grade endometrial carcinoma were identified, including 35 UPSC, 11 CC, and 51 G3EC. The clinicopathological characteristics of the study population are listed in Table 1. After restaging from 1988 FIGO to 2009 FIGO criteria, the number of stage I cases increased by 10. Four cases classified as stage IIA based on 1988 FIGO were restaged as either 2009 FIGO IA (n=2) or 2009 FIGO IB (n=2). In this group of four, tumor subtypes were UPSC (n=2) and G3EC (n=2). Six cases classified as 1988 FIGO stage IIIA based on positive cytology only were restaged into 2009 FIGO IA (n=2) or 2009 FIGO IB (n=4). The histological subtype for these six cases was UPCS (n=6). Overall, 8 patients (17.8%) in the UPSC and CC group were down-staged to stage I, and 2 patients (4.3%) in G3EC were down-staged to stage I.
The 3-year OS for 88 and 09 FIGO stage are listed in Table 2. There were no significant OS differences when comparing the 1988 FIGO stage to the 2009 FIGO stage in G3EC group. In UPSC and CC group, there were 2 deaths among patients with 1988 FIGO stage I disease and 6 deaths among patients with 2009 FIGO stage I. Moreover, the 3-year OS rate for 2009 FIGO stage I dropped to 81.6% compared to 92.9% for 1988 FIGO stage I (Table 2).
With regard to the pathological characteristics, there were no differences in tumor size in the uterus, myometrial involvement, lymphovascular space invasion, cervical stromal invasion, or lymph node metastases. However, disease spread beyond the uterus was significantly more frequent in UPSC and CC than in G3EC (41.3% vs.19.6%, p=0.020). There was no significant difference in the median age between those in the UPSC and CC group and G3EC group (61 vs. 57, p=0.092). The types of adjuvant therapy after primary surgery were unequally distributed; patients with G3EC more frequently received postoperative radiotherapy (32.6% vs. 62.7%, p<0.001), and those with UPSC and CC more frequently received postoperative chemotherapy (39.1% vs. 5.9%, p=0.001).
The median follow-up duration was 35.0 months (range, 1.1 to 177.8 months). The 75th percentile for follow-up months was 53. The median time to recurrence was 30.5 and 35.1 months in UPSC and CC, and G3EC, respectively. The death rate was 39.1% (18/46) for UPSC and CC, and 21.6% (11/51) for G3EC (p=0.059). The recurrence rate was 37.0% (17/46) for UPSC and CC, and 19.6% (10/51) for G3EC (p=0.057). The pattern of recurrence was not different between the two groups (Table 3). Two locoregional and four lymphatic recurrences were found in UPSC and CC patients, and one locoregional and three lymphatic recurrences were found in G3EC patients. The two groups had more hematogenous distant failure than locoregional or lymphatic failure (UPSC and CC, 11/17 [64.7%] and G3EC, 6/10 [60%]). In most cases of recurrence, adjuvant therapy (radiotherapy, chemotherapy, or a combination of both) was performed with the initial surgery (UPSC and CC, 16/17 [94.1%] and G3EC, 10/10 [100%]; p>0.05).
Overall, UPSC and CC was associated with poor OS outcome compared with G3EC, even after adjustment for 2009 FIGO stage and other clinicopathologic factors (Fig. 1). In univariate analysis, histologic type UPSC and CC, 2009 FIGO stage of III-IV, and positivity for LVSI were negatively associated with PFS, as well as OS (Table 4, Fig. 2). In multivariate analysis, these variables were consistently independent factors in OS (Table 4). There was no difference in PFS or OS when comparing UPSC and CC with G3EC after adjusting for 1988 FIGO stage and other clinicopathologic factors (Fig. 1). 1988 FIGO advanced-stage disease had the strongest negative impact on survival (hazard ratio [HR], 8.99; 95% confidence interval [CI], 2.66 to 30.37, p<0.001).
In this study, we found that the UPSC and CC had a worse prognosis than G3EC when patients were restaged using the 2009 FIGO staging system and this difference disappeared in patients with the 1988 FIGO staging system. Moreover, in UPSC and CC group, the 3-year OS rate for 2009 FIGO stage I dropped to 81.6 % compared to 92.9% for 1988 FIGO stage I.
UPSC, CC, and G3EC have been identified as high-grade endometrial cancers and account for the majority of uterine cancer deaths [6]. Recently, Song et al. [14] suggested that UPSCs had similar clinicopathologic features compared to the patients with carcinosarcomas in the same study group. The 5-year survival rates of our patients and those from prior studies are summarized in Table 5 [6-9,15-21]. Some studies have shown that patients with UPSC or CC had a significantly poorer prognosis compared with that of patients with G3EC [6,7,20,21], while other studies revealed no difference in outcome between UPSC and CC, and G3EC [8,9,16-19]. When compared to type I ECs, type II ECs are mostly represented by UPSC and CC, are more likely to present with metastatic disease at diagnosis, and have a poorer prognosis [8]. However, the molecular profile of G3EC has not yet been well characterized and G3EC does not clearly fit into either definition of type I or type II cancer. These controversies in classification have consequently generated conflicting results regarding the prognosis of these tumors.
In current study, comprehensive surgical staging was performed in both groups (G3EC vs. UPSC and CC) with pelvic and/or para-aortic lymph node dissection: 100% of the G3EC and 91.1% of the UPSC and CC patients. Moreover, the same proportion of patients in both groups (G3EC, 84.8%; UPSC and CC, 84.4%) submitted to adjuvant treatment, although a greater propensity for chemotherapy was observed in UPSC and CC patients. Since UPSC shows similar behaviors and spread patterns to serous papillary carcinoma of the ovary, comprehensive surgical staging in UPSC patients was suggested to more reliably predict extrauterine spread [22-25]. Recently, a variety of reports showed that platinum-based chemotherapy in combination with paclitaxel was the most effective adjuvant treatment modality in stage I-IV UPSC patients [26-30].
We observed that UPSC and CC had a worse prognosis than G3EC when restaged to the 2009 FIGO criteria. There were no differences in PFS and OS when comparing UPSC and CC with G3EC after adjusting for 1988 FIGO stage. Only 1988 FIGO high-stage disease had a strong negative impact on survival (HR, 8.99; 95% CI, 2.66 to 30.37; p<0.001). These results might be from that more patients with a poor prognosis were down-staged in a UPSC and CC group. The goal of combining the 1988 FIGO stages IA, IB, IIA, and IIIA with positive cytology-only subgroups in the 2009 FIGO criteria was to create a more streamlined staging system that merged groups with similar survival rates [13]. Several studies have demonstrated that the 2009 FIGO staging system has improved prognosis predictions and is less complex than earlier FIGO versions [11,12,31]. However, some of these studies did not include serous or clear cell histologic types [10,11]. In a study by Werner et al. [31], which included both UPSC and CC, the majority of non-endometrioid tumors that were down-staged to 2009 FIGO stage I were of serous histology. For 2009 FIGO stage IA patients, the 5-year survival rate was 45.8% for those in the serous histology subgroup (n=47). Of our patients, 8 of 10 that were down-stage to 2009 FIGO stage I were UPSC and CC, including 6 cases classified as 1988 FIGO stage IIIA based on positive cytology only. For the 2009 FIGO stage IA patients, the 5-year OS rate was 53.8% for the UPSC and CC subgroup. Mariani et al. [32] showed that disease-specific survival did not differ between stage IIIA cancer patients with positive cytology only (stage IIIA1) and those with uterine serosal invasion or adnexal spread (stage IIIA2). Moreover, patients who had stage IIIA1 disease with a non-endometrioid histologic type or LVSI (or both) had a significant frequency of extra-abdominal failure.
Recent relevant studies have reported the prognostic value of the 2009 FIGO staging criteria by comparing with the 1988 staging criteria of endometrial cancer. Lewin et al found the new staging criteria to appropriately delineate prognostic features [11]. On the other hand, Abu-Rustum et al. [33] evaluated their single-institution database and found that the revised system for stage I did not improve its predictive ability over the 1988 system. Seward et al. [34] evaluated the prognostic impact of these changes on the UPSC and reported that the 2009 FIGO criteria do not adequately delineate survival for UPSC in early-stage disease. They suggested that UPSC should continue to be staged with the more informative 1988 FIGO criteria.
This study had some limitations. First, there may be a recall bias due to the retrospective design of the study. Second, the type of adjuvant therapy was unequally distributed. Third, the number of patients was relatively small, which may have affected the results. The observation from this small series calls for a large, multi-institutional investigation.
In conclusion, we observed that UPSC and CC patients had different prognosis according to the old and new FIGO staging system. Our results suggest that UPSC and CC compared with the G3EC may retain the 1988 FIGO to be a slightly better discriminator than 2009 FIGO. Further large studies to evaluate the prognostic significance of these new criteria are needed in the future.
Figures and Tables
Fig. 1
Overall survival curve based on histologic type after adjusting for clinicopathologic factors. (A) Comparison between uterine papillary serous carcinoma (UPSC) and clear cell carcinoma (CC) and grade 3 endometrioid carcinoma (G3EC) in International Federation of Gynecology and Obstetrics (FIGO) 1988 (A) and 2009 (B) staging systems.

Fig. 2
Univariate analysis for survival outcome according to the histologic type. G3EC, grade 3 endometrioid carcinoma; UPSC, uterine papillary serous carcinoma; CC, clear cell carcinoma. (A) Proression-free survival, (B) Overall suvival.

Table 4
Univariate and multivariate analyses for survival outcomes according to individual parameters

References
1. Amant F, Moerman P, Neven P, Timmerman D, Van Limbergen E, Vergote I. Endometrial cancer. Lancet. 2005. 366:491–505.
2. Lee HP. Annual report of gynecologic cancer registry program in Korea: 1991~2004. Korean J Obstet Gynecol. 2008. 51:1411–1420.
3. SOG Gynecologic Oncology Committee. Annual report of gynecologic cancer registry program in Korea for 2004 (Jan. 1st, 2004-Dec. 31st, 2004). Korean J Obstet Gynecol. 2007. 50:28–78.
4. Bokhman JV. Two pathogenetic types of endometrial carcinoma. Gynecol Oncol. 1983. 15:10–17.
5. Tavassoli FA, Devilee P. WHO classification of tumors: pathology and cenetics. Tumors of the breast and female genital organs. 2003. Lyon: International Agency for Research on Cancer Press.
6. Hamilton CA, Cheung MK, Osann K, Chen L, Teng NN, Longacre TA, et al. Uterine papillary serous and clear cell carcinomas predict for poorer survival compared to grade 3 endometrioid corpus cancers. Br J Cancer. 2006. 94:642–646.
7. Boruta DM 2nd, Gehrig PA, Groben PA, Bae-Jump V, Boggess JF, Fowler WC Jr, et al. Uterine serous and grade 3 endometrioid carcinomas: is there a survival difference? Cancer. 2004. 101:2214–2221.
8. Soslow RA, Bissonnette JP, Wilton A, Ferguson SE, Alektiar KM, Duska LR, et al. Clinicopathologic analysis of 187 high-grade endometrial carcinomas of different histologic subtypes: similar outcomes belie distinctive biologic differences. Am J Surg Pathol. 2007. 31:979–987.
9. Voss MA, Ganesan R, Ludeman L, McCarthy K, Gornall R, Schaller G, et al. Should grade 3 endometrioid endometrial carcinoma be considered a type 2 cancer-a clinical and pathological evaluation. Gynecol Oncol. 2012. 124:15–20.
10. Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. 2009. 105:103–104.
11. Lewin SN, Herzog TJ, Barrena Medel NI, Deutsch I, Burke WM, Sun X, et al. Comparative performance of the 2009 international Federation of gynecology and obstetrics' staging system for uterine corpus cancer. Obstet Gynecol. 2010. 116:1141–1149.
12. Cooke EW, Pappas L, Gaffney DK. Does the revised International Federation of Gynecology and Obstetrics staging system for endometrial cancer lead to increased discrimination in patient outcomes? Cancer. 2011. 117:4231–4237.
13. Creasman W. Revised FIGO staging for carcinoma of the endometrium. Int J Gynaecol Obstet. 2009. 105:109.
14. Song T, Choi CH, Lee YY, Kim TJ, Lee JW, Kim BG, et al. Which is worse: uterine papillary serous carcinomas or carcinosarcomas? J Gynecol Oncol. 2011. 22:83–88.
15. Carcangiu ML, Chambers JT. Early pathologic stage clear cell carcinoma and uterine papillary serous carcinoma of the endometrium: comparison of clinicopathologic features and survival. Int J Gynecol Pathol. 1995. 14:30–38.
16. Cirisano FD Jr, Robboy SJ, Dodge RK, Bentley RC, Krigman HR, Synan IS, et al. The outcome of stage I-II clinically and surgically staged papillary serous and clear cell endometrial cancers when compared with endometrioid carcinoma. Gynecol Oncol. 2000. 77:55–65.
17. Alektiar KM, McKee A, Lin O, Venkatraman E, Zelefsky MJ, McKee B, et al. Is there a difference in outcome between stage I-II endometrial cancer of papillary serous/clear cell and endometrioid FIGO Grade 3 cancer? Int J Radiat Oncol Biol Phys. 2002. 54:79–85.
18. Halperin R, Zehavi S, Langer R, Hadas E, Bukovsky I, Schneider D. Uterine papillary serous carcinoma (pure and mixed type) compared with moderately and poorly differentiated endometrioid carcinoma. A clinicopathologic study. Eur J Gynaecol Oncol. 2002. 23:300–304.
19. Creasman WT, Kohler MF, Odicino F, Maisonneuve P, Boyle P. Prognosis of papillary serous, clear cell, and grade 3 stage I carcinoma of the endometrium. Gynecol Oncol. 2004. 95:593–596.
20. Alkushi A, Kobel M, Kalloger SE, Gilks CB. High-grade endometrial carcinoma: serous and grade 3 endometrioid carcinomas have different immunophenotypes and outcomes. Int J Gynecol Pathol. 2010. 29:343–350.
21. Greggi S, Mangili G, Scaffa C, Scala F, Losito S, Iodice F, et al. Uterine papillary serous, clear cell, and poorly differentiated endometrioid carcinomas: a comparative study. Int J Gynecol Cancer. 2011. 21:661–667.
22. Bristow RE, Asrari F, Trimble EL, Montz FJ. Extended surgical staging for uterine papillary serous carcinoma: survival outcome of locoregional (Stage I-III) disease. Gynecol Oncol. 2001. 81:279–286.
23. Schwartz PE. The management of serous papillary uterine cancer. Curr Opin Oncol. 2006. 18:494–499.
24. Hamilton CA, Liou WS, Osann K, Berman ML, Husain A, Teng NN, et al. Impact of adjuvant therapy on survival of patients with early-stage uterine papillary serous carcinoma. Int J Radiat Oncol Biol Phys. 2005. 63:839–844.
25. Chan JK, Loizzi V, Youssef M, Osann K, Rutgers J, Vasilev SA, et al. Significance of comprehensive surgical staging in noninvasive papillary serous carcinoma of the endometrium. Gynecol Oncol. 2003. 90:181–185.
26. Fader AN, Starks D, Gehrig PA, Secord AA, Frasure HE, O'Malley DM, et al. An updated clinicopathologic study of early-stage uterine papillary serous carcinoma (UPSC). Gynecol Oncol. 2009. 115:244–248.
27. Kelly MG, O'malley DM, Hui P, McAlpine J, Yu H, Rutherford TJ, et al. Improved survival in surgical stage I patients with uterine papillary serous carcinoma (UPSC) treated with adjuvant platinum-based chemotherapy. Gynecol Oncol. 2005. 98:353–359.
28. Fader AN, Drake RD, O'Malley DM, Gibbons HE, Huh WK, Havrilesky LJ, et al. Platinum/taxane-based chemotherapy with or without radiation therapy favorably impacts survival outcomes in stage I uterine papillary serous carcinoma. Cancer. 2009. 115:2119–2127.
29. Fields AL, Einstein MH, Novetsky AP, Gebb J, Goldberg GL. Pilot phase II trial of radiation "sandwiched" between combination paclitaxel/platinum chemotherapy in patients with uterine papillary serous carcinoma (UPSC). Gynecol Oncol. 2008. 108:201–206.
30. Roelofsen T, van Ham MA, de Hullu JA, Massuger LF. Clinical management of uterine papillary serous carcinoma. Expert Rev Anticancer Ther. 2011. 11:71–81.
31. Werner HM, Trovik J, Marcickiewicz J, Tingulstad S, Staff AC, Amant F, et al. Revision of FIGO surgical staging in 2009 for endometrial cancer validates to improve risk stratification. Gynecol Oncol. 2012. 125:103–108.
32. Mariani A, Webb MJ, Keeney GL, Aletti G, Podratz KC. Assessment of prognostic factors in stage IIIA endometrial cancer. Gynecol Oncol. 2002. 86:38–44.
33. Abu-Rustum NR, Zhou Q, Iasonos A, Alektiar KM, Leitao MM Jr, Chi DS, et al. The revised 2009 FIGO staging system for endometrial cancer: should the 1988 FIGO stages IA and IB be altered? Int J Gynecol Cancer. 2011. 21:511–516.
34. Seward S, Ali-Fehmi R, Munkarah AR, Semaan A, Al-Wahab ZR, Elshaikh MA, et al. Outcomes of patients with uterine serous carcinoma using the revised FIGO staging system. Int J Gynecol Cancer. 2012. 22:452–456.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download