Abstract
Objective
To evaluate survival and morbidity after pelvic exenteration (PE) for the curative management of recurrent cervical cancer.
Methods
We retrospectively evaluated patients with recurrent cervical cancer who underwent PE from January 2001 to April 2011. Patients were identified from the registry of our institution. The clinical status and demographic information was obtained by reviewing the medical records.
Results
Sixty-one recurrent cervical cancer patients underwent PE. Patients who received radiotherapy, operation, chemotherapy before PE were 98%, 41%, and 23%, respectively. The total morbidity rate was 44%; 10 (16%) patients had early complications (30 days or less after PE), whereas 22 (36%) patients had late complications. Wound problems were common early complications (7/18), and bowel fistulas were common late complications (9/30). The five-year overall survival and five-year disease-free survival were 56% and 49%, respectively. Median follow-up was 22 months (range, 1.8 to 60 months). Affecting factors for overall survival were resection margin status, pelvic wall and rectal involvement.
Conclusion
Our overall 5-year survival is encouraging. Although the morbidity rate is still high, PE is a potentially curative opportunity in gynecological malignancies with no other treatment options. The most important factors for overall survival after PE are the resection margin status, pelvic wall involvement and rectal involvement.
Pelvic exenteration (PE) is an ultraradical surgery pioneered first in gynecological oncology in 1948 by Brunschwig [1] for advanced cancer. This surgery removes basically all the pelvic organs including not only the uterus, ovaries, and vagina, but also the adjacent organs, which are bladder and rectosigmoid colon. However, the procedure was purely palliative and the operation resulted in the long-term survival of only a few patients [1].
Over the following 60 years, the improvement in surgical techniques, perioperative management, and selection criteria led to significant improvements in perioperative mortality, long-term survival, and quality of life [2,3]. Subsequently, the surgical procedure has evolved from a purely total exenteration to an operation that includes a reconstructive phase with urinary diversion, colon-sparing surgery, anal sphincter preservation, and pelvic floor reconstruction. Today, PE is considered to be a feasible procedure that offers life to selected patients for whom no other possibility of cure is available. The goal of PE has been mainly shifted from a palliative procedure to a potentially curative one. However, the reported morbidity rates still remain high [4-6], and reports regarding surgical procedures and outcome from various institutions lack coherence [7-12].
The risk factors for poor prognosis in PE have been reported by number of studies [7-10]. We previously described the role of PE for advanced or recurrent gynecologic malignancy and pointed out that tumor size exceeding 4 cm, margin status, and lymph node metastasis affected the survival rate [13]. However, no other studies showed consistent results of these factors. In this study, we reviewed the patients who underwent PE performed by the gynecological oncology division in a single institution. The goal of the study was to determine patient characteristics, surgical outcome, survival, recurrence, and complications in curative PE treatment.
We thoroughly reviewed medical records of 61 patients who underwent PE at National Cancer Center, Korea, from January 2000 through April 2011 for recurrent cervical cancer. Thirty three out of 61 patients were analyzed and reported in 2007 [13]. Approval for this retrospective study was given by the Institutional Review Board (NCCNCS-11-537). Patients underwent a thorough preoperative assessment to evaluate their general medical status and indication for surgery. The primary indication for PE is recurrent cervical cancer without distant metastasis. Patients underwent computed tomography (CT) or magnetic resonance imaging (MRI) of the pelvis and abdomen to evaluate the disease extent and to estimate the likely extent of surgery, and positron emission tomogram (PET) or PET-CT to identify metastatic disease. Images and biopsy results were discussed at the tumor board-a multidisciplinary team meeting of a gynecological oncologist, radiation oncologist, diagnostic radiologist, pathologist, and a nuclear medicine physician. Pelvic lesions and suspected metastatic lesions (the presence of which generally precluded surgery) underwent histological confirmation. Once surgical management was considered indicated, the procedure was discussed at length with the patient. The patient was provided with full details regarding the nature of the operation and its consequences. A psychologist evaluated the mental and psychological status of patients. All surgical procedures were performed by gynecological oncologists with curative intentions, who collaborated with the urologists and general and plastic surgeons. For each patient, the following characteristics were recorded; age at the time of procedure, primary cancer histology, site and size of recurrence, history of previous treatments, timing between primary diagnosis and relapse, type of operation, performed reconstructive techniques, pathology, complications, and the interval time from surgery to last follow-up or death.
PE was classified as anterior, posterior, and total PE. Anterior PE was referred to the removal of the reproductive tract and the bladder. Posterior PE was referred to the removal of the reproductive tract along with the rectosigmoid colon. And the total PE was referred to the removal of the reproductive tract, bladder, and rectosigmoid colon.
Surgical parameters, including PE type, duration of surgery, total blood loss, number of transfusions, intraoperative complications, and the length of hospital stay were evaluated. The post-operative morbidity was categorized as early (≤30 days after operation) or late (>30 days after operation). Overall survival (OS) time was calculated as months from the date of surgery to death or the date censored. Disease-free survival (DFS) time was calculated as months from the date of surgery to the date of recurrence.
Descriptive statistics are reported as frequencies and percentages or mean and standard deviations. The association between OS and PE was estimated using the method of Kaplan-Meier and assessed using the log-rank test. The Cox proportional hazards model was also used to adjust for resection margin status, pelvic wall and rectal involvement. All statistical testing was conducted at the 0.05 confidence level with SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA).
From January 2001 to April 2011, 61 patients who had recurrent cervical cancer underwent PE. The initial FIGO stage of patients who underwent PE was I (9/61), II (20/61), III (6/61), IV (3/61), and unknown (23/61). The type of initial treatment was radical hysterectomy (6/61), radiotherapy (33/61), radical hysterectomy and adjuvant radiotherapy (19/61), and neoadjuvant chemotherapy plus radical hysterectomy and adjuvant radiotherapy (3/61). And 13% of the patients had undergone chemotherapy (8/61), 13% had undergone radiotherapy (8/61), and 3% (2/61) had undergone hysterectomy before PE after recurrence. Ninety-eight percent of the patients who underwent PE had undergone radiotherapy (60/61). One patient had left sided pelvic cavity recurrence with bladder wall invasion due to large irregular mass. She had a large vesicovaginal fistula. This patient had undergone PE without radiotherapy due to the consideration for the quality of life after treatment. Forty-two (69%) patients had undergone total PE, 17 (28%) anterior PE, and 2 (3%) posterior PE (Table 1).
The median age at operation time was 61 years (range, 29 to 77 years). The median time from primary diagnosis to relapse was 34.1 months. The median estimated blood loss (EBL) was 1,089 mL (range, 150 to 6,200 mL). The median number of intraoperatively given red blood cell unit was 4. The median operation time was 10 hours. The median hospital stay was 34 days (range, 13 to 118 days) (Table 1). No perioperative (≤30 days after surgery) death was observed.
After radical surgery, 27 (44%) patients underwent pelvic reconstructive surgery using autologous tissue flaps, of which the following types were used: omental flaps, 17 (22.9%); vertical rectus abdominus myocutaneous flaps, 5 (6.0%); gracilis myocutaneous flaps, 4 (4.8%); and transverse rectus abdominus myocutaneous flaps, 1 (1.2%). A bilateral pudendal thigh flap and a split thickness skin graft were used in 1 patient for vaginal reconstructive surgery. Of the flap patients, three underwent neovagina creation using a pedicled myocutaneous flap (1 vertical rectus abdominus myocutaneous flap, 2 gracilis myocutaneous flaps). For fecal diversion, 35 (57%) patients underwent a colostomy. Six (10%) patients underwent primary low colorectal anastomosis. Among these, 4 patients underwent a prophylactic ileostomy. For urinary diversion, 59 (97%) patients underwent ileal conduit formation; no patients underwent a continent urinary diversion. Patients who had resection margin involvement underwent adjuvant chemotherapy or radiotherapy after PE.
Early and late complications are summarized in Table 2. The overall morbidity rate was 44%. Early postoperative complications, defined as occurring within 30 days of surgery, were present in 10 (16%) patients. Wound problem was the most common early complication, occurring in 7 (11%) patients. Complications other than wound problem were seen in 6 (10%) patients: 5 fistulas and 1 ileus. Late postoperative complications, defined as occurring after 30 days of surgery, were present in 22 (36%) patients. Common late complications included 10 fistulas, 5 bowel obstructions, and 5 ileuses. Among 10 fistulas in late complications, 8 were benign fistulas due to severe adhesion and 2 were malignant fistulas due to tumor invasion. All rectovaginal fistulas in late complication were caused by tumor invasion. The median time from PE to fistula was 3.5 months (range, 1 to 48 months). Type of exenteration did not show the difference of morbidity.
The median follow-up time was 22 months (range, 1 to 60 months). Five-year OS was 56% and five-year DFS was 49%. After PE, 8 patients had pelvic and distant recurrences, including 3 lungs, 2 lymph nodes, 1 bone, and 1 omentum. Twenty patients had multiple distant recurrences. The median time to recurrence from PE was 6.1 months (range, 0.7 to 47.8 months). Only one case was a localized pelvic recurrence. Treatment included the following: chemotherapy, 1; surgery and chemotherapy, 1; radiation therapy and chemotherapy, 7; and hospice management, 12. Eighteen patients died from the disease. The median time from PE to death was 6.5 months (range, 0.1 to 58.2 months).
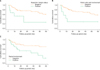
DFS and OS were analyzed in terms of considerable clinical and histopathological factors and common complications that might have affected survival. Only variables that were p<0.1 at univariate analysis were used for multivariate analysis. Multivariate analysis found that resection margin status, pelvic wall involvement and rectal involvement were significantly associated with OS (p=0.043, 0.037, and 0.044, respectively) (Table 3). Univariate analysis showed that pelvic wall invasion and rectal involvement were associated with DFS (p=0.002 and 0.044, respectively), and that resection margin status and bladder wall invasion did not show the significance but revealed the borderline significance (p=0.058 and 0.054, respectively) (Table 3). Multivariate analysis of pelvic wall involvement, rectal involvement, resection margin status and bladder wall invasion found that pelvic wall involvement and rectal involvement affected DFS (p=0.010 and 0.008, respectively) (Table 3). Exenteration type, tumor size, lymphovascular space involvement, pelvic lymph node involvement, bladder involvement and parametrium involvement were not affected the OS and DFS in multivariate analysis. The median survival times of patients who had resection margin positive status, pelvic wall invasion and rectal involvement were 9.4, 9.5, and 14.3 months, respectively (Fig. 1). Among the patients who underwent margin free resection, rectal involvement affected OS (p=0.007) and bladder/rectal involvement affected DFS in univariate analysis (p=0.039 and 0.001, respectively).
PE is the only optimal treatment for some patients with advanced or recurrent gynecological malignancies. Our findings of 56% 5-year survival and 44% morbidity in these patients are similar to previous results [2,3,7,11]. Many previous studies reported survival outcomes and morbidities of approximately 30-60% and 40-83%, respectively [2,3,7,11,14]. Carefully selected patients, meticulous operative techniques, improved surgical instruments, and intensive postoperative management might have improved both the survival rate and morbidity [15]. However, the morbidity of PE was still high (Table 4). As PE might be a potentially curative option for some patients with advanced gynecological malignancies, further studies will be needed to decrease the morbidity.
Some studies reported that the majority of early complications were caused by infections, and common late complications were urinary tract infections and fistulas [2,7,13]. Many factors, including long duration of operation, type of catheter placement, and massive internal organ handling, were more commonly caused by wound and urinary tract infections. The infection rates were decreased by better patient selection, antibiotics usage, and improved antiseptic and operative techniques [7,16,17]. Tumor recurrence and postoperative adhesion were common causes of fistulas. Some studies reported that pelvic reconstructive surgery might have reduced fistula formation [18,19]. However, effective preventive methods for fistula formation have not yet been reported. In the present study, common early complication was wound dehiscence due to infection. Common late complications were fistulas and intestinal obstructions. Late intestinal obstructions and fistulas were commonly the results of adhesions and tumor recurrence. In our study, all intestinal obstruction and fistulas, except for rectovaginal fistula, that occurred in late complication were caused by severe adhesion. Two rectovaginal fistulas were caused by tumor invasion. We suggest the mechanism of fistula formation to be the elevated pressure on the weakest portion of the small bowel, which might be impacted and adhesive in the large gap left by PE in the pelvic floor. A further study is warranted to confirm this speculation.
In our study, 44% of patients underwent reconstructive surgery in the pelvis or vagina using an autologous tissue flap (such as an omental flap or pedicled muscle transposed into the pelvis and perineum). The frequency of pelvis or vagina reconstruction in our series was lower than other studies that recommended pelvic floor reconstruction for reducing complications [18,19]. The causes of the low reconstruction frequency were that the patients did not opt a neovagina in fear of increased morbidity and refused the intercourse any more. Park et al. [13] previously reported that informing patients about the morbidity, the possibility of intercourse after operation, and the procedure by an experienced surgeon were very important for pelvic reconstructive surgery. Prospective studies showing that pelvic reconstruction reduces operative morbidity will be needed, and physicians should try to share as much information as possible with patients.
Number of clinical factors was reported that affect poor prognosis in the patients who undergo PE [2,20-23]. However, no other factor except for margin involvement was consistently identified to be established risk factor for poor prognosis. In the current series, multivariate analysis showed that resection margin status, pelvic wall involvement and rectal involvement affected OS. Indeed, resection margin status should be an important factor for poor prognosis. Many studies reported pelvic wall involvement was also associated with high overall mortality [24-26]. Mourton et al. [27] reported that rectal involvement was an affecting factor of OS. Although these factors are identified across a number of studies, not all studies consistently identify all of these factors. Many factors affecting the prognosis in PE await confirmation by further prospective studies.
We recognize that our study has certain limitations. First, we have collected the date retrospectively presumably leading to a selection bias. Second, this study might be similar to our previous report. However, the subjects were limited to be the recurrent cervical cancer patients who had undergone radiotherapy in contrast to the several types of gynecologic oncology primary cases that were included in the previous report. Third, we did not assess the survival rate affected by fistulas because of the limited sample size. In this study, all fistulas, except for rectovaginal fistula caused by tumor invasion, occurred in late complications caused by severe adhesions. Without reference to the exact cause of fistulas, we can only presume that bowel fistulas are associated with lower quality of life and high overall mortality. Further studies will be needed to confirm this association. Despite the limitations, this study established the fact that constant affecting factors for survival rate are resection margin status and pelvic wall involvement.
In our series, PE represents a feasible therapeutic surgical opportunity with optimal long-term survival. Although the morbidity rate still remains significantly high, PE may provide the only hope for a cure with some advanced or recurrent pelvic malignancies. Resection margin status, pelvic wall involvement and rectal involvement are significant affecting factors for OS after PE.
Figures and Tables
Fig. 1
Overall survival by resection margin status (negative margin, n=52 vs. positive margin, n=9) (A); pelvic side wall involvement (negative, n=54 vs. positive, n=7) (B); and rectal involvement (negative, n=41 vs. positive, n=20) (C) after adjustment for resection margin status, pelvic side wall involvement and rectal involvement (Cox regression model, p=0.043, p=0.037, and p=0.044, respectively). In 2007, 33 out of 61 present cases were analyzed and reported.
References
1. Brunschwig A. Complete excision of pelvic viscera for advanced carcinoma: a one-stage abdominoperineal operation with end colostomy and bilateral ureteral implantation into the colon above the colostomy. Cancer. 1948. 1:177–183.
2. Morley GW, Hopkins MP, Lindenauer SM, Roberts JA. Pelvic exenteration, University of Michigan: 100 patients at 5 years. Obstet Gynecol. 1989. 74:934–943.
3. Stanhope CR, Webb MJ, Podratz KC. Pelvic exenteration for recurrent cervical cancer. Clin Obstet Gynecol. 1990. 33:897–909.
4. Houvenaeghel G, Moutardier V, Karsenty G, Bladou F, Lelong B, Buttarelli M, et al. Major complications of urinary diversion after pelvic exenteration for gynecologic malignancies: a 23-year mono-institutional experience in 124 patients. Gynecol Oncol. 2004. 92:680–683.
5. Kraybill WG, Lopez MJ, Bricker EM. Total pelvic exenteration as a therapeutic option in advanced malignant disease of the pelvis. Surg Gynecol Obstet. 1988. 166:259–263.
6. Bladou F, Houvenaeghel G, Delpero JR, Guerinel G. Incidence and management of major urinary complications after pelvic exenteration for gynecological malignancies. J Surg Oncol. 1995. 58:91–96.
7. Berek JS, Howe C, Lagasse LD, Hacker NF. Pelvic exenteration for recurrent gynecologic malignancy: survival and morbidity analysis of the 45-year experience at UCLA. Gynecol Oncol. 2005. 99:153–159.
8. Roos EJ, Van Eijkeren MA, Boon TA, Heintz AP. Pelvic exenteration as treatment of recurrent or advanced gynecologic and urologic cancer. Int J Gynecol Cancer. 2005. 15:624–629.
9. Sharma S, Odunsi K, Driscoll D, Lele S. Pelvic exenterations for gynecological malignancies: twenty-year experience at Roswell Park Cancer Institute. Int J Gynecol Cancer. 2005. 15:475–482.
10. Goldberg GL, Sukumvanich P, Einstein MH, Smith HO, Anderson PS, Fields AL. Total pelvic exenteration: the Albert Einstein College of Medicine/Montefiore Medical Center Experience (1987 to 2003). Gynecol Oncol. 2006. 101:261–268.
11. Maggioni A, Roviglione G, Landoni F, Zanagnolo V, Peiretti M, Colombo N, et al. Pelvic exenteration: ten-year experience at the European Institute of Oncology in Milan. Gynecol Oncol. 2009. 114:64–68.
12. Benn T, Brooks RA, Zhang Q, Powell MA, Thaker PH, Mutch DG, et al. Pelvic exenteration in gynecologic oncology: a single institution study over 20 years. Gynecol Oncol. 2011. 122:14–18.
13. Park JY, Choi HJ, Jeong SY, Chung J, Park JK, Park SY. The role of pelvic exenteration and reconstruction for treatment of advanced or recurrent gynecologic malignancies: analysis of risk factors predicting recurrence and survival. J Surg Oncol. 2007. 96:560–568.
14. Fleisch MC, Pantke P, Beckmann MW, Schnuerch HG, Ackermann R, Grimm MO, et al. Predictors for long-term survival after interdisciplinary salvage surgery for advanced or recurrent gynecologic cancers. J Surg Oncol. 2007. 95:476–484.
15. Einenkel J, Holler B, Hoffmeister A. Sonographic diagnosis and endo-sponge assisted vacuum therapy of anastomotic leakage following posterior pelvic exenteration for ovarian cancer without using a protective stoma. J Gynecol Oncol. 2011. 22:131–134.
16. Galante M, Hill EC. Pelvic exenteration: a critical analysis of a ten-year experience with the use of the team approach. Trans Pac Coast Obstet Gynecol Soc. 1970. 38:59–68.
17. Evans RP, Clyburn TA, Moucha CS, Prokuski L. Surgical site infection prevention and control: an emerging paradigm. Instr Course Lect. 2011. 60:539–543.
18. Salom EM, Penalver MA. Pelvic exenteration and reconstruction. Cancer J. 2003. 9:415–424.
19. Momoh AO, Kamat AM, Butler CE. Reconstruction of the pelvic floor with human acellular dermal matrix and omental flap following anterior pelvic exenteration. J Plast Reconstr Aesthet Surg. 2010. 63:2185–2187.
20. Anthopoulos AP, Manetta A, Larson JE, Podczaski ES, Bartholomew MJ, Mortel R. Pelvic exenteration: a morbidity and mortality analysis of a seven-year experience. Gynecol Oncol. 1989. 35:219–223.
21. Rutledge FN, Smith JP, Wharton JT, O'Quinn AG. Pelvic exenteration: analysis of 296 patients. Am J Obstet Gynecol. 1977. 129:881–892.
22. Shingleton HM, Soong SJ, Gelder MS, Hatch KD, Baker VV, Austin JM Jr. Clinical and histopathologic factors predicting recurrence and survival after pelvic exenteration for cancer of the cervix. Obstet Gynecol. 1989. 73:1027–1034.
23. Roberts WS, Cavanagh D, Bryson SC, Lyman GH, Hewitt S. Major morbidity after pelvic exenteration: a seven-year experience. Obstet Gynecol. 1987. 69:617–621.
24. Mitulescu G, Ungureanu C, Gluck G, Stingu C, Mitulescu D, Stanculeanu D, et al. Total pelvic exenteration in the treatment of advanced pelvic cancer. Chirurgia (Bucur). 2007. 102:143–154.
25. Moriya Y, Akasu T, Fujita S, Yamamoto S. Aggressive surgical treatment for patients with T4 rectal cancer. Colorectal Dis. 2003. 5:427–431.
26. Yamada K, Ishizawa T, Niwa K, Chuman Y, Akiba S, Aikou T. Patterns of pelvic invasion are prognostic in the treatment of locally recurrent rectal cancer. Br J Surg. 2001. 88:988–993.
27. Mourton SM, Chi DS, Sonoda Y, Alektiar KM, Venkatraman ES, Barakat RR, et al. Mesorectal lymph node involvement and prognostic implications at total pelvic exenteration for gynecologic malignancies. Gynecol Oncol. 2006. 100:533–536.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download