Abstract
Objective
The purpose of this retrospective study was to assess the tolerability and efficacy of sequential chemotherapy and radiotherapy for the treatment of high risk endometrial cancer.
Methods
We conducted a retrospective study of previously untreated high risk endometrial cancer patients who received sequential chemotherapy and radiotherapy in accordance with the sandwich approach from June 2008 until June 2011. High risk endometrial cancer patients underwent complete surgical staging followed by adjuvant therapy encompassing sequential chemotherapy, radiation therapy and consolidation chemotherapy.
Results
The study analysis comprised 32 endometrial cancer patients. All subjects were treated with carboplatin and paclitaxel chemotherapy; currently, 186 cycles have been administered and 94% of patients have completed the planned number of cycles. Grade 3 neutropenia developed in 1 (3.1%) patient; there was no incidence of grade 4 neutropenia. Moreover, we observed grade 3 anemia in four (12.5%) patients and grade 4 anemia in one (3.1%) patient. One (3.1%) patient developed grade 3 thrombocytopenia; grade 4 thrombocytopenia was not observed. Five patients exhibited progressive disease, three of whom have since expired; mean progression free survival and follow-up were 17.4 months and 18.9 months, respectively.
Conclusion
The preliminary results from our study suggest that the sandwich approach to treating high risk endometrial cancer patients is feasible. Hematologic toxicity was well tolerated and non-hematologic toxicity was mild and easily managed. Further study of this novel regimen in a larger patient population with extended follow-up is necessary.
Endometrial cancer is the most common gynecologic malignancy in the United States, with approximately 42,160 new cases diagnosed in 2009 [1]. The majority of endometrial cancer patients present with early stage disease, which is associated with a favorable prognosis. Nevertheless, recurrence rates are high in advanced stage disease; reported survival rates for patients with stage III or IV endometrial cancer range from 30-89% and 0-10%, respectively [2-4].
Chemotherapy and whole abdominal radiotherapy (WAR) have been actively employed in the treatment of advanced endometrial cancer [5-7]. However, in comparison to WAR, systemic chemotherapy has demonstrated greater efficacy and more favorable patient outcomes [2]. Chemotherapy alone, nonetheless, has been associated with unfavorable pelvic relapse rates and appears inadequate at staving off loco-regional recurrences [2,8]. Alternatively, when combining chemotherapy and irradiation, high risk endometrial cancer patients exhibited superior 3-year progression free (PFS, 62%) and overall survival (OS, 79%) compared to either radiotherapy (PFS, 59% and OS, 70%) or chemotherapy alone (PFS, 19% and OS, 33%) [9].
One consideration in employing chemotherapy and radiotherapy is the appropriate timing of treatment because of the the potential for alleviating patient toxicity. For example, in patients who commence with chemotherapy and develop toxicity, their capacity to complete radiotherapy may be compromised [10]. Conversely, when radiotherapy is initially administered, patients may be more susceptible to cancer progression from residual microscopic disease during the transitional period (i.e., prior to initiating chemotherapy) [9]. Studies have therefore, attempted to evaluate if the particular sequence in which adjuvant therapy is administered can mitigate toxicity and improve patient outcomes [4,9,11-13].
One such approach, the sandwich method, involves adjuvant chemotherapy followed by radiotherapy and subsequent chemotherapy. In modifying the sequence of chemotherapy and irradiation, the hematologic toxicity is theoretically more manageable (i.e., a decreased incidence of dose delays and reductions), facilitating the administration of both treatments [11,12]. In another study involving endometrial cancer patients who were treated with the sandwich approach, the subjects were able to tolerate higher chemotherapy doses and experienced a lower incidence of dose delays. Moreover, they exhibited a 3-year PFS of 69% and an OS of 91% [13].
The sandwich approach potentially confers a more optimal prognostic benefit compared to conventional administration of chemotherapy and radiotherapy. The purpose of the current retrospective study was to evaluate the efficacy and toxicity profile of sequential multi-modality sandwich therapy for the treatment of high risk endometrial carcinoma.
Following IRB approval, we conducted a chart review of 137 newly diagnosed endometrial cancer patients who received adjuvant chemo-radiation therapy from June 2008 until June 2011. From this group, we selected subjects who adhered to the following inclusion criteria: advanced stage or high risk endometrial cancer patients who underwent surgery and adjuvant sequential chemotherapy and radiotherapy followed by 3 additional cycles of chemotherapy.
High risk endometrial cancer criteria included, but were not limited to, high grade (≥2), advanced stage, presence of lymph-vascular space invasion, parametrial involvement, positive pelvic or para-aortic nodes, cervical or vaginal disease and myometrial invasion (outer one-third). Subjects underwent surgical staging comprised of total hysterectomy, bilateral salpingo-oophorectomy, bilateral pelvic and para-aortic lymph node dissection and peritoneal cytology. Pelvic lymph node dissection typically encompassed the removal of lymphatic tissue from the anterior and medial surfaces of the iliac vessels and from the obturator distribution of the aforementioned nerve.
Original pathologic reports were reviewed to determine histologic type, FIGO stage, tumor grade, nodal status and identified sites of metastasis. Histologic diagnosis was confirmed in all cases via pathologic evaluation. Status of surgical cytoreduction was determined per the physician's operative notes. We defined optimal debulking as a maximum 1 cm diameter of residual disease following surgery [14].
Patients primarily commenced their chemotherapy regimen within 2-3 weeks of initial surgical debulking. All study patients were treated with carboplatin (area under the curve [AUC] 5 or 6) and paclitaxel (175 mg/m2) every 21 days for an intended 3 cycles prior to the initiation of radiotherapy. Toxicity was graded using the National Cancer Institute criteria [15].
Radiation therapy dosage and irradiated fields were determined by disease site, lymph node status and the discretion of the treating radiation oncologist. Prior to being irradiated, treatment planning was assessed to define the intended fields corresponding to the vaginal cuff, pelvic and para-aortic nodes, kidneys and small bowel.
Select patients were treated with a total dose of external-beam pelvic radiation of 50.4 Gy to the pelvis over 5 weeks with a daily fraction size of 1.8 Gy. Radiotherapy was administered via 4 field technique employing an 18 MV linear accelerator with custom multi-leaf collimation blocking. Certain patients underwent intensity modulated radiation therapy (IMRT) to further mitigate the damage to healthy tissue. In patients with positive para-aortic nodes, the irradiated fields encompassed both pelvic and para-aortic chains. Conversely, if the para-aortic nodes were negative for metastatic disease, only the pelvic nodes were irradiated. Chemotherapy or radiotherapy related dose delays or modifications were noted.
Date of disease progression and site of recurrence were recorded. Recurrences were identified by histologic, radiologic or cytologic methods. PFS was defined as the period between initial surgical intervention and diagnosis of disease recurrence. OS was defined as the time from initial surgical treatment until death with all causes of death treated equally. If a subject had not progressed or died, PFS was censored at the time of last follow-up. Long-term surveillance for patients occurred via patient evaluation every 3 months for 3 years, semi-annually for 2 years and then annually, thereafter.
All statistical analyses were conducted using MedCalc statistical software for biomedical research (ver. 9.5.1 for Windows; MedCalc Software, Mariakerke, Belgium). Data analysis was initially conducted by employing a descriptive statistical approach and further explored via Kaplan Meier and Cox proportional-hazards regression; significance (<0.05) was determined via 2-sided p-values.
From the original group, we identified 33 subjects who underwent surgical treatment and were either in the process of or completed adjuvant sequential chemotherapy and radiotherapy in accordance with the sandwich approach. One patient was removed from the study during cycle one, electing to transfer her care to another medical facility; the subject's data were excluded from the overall group analysis.
The predominant histologic subtype was endometrioid (n=19; 59.4%). In the present study population, 46.9% had poorly differentiated tumors, while 40.6% and 12.5% had moderately and well differentiated cancers, respectively. The patients' clinical and pathologic characteristics are reported in Table 1.
The total number of chemotherapy cycles administered to the 32 subjects at the conclusion of data collection was 186; 94% of the patients completed the planned number of cycles. One patient withdrew from the study following cycle 3 after she developed a seizure and another was removed following cycle 4 due to grade 2 thrombocytopenia. Nevertheless, all 32 patients were treated with 3 chemotherapy cycles prior to radiation therapy; the median number of chemotherapy cycles subsequent to radiation therapy was 3 (range, 0 to 3).
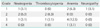
In terms or toxicity, grade 3 neutropenia was observed in 1 (3.1%) patient; none of the subjects developed grade 4 neutropenia. Moreover, four (12.5%) patients developed grade 3 anemia and one (3.1%) patient exhibited grade 4 anemia. One (3.1%) patient exhibited grade 3 thrombocytopenia; we did not observe any grade 4 thrombocytopenia. There was no incidence of grade 3 or 4 neurotoxicity, although 1 (3.1%) patient developed grade 1 neuropathy (Table 2).
The mean total dose of radiation therapy was 4,722.81 +/- 583.82 cGY (95% confidence interval [CI], 4,512.32 to 4,933.30). The total dose prescribed to the pelvic region ranged from 4,000 to 4,600 cGY. The median time from initiation of chemotherapy to commencement of radiotherapy was 39 days (range, 22 to 61 days). The median number of radiation therapy days was 46 days (range, 39 to 55 days). The inclusion of high dose rate (HDR) vaginal vault brachytherapy (700 cGY prescribed to the vaginal surface) was contingent upon the treating physician's discretion. In the group of 32 patients, 7 received vaginal brachytherapy.
During the course of this review, there were only 3 dose delays, neither of which resulted in a dose reduction. Two chemotherapy dose delays were attributed to ≥grade 2 thrombocytopenia or neutropenia. One patient experienced a radiotherapy related dose delay associated with grade 2 colitis. Four patients received granulocyte colony-stimulating factor (G-CSF) to address ≥grade 2 neutropenia; three patients had a blood transfusion.
Thus far, 5 patients have exhibited disease progression. There were two cases of recurrent disease in the vagina (stage II and IIIC2) and one case of progressive disease in the pelvis (stage IA). Moreover, one patient exhibited recurrent extra-pelvic disease (IIIC2) and another subject developed recurrent pulmonary disease (stage IVA). The patients' mean progression free survival was 17.4±6.56 months (95% CI, 15.00 to 19.74) (Fig. 1). While recognizing that a small sample size essentially precludes a sub-group analysis, we consider it noteworthy that 4 of the 5 progressive disease cases coincided with a high risk histology (uterine papillary serous carcinoma [UPSC]-3, clear cell-1); three patients have expired since the initiation of the study and overall survival is currently indeterminate. The patients' mean duration of follow-up was 18.9±7.48 months (95% CI, 16.21 to 21.60).
Chemotherapy and radiation therapy have frequently been employed in the treatment of advanced endometrial cancer [5-7,9]. There are, however, complications associated with administering these two therapies [10-12]. Hence, to address these concerns, novel regimens such as the sandwich approach, have been considered.
In the present sandwich therapy investigation for the treatment of high risk endometrial cancer, we ascertained that one (0.5%) cycle was associated with grade 3 neutropenia, with no observed grade 4 neutropenia. Similarly, only one (0.5%) cycle was associated with grade 3 thrombocytopenia; there was no incidence of grade 4 thrombocytopenia. Grade 3 anemia coincided with 7 (3.77%) cycles and one (0.5%) cycle was associated with grade 4 anemia. Grade 1 neuropathy was encountered with one cycle; non-hematologic toxicity was mild and easily managed. Nevertheless, the retrospective nature of this study limits a comprehensive assessment of toxicity.
Lupe et al. [12] employed 4 cycles of adjuvant chemotherapy, followed by radiotherapy and 2 additional cycles of chemotherapy for the treatment of advanced stage endometrial cancer. They reported that the overall chemotherapy toxicity profile was acceptable; greater than 91% of chemotherapy cycles prior to radiotherapy were administered, but only 76% of the subsequent chemotherapy cycles were completed due to grade 3/4 hematologic toxicity.
Fields et al. [11] studied the impact of sandwich therapy (paclitaxel and platinum chemotherapy, followed by pelvic radiotherapy and 3 additional cycles of chemotherapy) in optimally resected and staged UPSC patients. They encountered acceptable toxicity although grades 3 or 4 neutropenia were associated with 42% of the cycles.
In our study, we reported an 84% PFS rate, which is higher than the 69% described by Secord et al. [9] and approximately 55% in both the Fields et al. [11] and Lupe et al. [12] studies. One may conjecture that these PFS differences are attributed to diverse patient populations (e.g., variations in disease stage), different treatment regimens and duration of follow-up. For example, Geller et al. [10] primarily (91% of patients) employed carboplatin and paclitaxel in their sequential multi-modality therapy study for the treatment of high risk endometrial cancer; their reported 80.4% PFS was similar to our results. In a later study, Geller et al. [16] reported an 87% PFS following sandwich therapy with carboplatin and docetaxel, although their patient population was comprised of both advanced and recurrent endometrial cancer patients.
High risk endometrial cancer patients are vulnerable to local and distal recurrences, and thus, sandwich therapy may provide a therapeutic benefit; chemotherapy can assist with staving off upper abdominal disease following surgical staging and post radiotherapy potentially mitigates the risk for local recurrences [9,13]. In the current investigation, five patients developed recurrent cancer and the overall PFS was greater than 17 months; three patients exhibited progressive disease distally (e.g., pulmonary, pelvis or extra-pelvic) whereas two developed a vaginal recurrence. The majority (80%) of our progressive disease cases encompassed UPSC and clear cell tumors; this is consistent with previous studies that have categorized these tumor histologies as high risk [10,17] although one could speculate that our results are attributed to a stage phenomenon or a combination of these two factors.
In high risk endometrial cancer patients, the most frequent site of recurrence is the vagina [18]. Therefore, the inclusion of vaginal brachytherapy (VBT) for endometrial cancer patients with positive pelvic or para-aortic nodes, cervical or vaginal disease and parametrial involvement may be indicated [18-21]. We employed VBT in less than 25% of patients, although the treatment potentially engenders a significant therapeutic benefit. For example, in the PORTEC-2 trial, high-intermediate risk endometrial carcinoma patients were randomized to either external beam radiotherapy (46 Gy) or to VBT (30 Gy); estimated 5-year vaginal recurrent rates were similar (1.8% for VBT and 1.6% for external beam radiotherapy [EBRT]) but loco-regional relapse rates were more favorable in the VBT patients (2.1% vs. 5.1%) [18].
The data presented in this current analysis provide support for the hypothesis that sequential chemotherapy and radiotherapy in accordance with moreover the sandwich approach may ultimately improve high risk endometrial cancer patient outcomes. The sandwich approach appeared to demonstrate reasonable activity and was well tolerated (i.e., there was a reasonably low incidence of dose delays or reductions).
The current study has several limitations; in particular, an appreciation of overall toxicity may be confounded in a retrospective evaluation. Our definition of high risk endometrial cancer could be considered variable (i.e., low to high risk biologic behavior), which may explain the favorable outcomes in comparison to previous studies. Moreover, patient follow-up was not extensive (18.9 months) and reporting bias is always a concern with investigational evaluations. We also recognize that the patients' beneficial outcomes may reflect the preponderance of subjects with low to moderate grade or stage of disease; several of the study patients had endometrioid histology, in contrast to reported series [9,12].
The type of radiotherapy was also not delineated (i.e., we did not discern if there were prognostic differences amongst the patients who received pelvic radiotherapy (with or without extended fields), vaginal brachytherapy alone or with pelvic radiotherapy, and IMRT). In particular, the use of IMRT may have accounted for the reasonable toxicity encountered in the present study. Additional investigation of this novel regimen with a larger population of high risk endometrial cancer patients, even if only compared to a well-characterized control population, would strengthen the conclusions associated with the present analysis.
Figures and Tables
Fig. 1
Progression-free survival for high-risk endometrial cancer patients treated with sequential multimodal therapy.

References
1. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009. 59:225–249.
2. Randall ME, Filiaci VL, Muss H, Spirtos NM, Mannel RS, Fowler J, et al. Randomized phase III trial of whole-abdominal irradiation versus doxorubicin and cisplatin chemotherapy in advanced endometrial carcinoma: a Gynecologic Oncology Group Study. J Clin Oncol. 2006. 24:36–44.
3. Smith RS, Kapp DS, Chen Q, Teng NN. Treatment of high-risk uterine cancer with whole abdominopelvic radiation therapy. Int J Radiat Oncol Biol Phys. 2000. 48:767–778.
4. Onda T, Yoshikawa H, Mizutani K, Mishima M, Yokota H, Nagano H, et al. Treatment of node-positive endometrial cancer with complete node dissection, chemotherapy and radiation therapy. Br J Cancer. 1997. 75:1836–1841.
5. Thigpen JT, Brady MF, Homesley HD, Malfetano J, DuBeshter B, Burger RA, et al. Phase III trial of doxorubicin with or without cisplatin in advanced endometrial carcinoma: a gynecologic oncology group study. J Clin Oncol. 2004. 22:3902–3908.
6. Sutton G, Axelrod JH, Bundy BN, Roy T, Homesley HD, Malfetano JH, et al. Whole abdominal radiotherapy in the adjuvant treatment of patients with stage III and IV endometrial cancer: a gynecologic oncology group study. Gynecol Oncol. 2005. 97:755–763.
7. Fleming GF, Brunetto VL, Cella D, Look KY, Reid GC, Munkarah AR, et al. Phase III trial of doxorubicin plus cisplatin with or without paclitaxel plus filgrastim in advanced endometrial carcinoma: a Gynecologic Oncology Group Study. J Clin Oncol. 2004. 22:2159–2166.
8. Aoki Y, Kase H, Watanabe M, Sato T, Kurata H, Tanaka K. Stage III endometrial cancer: analysis of prognostic factors and failure patterns after adjuvant chemotherapy. Gynecol Oncol. 2001. 83:1–5.
9. Secord AA, Havrilesky LJ, O'Malley DM, Bae-Jump V, Fleming ND, Broadwater G, et al. A multicenter evaluation of sequential multimodality therapy and clinical outcome for the treatment of advanced endometrial cancer. Gynecol Oncol. 2009. 114:442–447.
10. Geller MA, Ivy J, Dusenbery KE, Ghebre R, Isaksson Vogel R, Argenta PA. A single institution experience using sequential multi-modality adjuvant chemotherapy and radiation in the sandwich method for high risk endometrial carcinoma. Gynecol Oncol. 2010. 118:19–23.
11. Fields AL, Einstein MH, Novetsky AP, Gebb J, Goldberg GL. Pilot phase II trial of radiation "sandwiched" between combination paclitaxel/platinum chemotherapy in patients with uterine papillary serous carcinoma (UPSC). Gynecol Oncol. 2008. 108:201–206.
12. Lupe K, Kwon J, D'Souza D, Gawlik C, Stitt L, Whiston F, et al. Adjuvant paclitaxel and carboplatin chemotherapy with involved field radiation in advanced endometrial cancer: a sequential approach. Int J Radiat Oncol Biol Phys. 2007. 67:110–116.
13. Alvarez Secord A, Havrilesky LJ, Bae-Jump V, Chin J, Calingaert B, Bland A, et al. The role of multi-modality adjuvant chemotherapy and radiation in women with advanced stage endometrial cancer. Gynecol Oncol. 2007. 107:285–291.
14. Patsavas K, Woessner J, Gielda B, Rotmensch J, Yordan E, Bitterman P, et al. Optimal surgical debulking in uterine papillary serous carcinoma affects survival. Gynecol Oncol. 2011. 121:581–585.
15. National Institute of Health. NIH common terminology criteria for adverse events (CTCAE) v3.0. 2003. Washington: National Institute of Health.
16. Geller MA, Ivy JJ, Ghebre R, Downs LS Jr, Judson PL, Carson LF, et al. A phase II trial of carboplatin and docetaxel followed by radiotherapy given in a sandwich method for stage III, IV, and recurrent endometrial cancer. Gynecol Oncol. 2011. 121:112–117.
17. O'Hanlan KA, Levine PA, Harbatkin D, Feiner C, Goldberg GL, Jones JG, et al. Virulence of papillary endometrial carcinoma. Gynecol Oncol. 1990. 37:112–119.
18. Nout RA, Smit VT, Putter H, Jürgenliemk-Schulz IM, Jobsen JJ, Lutgens LC, et al. Vaginal brachytherapy versus pelvic external beam radiotherapy for patients with endometrial cancer of high-intermediate risk (PORTEC-2): an open-label, non-inferiority, randomized trial. Lancet. 2010. 375:816–823.
19. Diavolitsis V, Boyle J, Singh DK, Small W Jr. The role of adjuvant radiation in endometrial cancer. Oncology (Williston Park). 2009. 23:342–349.
20. Dickler A, Puthawala MY, Thropay JP, Bhatnagar A, Schreiber G. Prospective multi-center trial utilizing electronic brachytherapy for the treatment of endometrial cancer. Radiat Oncol. 2010. 5:67.
21. McCloskey SA, Tchabo NE, Malhotra HK, Odunsi K, Rodabaugh K, Singhal P, et al. Adjuvant vaginal brachytherapy alone for high risk localized endometrial cancer as defined by the three major randomized trials of adjuvant pelvic radiation. Gynecol Oncol. 2010. 116:404–407.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download