Abstract
Objective
To determine the predictive accuracy of the combined panels of serum human tissue kallikreins (hKs) and CA-125 for the detection of epithelial ovarian cancer.
Methods
Serum specimens collected from 5 Indonesian centers and 1 Vietnamese center were analyzed for CA-125, hK6, and hK10 levels. A total of 375 specimens from patients presenting with ovarian tumors, which include 156 benign cysts, 172 epithelial ovarian cancers (stage I/II, n=72; stage III/IV, n=100), 36 germ cell tumors and 11 borderline tumors, were included in the study analysis. Receiver operating characteristic analysis were performed to determine the cutoffs for age, CA-125, hK6, and hK10. Sensitivity, specificity, negative, and positive predictive values were determined for various combinations of the biomarkers.
Results
The levels of hK6 and hK10 were significantly elevated in ovarian cancer cases compared to benign cysts. Combination of 3 markers, age/CA-125/hk6 or CA-125/hk6/hk10, showed improved specificity (100%) and positive predictive value (100%) for prediction of ovarian cancer, when compared to the performance of single markers having 80-92% specificity and 74-87% positive predictive value. Four-marker combination, age/CA-125/hK6/hK10 also showed 100% specificity and 100% positive predictive value, although it demonstrated low sensitivity (11.9%) and negative predictive value (52.8%).
Ovarian cancer is one of the most severe gynecological malignancies known and is the fourth leading cause of cancer-related deaths in the United States [1], and has become the most lethal of all gynecological malignancies in Singapore women. Early stage disease has excellent prognosis but late stage disease has contributed to the high mortality rate of between 80% and 90% compared to early stage disease of between 10% and 30% [2]. Similar trends have been seen in Singapore women showing mortality of advanced stage at 77.1% and 20% in the early stage disease over a 5-year period [3]. The overall 5-year survival rate has not changed over the past thirty years despite the availability of new cytotoxic treatments [4] which showed dismal outcome, especially in advanced stage disease. Early detection remains the most important approach to improve long-term survival for ovarian cancer. Currently, CA-125 discovered nearly 30 years ago [5] remained the well-accepted serum biomarker for ovarian cancer but is neither specific nor sensitive enough for diagnosis [6-8]. It has clinical value for disease monitoring and has been used as an aid for early detection of relapse and for evaluation of response to treatment [9-11]. Prognostic indicators or biomarkers improve the accuracy of predicting patient outcomes, and until reliable screening or diagnostic strategies become available, they may contribute to the optimal tailored individual management of patients with ovarian cancer.
The current trend to focus on combined multiparametric analysis of different biomarkers to improve clinical outcomes and diagnosis will offer several advantages [12-15]. The group of serine proteases known as human tissue kallikreins (hK) has a rich source of cancer biomarkers and suited for multiparametric analysis. Human tissue kallikreins (KLK for gene, hK for protein) is a family of 15 members encoded by a group of genes tandemly localized on chromosome 19q13.3-4 [16]. It is highly expressed in sex organs such as the breast, ovary, prostate and testis. Emerging diagnostic markers notably hK6, hK10, and hK11 are highly expressed in the majority of ovarian cancer cases and especially in the advanced stage diseases [17-20]. The conventional CA-125 marker has shown negative values in 40% to 50% of early stage ovarian cancer and upregulated in benign tumors and other cancers [8,21]. However, tissue kallikrein proteins hK6 and hK10 together with osteopontin levels have been reported to be promising potential markers that might complement CA-125 in ovarian cancer [22]. It was suggested that the expression of hK6 may be an early event during ovarian cancer development and have potential use as biomarker for early detection of ovarian cancer [23] and prediction of progression-free survival [24]. In a small ovarian cancer cohort study, elevated levels of CA-125, hK6 and hK10 were seen. However, elevated serum hK6 levels was associated with mortality outcome within 12 months of diagnosis compared to those who survived over five years from epithelial ovarian cancer [3].
The objective of this collaborative study in South-East Asia from five Indonesian centers and one Vietnamese center in Ho Chi Minh City was to determine the value of ovarian cancer biomarkers hK6/hK10 and their association with CA-125 levels and age in patients with ovarian tumors for the prediction of epithelial ovarian cancer.
The study received approval from the National University of Singapore Institutional Review Board (NUS-IRB reference codes 05-025 and 06-067) and the respective ethics committee of various institutions involved in the study. Inclusion criteria were women with a pelvic mass detected by ultrasound at the hospital clinic and scheduled for operation. This was a prospective study and patients diagnosed with ovarian tumors were recruited to the study. Informed Consent was sought before they were allowed to take part in the study. Recruitment of subjects began in May 2005 in Medan, Indonesia and thereafter in various Indonesian centers; Denpasar (February 2006), Palembang (October 2006), Yogyakarta (December 2006), Jakarta (September 2007), and Ho Chi Minh City, Vietnam (April 2008) until August 2010. A total of 375 samples with confirmed patient information data were received; benign cysts 156, epithelial ovarian cancer 172 (stage I/II, n=72; stage III/IV n=100), germ cell cancer 36 and borderline 11. Administration of chemotherapy consisting of either cyclophosphamide, taxol and platinum drugs was recorded only for 26.2% (45/172) epithelial ovarian cancer patients. Most of the cancer patients were lost to follow-up and survival outcome analysis was not possible as most of them returned to their hometown soon after their diagnosis and surgery or after chemotherapy and did not returned for follow-up visits. Benign cyst cohorts were significantly younger with mean age of 38.3±1.2 years (95% CI, 35.9 to 40.8) compared to ovarian cancer patients with mean age of 45.5±1.0 years (95% CI, 43.5 to 47.5).
Blood sampling was performed in the morning before the scheduled operation. A clean venepuncture was performed together for hemostatic analysis, about 5 mL of plain blood was transferred in to clean plastic tubes. The blood tubes were then left at room temperature to clot for about 2 hours before they are centrifuged at 2,000 g for 15 minutes. The available sera was stored in aliquots and immediately kept at either -40℃ or -70℃ until dispatched to Singapore for storage at -80℃ and analysis.
CA-125 assay was performed by IMMULITE 1000 systems (Siemens, Los Angeles, CA, USA). Elisa assay for serum hK6 and hK10 was performed at the Pathology & Laboratory Medicine, Mount Sinai Hospital, Toronto, Canada, after consultation. It is a two-step sandwich immunoassay described earlier by Diamandis et al. [25].
All statistical analysis was performed using SPSS ver. 18.0 (SPSS Inc., Chicago, DE, USA). Group means were tested and compared by t-test. A p-value of less than 0.05 was considered statistically significant. Receiver operating characteristics (ROC) analysis were performed to determine the optimal cutoffs for age, CA-125, hK6 and hK10 levels. The sensitivity, specificity, positive predictive value (ppv) and negative predictive value (npv) for single and combination of markers were determined for the detection of ovarian cancer, early and advanced stage of disease.
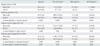
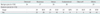
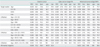
The types of benign cysts and epithelial ovarian cancer in the cohorts studied are shown in Table 1. The comparison of mean values of age, CA-125, hK6, and hK10 between benign cysts and epithelial ovarian cancer are shown in Table 2. Benign cyst cohorts from the Vietnamese center (n=44) and the Indonesian centers (n=112) showed no significant differences in the parameters studied. Hence, they were grouped together in the final analysis. Ovarian cancer cohorts were significantly older with a mean age of 45.5 years compared to 38.3 years in benign cyst cohorts and showed significant upregulation (p<0.001) of CA-125, hK6, and hK10 levels compared to benign cyst cohorts. In early stage ovarian cancer cases, significantly elevated levels of CA-125 (p=0.04), hK6 (p=0.03) in addition to older age (p=0.005) were observed compared to benign cyst cohorts. In addition, significant upregulation of CA-125 (p<0.001), hK6 (p=0.001), and hK10 (p=0.001) levels together with older age (p=0.002) were also seen in advanced stage diseases compared to benign cyst cohorts. When comparing early and advanced stage diseases, CA-125 (p=0.03) and hK6 (p=0.04) were significantly elevated in advanced stage disease with no significant differences in hK10 level and age. The variable scatter plots for the markers studied in benign cyst, early and advanced stage cancer are shown in Fig. 1. No significant differences in age, hK6 and hK10 levels between germ cell cancer (n=36) and benign cyst cohorts except CA-125 level which was significantly elevated (p=0.04) with mean value of 377.3±224.2 IU/mL (data not shown). The highest hK6 and hK10 levels were expressed by mucinous cancer (mean, 10.0±2.6 ng/mL and 3.3±1.2 ng/mL respectively), whilst in benign cyst cohorts, the endometroid type showed relatively elevated levels of hK6 (mean, 4.6±0.6 ng/mL) with hK10 mean levels of between 1.0 to 1.2 ng/mL seen for different benign types including endometroid cysts. Optimal cutoffs determined by ROC analysis for age, CA-125, hK6, and hK10 were 42 years, 93.0 IU/mL, 6.0 ng/mL, and 1.4 ng/mL, respectively and they were all above the mean levels of benign cyst cohorts (Table 2). The combination of either hK6 or hK10 with CA-125 showed potential as ovarian cancer prediction. The 3-combined markers of either age/CA-125/hK6 or CA-125/hK6/hK10 had 100% specificity and ppv with npv 54.1%/55.6% and sensitivity 18.8%/19.2% respectively for ovarian cancer prediction. The 4-combined markers age/CA-125/hK6/hK10 also showed 100% specificity and ppv with sensitivity 11.9%. When all 4 combined markers are negative, no advanced cancer is predicted with 100% specificity and ppv. The predictive values of various combinations of epithelial ovarian cancer markers are shown in Table 3.
Promising predictive tumor markers have been evaluated in patients with ovarian cancer. These combinations of markers showed promise to improve sensitivity and specificity, and in one study of four-marker panel which included CA-125, apolipoprotein A-1, transthyretin and transferrin, it was reported to improve sensitivity (96%), specificity (98%) for early stage ovarian cancer but has yet to be validated in clinical trials [26]. An earlier study using four-analyte test (leptin, prolactin, osteopontin, and insulin-like growth factor II) exhibited sensitivity 95%, ppv 95%, and npv 94% [27]. Proteases have emerged as important prognosticators in ovarian cancer [28] and the human tissue kallikrein family showed promise as biomarkers for ovarian cancer diagnosis, prognosis and monitoring [17,18,20]. Elevated serum or tissue levels of hKs have been individually implicated as diagnostic and prognostic factors in ovarian cancer [18,29 32]. In advanced stage disease, serous histological type and large residual tumor are known indicators for aggressiveness and poor outcome in ovarian cancer [30]. Proteases are widely believed to be involved in carcinogenesis and the concentration of proteases released by the primary tumor may reflect the ability of a tumor to spread [33,34]. Combined serum hK6 and hK10 can increase the diagnostic sensitivity of CA-125 in patients with early stage (I/II) ovarian cancer [29]. In the current study, the combination of hK6 and/or hK10 with CA-125 improved the specificity and ppv for the detection of ovarian cancer, despite the lower sensitivity.
In this study from South-East Asia, the ovarian cancer cohorts was significantly older with upregulated levels of CA-125, hK6, and hK10 than those observed in benign cyst cohorts. Early stage cancer showed older cohorts with significant upregulation of CA-125 and hK6 levels when compared with benign cyst cohorts. Only CA-125 and hK6 levels were further raised in advanced stage disease compared to early stage. The ovarian cancer cohorts from this study were younger (mean, 45.5 years) than reported for the incidence in postmenopausal women in the United States (mean, 60 years) and Scandinavia (mean, 61 years) [35,36]. Expression of the highest levels of hK6/hK10 in ovarian cancer were seen in mucinous cancer, contrary to the serous type reported [32]. In benign tumors, endometroid type expresses the highest hK6 levels whilst hK10 was not appreciable. In germ cell tumors, neither hK6 nor hK10 were upregulated except for raised CA-125 levels.
The proposed combination of biomarkers, including hK6, hK10, CA-125, and age, which cutoffs were determined by ROC analysis showed potential in improving the prediction of epithelial ovarian cancer in patients presenting with ovarian tumors. We analyzed various combination of the 4 markers for their ability to predict ovarian cancer, in early and late stage disease. Using this approach, the combination of 3 markers including age/CA-125/hK6 and hk6/hK10/CA-125 showed 100% specificity and ppv despite lower sensitivity, similar to the 4-marker combination of age/CA-125/hK6/hK10. No advanced cancer is predicted if the 4 combined markers are negative. The template proposed for predicting ovarian cancer may not meet the WHO criteria for screening tests which defines that high sensitivity and specificity are required during development of screening tests to detect early stage disease [37]. Screening tests must achieve at least 75% sensitivity and specificity of greater than 99.6% to achieve a positive predictive value of 10% for the detection of all stages of ovarian cancer [38]. Moreover, there may be limitations to this approach as full ultrasonography details are lacking but further study with the inclusion of ultrasonography can better enhance the potential value of these markers.
The analysis of combined markers may be a better choice than the use of CA-125 alone to predict ovarian cancer. Whilst the markers may be combined with CA-125 in improving the overall specificity of ovarian cancer detection, further investigation is needed to refine and evaluate the marker panels as a screening and detection modality [39]. The combination of multiple biomarkers and early screening modalities may be the key to obtain the most accurate forms of ovarian cancer detection. It is also important to identify screening techniques with low false positive rates and high positive predictive value so that negative surgical interventions can be minimized [39].
In conclusion, ovarian cancer cohorts from the region were older with upregulated levels of CA-125, hK6, and hK10. The combination of hK6 and hK10 with CA-125 and age demonstrated the potential for improved prediction of epithelial ovarian cancer, early and late stage disease in patients presenting with ovarian tumor.
Figures and Tables
Fig. 1
Scatter plots with mean levels indicated comparing the variable distribution of age, CA-125, human tissue kallikrein 6 (hK6), hK10 between benign cyst and ovarian cancer stage I/II and stage III/IV.

Table 2
Descriptive statistics and group mean test for age, CA-125, human tissue kallikrein 6 (hK6), and hK10 in benign cyst and epithelial ovarian cancer (early and advanced stage disease)
ACKNOWLEDGMENTS
The study was made possible through the financial support from the Lee Foundation. The collaboration study involving Indonesian centers was initiated through Professor Djaffar Siddik, former Head of the University Department of Obstetrics and Gynaecology, Adam Malik Hospital, Medan, Sumatra, Indonesia and the author with assistance from Professor Herman Hariman of the University of North Sumatera Faculty of Medicine. The expert technical assistance from Chua SE, Yuen WK and Ng BL is gratefully acknowledged.
References
1. Jemal A, Tiwari RC, Murray T, Ghafoor A, Samuels A, Ward E, et al. Cancer statistics, 2004. CA Cancer J Clin. 2004. 54:8–29.
2. Schink JC. Current initial therapy of stage III and IV ovarian cancer: challenges for managed care. Semin Oncol. 1999. 26:2–7.
3. Koh SC, Razvi K, Chan YH, Narasimhan K, Ilancheran A, Low JJ, et al. The association with age, human tissue kallikreins 6 and 10 and hemostatic markers for survival outcome from epithelial ovarian cancer. Arch Gynecol Obstet. 2011. 284:183–190.
4. Cannistra SA. Cancer of the ovary. N Engl J Med. 2004. 351:2519–2529.
5. Bast RC Jr, Feeney M, Lazarus H, Nadler LM, Colvin RB, Knapp RC. Reactivity of a monoclonal antibody with human ovarian carcinoma. J Clin Invest. 1981. 68:1331–1337.
6. Rosenthal AN, Jacobs IJ. The role of CA 125 in screening for ovarian cancer. Int J Biol Markers. 1998. 13:216–220.
7. Maggino T, Gadducci A. Serum markers as prognostic factors in epithelial ovarian cancer: an overview. Eur J Gynaecol Oncol. 2000. 21:64–69.
8. Bast RC Jr, Xu FJ, Yu YH, Barnhill S, Zhang Z, Mills GB. CA 125: the past and the future. Int J Biol Markers. 1998. 13:179–187.
9. Rustin GJ, Nelstrop A, Stilwell J, Lambert HE. Savings obtained by CA-125 measurements during therapy for ovarian carcinoma: the North Thames Ovary Group. Eur J Cancer. 1992. 28:79–82.
10. Rustin GJ, Nelstrop AE, McClean P, Brady MF, McGuire WP, Hoskins WJ, et al. Defining response of ovarian carcinoma to initial chemotherapy according to serum CA 125. J Clin Oncol. 1996. 14:1545–1551.
11. Eisenhauer EA, Vermorken JB, van Glabbeke M. Predictors of response to subsequent chemotherapy in platinum pretreated ovarian cancer: a multivariate analysis of 704 patients. Ann Oncol. 1997. 8:963–968.
12. Spentzos D, Levine DA, Ramoni MF, Joseph M, Gu X, Boyd J, et al. Gene expression signature with independent prognostic significance in epithelial ovarian cancer. J Clin Oncol. 2004. 22:4700–4710.
13. Kaern J, Aghmesheh M, Nesland JM, Danielsen HE, Sandstad B, Friedlander M, et al. Prognostic factors in ovarian carcinoma stage III patients: can biomarkers improve the prediction of short- and long-term survivors? Int J Gynecol Cancer. 2005. 15:1014–1022.
14. Bast RC Jr, Badgwell D, Lu Z, Marquez R, Rosen D, Liu J, et al. New tumor markers: CA125 and beyond. Int J Gynecol Cancer. 2005. 15:Suppl 3. 274–281.
15. Badgwell D, Bast RC Jr. Early detection of ovarian cancer. Dis Markers. 2007. 23:397–410.
16. Yousef GM, Diamandis EP. The new human tissue kallikrein gene family: structure, function, and association to disease. Endocr Rev. 2001. 22:184–204.
17. Diamandis EP, Yousef GM. Human tissue kallikreins: a family of new cancer biomarkers. Clin Chem. 2002. 48:1198–1205.
18. Diamandis EP, Okui A, Mitsui S, Luo LY, Soosaipillai A, Grass L, et al. Human kallikrein 11: a new biomarker of prostate and ovarian carcinoma. Cancer Res. 2002. 62:295–300.
19. Diamandis EP, Scorilas A, Fracchioli S, Van Gramberen M, De Bruijn H, Henrik A, et al. Human kallikrein 6 (hK6): a new potential serum biomarker for diagnosis and prognosis of ovarian carcinoma. J Clin Oncol. 2003. 21:1035–1043.
20. Obiezu CV, Diamandis EP. Human tissue kallikrein gene family: applications in cancer. Cancer Lett. 2005. 224:1–22.
21. Mills GB, Bast RC Jr, Srivastava S. Future for ovarian cancer screening: novel markers from emerging technologies of transcriptional profiling and proteomics. J Natl Cancer Inst. 2001. 93:1437–1439.
22. Rosen DG, Wang L, Atkinson JN, Yu Y, Lu KH, Diamandis EP, et al. Potential markers that complement expression of CA125 in epithelial ovarian cancer. Gynecol Oncol. 2005. 99:267–277.
23. Ni X, Zhang W, Huang KC, Wang Y, Ng SK, Mok SC, et al. Characterisation of human kallikrein 6/protease M expression in ovarian cancer. Br J Cancer. 2004. 91:725–731.
24. Zheng Y, Katsaros D, Shan SJ, de la Longrais IR, Porpiglia M, Scorilas A, et al. A multiparametric panel for ovarian cancer diagnosis, prognosis, and response to chemotherapy. Clin Cancer Res. 2007. 13:6984–6992.
25. Diamandis EP, Yousef GM, Soosaipillai AR, Grass L, Porter A, Little S, et al. Immunofluorometric assay of human kallikrein 6 (zyme/protease M/neurosin) and preliminary clinical applications. Clin Biochem. 2000. 33:369–375.
26. Nosov V, Su F, Amneus M, Birrer M, Robins T, Kotlerman J, et al. Validation of serum biomarkers for detection of early-stage ovarian cancer. Am J Obstet Gynecol. 2009. 200:639.e1–639.e5.
27. Mor G, Visintin I, Lai Y, Zhao H, Schwartz P, Rutherford T, et al. Serum protein markers for early detection of ovarian cancer. Proc Natl Acad Sci U S A. 2005. 102:7677–7682.
28. Duffy MJ. Proteases as prognostic markers in cancer. Clin Cancer Res. 1996. 2:613–618.
29. Borgono CA, Diamandis EP. The emerging roles of human tissue kallikreins in cancer. Nat Rev Cancer. 2004. 4:876–890.
30. Diamandis EP, Yousef GM, Soosaipillai AR, Bunting P. Human kallikrein 6 (zyme/protease M/neurosin): a new serum biomarker of ovarian carcinoma. Clin Biochem. 2000. 33:579–583.
31. Dorn J, Schmitt M, Kates R, Schmalfeldt B, Kiechle M, Scorilas A, et al. Primary tumor levels of human tissue kallikreins affect surgical success and survival in ovarian cancer patients. Clin Cancer Res. 2007. 13:1742–1748.
32. Trope C. Prognostic factors in ovarian cancer. Cancer Treat Res. 1998. 95:287–352.
33. Aznavoorian S, Murphy AN, Stetler-Stevenson WG, Liotta LA. Molecular aspects of tumor cell invasion and metastasis. Cancer. 1993. 71:1368–1383.
34. Duffy MJ. The role of proteolytic enzymes in cancer invasion and metastasis. Clin Exp Metastasis. 1992. 10:145–155.
35. Kramer BS, Gohagan J, Prorok PC, Smart C. A National Cancer Institute sponsored screening trial for prostatic, lung, colorectal, and ovarian cancers. Cancer. 1993. 71:589–593.
36. Bjorge T, Engeland A, Sundfor K, Trope CG. Prognosis of 2,800 patients with epithelial ovarian cancer diagnosed during 1975-94 and treated at the Norwegian Radium Hospital. Acta Obstet Gynecol Scand. 1998. 77:777–781.
37. Wilson JM, Jungner G. Principles and practice of screening for disease. 1968. Geneva: World Health Organization.
38. Chu CS, Rubin SC. Screening for ovarian cancer in the general population. Best Pract Res Clin Obstet Gynaecol. 2006. 20:307–320.
39. Rein BJ, Gupta S, Dada R, Safi J, Michener C, Agarwal A. Potential markers for detection and monitoring of ovarian cancer. J Oncol. 2011. 2011:475983.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download