Abstract
Objective
To determine the baseline information about the knowledge of cervical cancer and explore attitude and practice of Pap smear screening among staff nurses.
Methods
A pretested structured self administered questionnaire based survey was done on 205 staff nurses working in Rural Institute of Medical Sciences & Research, Saifai, Etawah, containing mostly recognition and some recall type questions about demographics, knowledge about cervical cancer, its risk factors, screening techniques, attitudes towards cervical cancer screening and its practices.
Results
In this study, 74% knew that Pap smear is used for detection of cervical cancer, but only 59% knew that it can detect both cancerous as well as precancerous lesions of the cervix. Only 18% of the respondents knew about human papillomavirus vaccine. A 47% of respondents had never taken a Pap smear; 63% never referred patients for the screening. Most nurses (79%) thought that a speculum examination and Pap smear are procedures to be performed by the doctors. Among all the respondents, only 11% had ever undergone a Pap smear on themselves.
Globally, cervical cancer is one of the most common cancers in women, with an estimate of 468,000 new cases annually, and 80% of these cases occurring in developing and undeveloped countries [1]. India accounts for one-fifth of the world burden of cervical cancer [2]. In many of the developed countries the annual incidence and mortality from this cancer has gone down by 50-70% since the introduction of population based screening [3]. But it is still a major killer among developing countries, especially in rural settings due to absence of a nationally organized screening program, and also as a result of infrastructural, financial and personnel constraints. In developing countries like ours, more than three-fourths of cervical cancer patients are diagnosed at advanced stages leading to poor prospects of long-term survival and cure [4]. As the doctor to patient ratio is low in India i.e., 1:2,000 according to Medical Council of India (Press Information Bureau, Government of India, Ministry of Health and Family Welfare, 29 November 2011), staff nurses if trained properly, can make aware and screen all the women coming / admitting to hospital for any of their problems, along with motivating the peripheral health workers to bring all the sexually active females to the hospital for the cervical screening. KAP (knowledge, attitude and practice) study will bring forth the weak points among nurses, so that a comprehensive practical training for staff nurses can be organized. In India it is estimated that there were 112,609 new cervical cancers in the year 2004 and this number is expected to rise to 139,864 in 2015 [5]. Therefore awareness among nurses is a basic requirement to implement a successful screening program and actually reduces the incidence of cervical cancer in developing countries like India.
In India, despite the public health importance that cervical cancer merits, there are only sporadic efforts in hospitals and research settings to minimize the mortality from the cancer. The present study was undertaken with the following objectives: 1) to determine the baseline information of the knowledge on risk factors of cervical cancer as well as awareness of the related symptoms and 2) to explore the attitudes and practices among nurses in terms of cervical cancer screening programs such as Pap smear with a view to sensitize them as a first step towards increasing screening uptake in the community.
This descriptive cross-sectional study was conducted in Uttar Pradesh Rural Institute of Medical Sciences & Researches, Saifai, Etawah, which is a referral tertiary care hospital and teaching institute, on 190 female staff nurse over the period of two months from 1st September to 31st October 2010. Working since 2005 it is the largest and busiest government hospital in western Uttar Pradesh. Among 190 nurses, 171 (90%) accepted to participate in the study. A total of 160 questionnaires were retrieved giving a 93.5% return rate, out of which 27 were incomplete and were excluded, leaving the number to 133 only for the study analysis. Thus the final sample size was limited to 133 only (Fig. 1). The self-administered structured questionnaire was developed in collaboration with the gynecological and community medicine department to cover most of the aspects related to cervical cancer and its screening, containing some recall and mostly recognition questions. Recall questions were about demographics, the knowledge of risk factors, sign and symptoms of cervical cancer, diagnosing modalities other than Pap smear and vaccine for human papilloma virus (HPV), whereas rest questions (as on knowledge of eligibility for screening and its interval, practices and attitudes about cervical cancer screening) were of the recognition type. Recognition questions tried to have all relevant alternatives with one or multiple correct answers. Extra space provided at the end of some recognition questions as 'other comments'. Questions tried to be short, clear, readable and understandable to the staff nurses with only few medical terminologies. The questionnaire was pretested initially on a small group of randomly selected staff nurses and subsequent modifications were made before the final study was undertaken. These data were not included in the final analysis of the study.
We elicited knowledge about eligibility for screening and screening interval according to American Congress of Obstetricians and Gynecologists (ACOG) guidelines [6]. Practices were evaluated as screening patients for cervical cancer, referring patients for screening and having ever been screened themselves. Attitudes referred to the various reasons for not screening patients, not referring patients for screening, and not getting screened themselves. After verbal consent, the questionnaire was provided and participants were asked to fill it individually without discussing with others. The study protocol was approved by the institutional ethical committee. The data was entered into MS Excel software. Proportion and chi-square was applied for the analysis and interpretation of the result using 95% confidence interval.
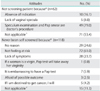
Mean age of respondents was 27.82±3.85 years. A 62% of participants were married, and 70% were not using any contraceptive method (Table 1). Of all respondents, 127 (96%) had heard about the Pap smear but 22% were unaware that it is used for detection of cervical cancer. Only 59% knew that it could detect both cancerous and precancerous lesions of the cervix. More than three quarters, 76% of them knew that if cervical changes were found early then they were easily curable. Only 20% knew more than 3 risk factors, whereas more than half respondents (54%) knew that HPV infection is one of the risk factors of cervical cancer. According to 54% respondents, women above 21 years of age or those who are sexually active for last 3 years (whichever is earlier) were eligible candidates for Pap smear. A 31% of respondents thought Pap screening should only be done in the presence of symptoms. A 90% of respondents knew about the cervical biopsy, although only 7% respondents knew about visual inspection after acetic acid application (VIA), and 20% knew about colposcopy as diagnostic modalities of cervical cancer screening other than Pap smear. Only 18% of the respondents knew about the HPV vaccine. Only 21% respondents gained information about Pap smear while working in this institute (Table 2).
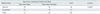
A 74% of the study participants routinely managed female patients, and 53% had frequently performed vaginal examinations, although the use of speculum was surprisingly low (21%). A large number of respondents (47%) had never taken a Pap smear; 59% never asked patients whether they were ever screened for cervical cancer or not, and 63% never referred patients for screening. Among all the respondents only 15 (11.3%) had ever undergone a Pap smear on themselves (Table 3).
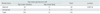
Most nurses (79%) thought that a speculum examination and Pap smear were procedures to be performed by doctors only. A 25% of respondents had no reason for not screening themselves; 61% not felt at risk; 24% never screened themselves as they thought that they had no symptoms; 1% thought that if a woman is a virgin, the Pap test will take away her virginity; for 6% it was embarrassing to have a Pap test done; 3% were afraid of the possible outcome, and 4% thought that if "I am destined to get cancer, I will" (Table 4).
Out of 82 married respondents 39 had taken Pap smear of patients, in comparison to 32 out of 51 unmarried and this difference was statistically insignificant (p>0.05) (Table 5). The respondents who had had Pap smear were from the married group only, so the association between respondents' marital status and Pap smear history was statistically significant (p<0.05) (Table 6).
Cervical cancer despite being the commonest genital cancer of women in India, there are no properly organized or high-level opportunistic screening programs for cervical cancer in any of the provincial states of India [7]. Data from population-based cancer registries indicate a slow, but steady, decline in the incidence of cervical cancer. However, the rates are still too high, particularly in the rural areas, and the absolute number of cases is on an increase due to population growth [7]. In the absence of a systematic screening program the expected practice is to opportunistically screen eligible women when they come to health units for other services. In the opportunistic screening system (at antenatal, postnatal, family planning visits, reproductive tract infection/sexually transmitted infection clinic, anti retroviral therapy centre centre or for any health complaint) the onus is on the health worker who handles the eligible women to offer screening or refer her to a unit where screening can be done. In our institution the Pap smear is exclusively performed in the gynecological department and all eligible women from other units are referred there for screening. Studies have shown it is possible to train nurses to screen for cervical cancer [8]. Attitudes that screening is to be done by doctors or gynaecologists only needs to change. The survey revealed that the hospital played a limited role as a source of information on Pap smear. Although the Pap smear based screening program is not feasible in low resource settings like India due to economical and logistic reasons as there is a lack of trained pathologists and equipped laboratories. This calls for a re-orientation of nurses, paramedicals and health workers and a need for introduction of simpler cervical cancer screening methods such as visual inspections that are more sustainable [9].
Our results resemble the similar study from Turkey [10] and shows that almost all respondents had heard about the Pap smear, but only one-half of them knew that it can detect both cancerous and precancerous lesions of cervical cancer. The rest believed that it is to detect existing cancer and required to be done in symptomatic cases only. Despite considerable awareness of a link between cervical cancer and sexual activity, as well as the role of sexually-transmitted infections, only 54% of the respondents had heard of the HPV; while most were ignorant about HPV vaccine.
Our finding that married women are more likely to be screened is consistent with previous studies in India [11]. The proposed reason is that married women may receive more frequent obstetric or gynecological care, making them more responsive to reproductive health care [12]. Because sexual relationships outside marriage are not culturally accepted in many rural areas of India [13], unmarried women normally refuses to screen themselves out of fear of the potential social stigma they would suffer if they had a test perceived to be used for sexually active women.
A quarter of respondents perceived cervical cancer as a terminal illness with no hope for a cure, even when detected in the early stages. The pessimistic attitude towards cancer and death needs to be addressed. The belief that death is inevitable when cancer is present has been identified as a barrier to participation in cancer screening, detection and treatment [14]. In departments other than gynecology, the negative practice among nurses of not screening patients who come under their care could be attributed to their routines, but this would not explain the reluctance to get screened themselves despite the availability of a free service almost any time they wished to. Among the eligible respondents 89% had never screened themselves because they did not feel vulnerable to the disease. It is unlikely that these medical workers will ever motivate others or advise them until their doubts are cleared. The lack of depth on knowledge of cervical cancer in staff nurses can be explained by their training curriculum. Until recently, cervical cancer prevention issue has been the concern of physicians. In the proposed diagnosis and treat strategies [15] there will be need to integrate cervical cancer prevention issues in the nurses' training curriculum. Nurses will form the backbone for informing the population, as they are the first port of entry into the health system. It remains to be seen which approach is best for cervical cancer control for our country.
There are certain limitations inherent to the design of the present study; firstly, regarding the questions which are mainly recognition and some recall type. Both the recall and recognition questions have limitations. We predicted that recognition scores would be greater than recall scores [16], but it is difficult to determine which better captures the concept of cancer awareness. Recall underestimates awareness because it is limited by memory, while recognition overestimates awareness because participants find it easy to guess. Secondly, the method used for estimating the practice of Pap smears-namely self-reported test history, which may be faulty due to inaccurate recall or desirability bias [15]. Thirdly, the order of the questions may have an impact on the findings. However, in most situations it is not pragmatically feasible to randomize the order in which the questions are asked, and possible priming effects were considered when designing the measure. However, there is a need for further investigation on different approaches to measure cancer knowledge related to behavioral outcomes, and identifying best measure to predict early cancer.
The study showed that despite knowledge of the gravity of cervical cancer and prevention by screening using a Pap smear, attitudes and practices among nurses towards cervical cancer screening were negative; especially uptake of Pap smear test is abysmally poor.
Figures and Tables
References
1. Standard & Guidelines, Cervical and breast cancer screening by VIA & CBE. 2006. New York: The United Nations Population Fund.
2. Desai M. An assessment of community based cancer screening program among Indian women using the Anganwadi workers. J Obstet Gynecol Ind. 2004. 54:483–487.
3. Adeleke NA, Komolafe JA. Knowledge, attitude and practice of cervical cancer screening among women of reproductive age group in Osogbo, south western Nigeria. Sex Health Matters. 2007. 8:70–73.
4. Postgraduate Institute of Medical Education and Research. Guidelines for cervical cancer screening programme. Government of India-World Health Organization Collaborative Programme (2004-2005). 2006. Chandigarh, India: Postgraduate Institute of Medical Education and Research.
5. National Commission on Macroeconomics and Health. Burden of disease in India. 2005. New Delhi, India: Ministry of Health & Family Welfare, Government of India.
6. Hainer R. New guidelines: Pap test should start at age 21 [Internet]. 2009. cited 2012 May 30. Atlanta: Cable News Network (CNN);Available from: http://edition.cnn.com/2009/HEALTH/11/20/pap.cervical.cancer/index.html.
7. Sankaranarayanan R, Budukh AM, Rajkumar R. Effective screening programmes for cervical cancer in low- and middle-income developing countries. Bull World Health Organ. 2001. 79:954–962.
8. Chirenje ZM, Chipato T, Kasule J, Rusakaniko S. Visual inspection of the cervix as a primary means of cervical cancer screening: results of a pilot study. Cent Afr J Med. 1999. 45:30–33.
9. Cronje HS, Parham GP, Cooreman BF, de Beer A, Divall P, Bam RH. A comparison of four screening methods for cervical neoplasia in a developing country. Am J Obstet Gynecol. 2003. 188:395–400.
10. Ertem G. Awareness of cervical cancer risk factors and screening behavior among nurses in a rural region of Turkey. Asian Pac J Cancer Prev. 2009. 10:735–738.
11. Sankaranarayanan R, Rajkumar R, Arrossi S, Theresa R, Esmy PO, Mahe C, et al. Determinants of participation of women in a cervical cancer visual screening trial in rural south India. Cancer Detect Prev. 2003. 27:457–465.
12. Siahpush M, Singh GK. Sociodemographic predictors of pap test receipt, currency and knowledge among Australian women. Prev Med. 2002. 35:362–368.
13. Bott S, Jejeebhoy S, Shah I, Puri C. Towards adulthood: exploring the sexual and reproductive health of adolescent in South Asia. 2003. Geneva: World Health Organization.
14. Powe BD, Finnie R. Cancer fatalism: the state of the science. Cancer Nurs. 2003. 26:454–465.
15. Denny L, Kuhn L, De Souza M, Pollack AE, Dupree W, Wright TC Jr. Screen-and-treat approaches for cervical cancer prevention in low-resource settings: a randomized controlled trial. JAMA. 2005. 294:2173–2181.
16. Waller J, McCaffery K, Wardle J. Measuring cancer knowledge: comparing prompted and unprompted recall. Br J Psychol. 2004. 95(Pt 2):219–234.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download