Abstract
Objective
Ductal lavage (DL) involves evaluation of the ductal system of the breast for detection of intra-ductal carcinomas and precursor lesions by collecting breast epithelial cells using a small-gauge catheter inserted into a ductal orifice on the nipple. The aim of this survey was to analyze cytologic features of samples obtained from low-risk women with DL and to elucidate the efficacy of this diagnostic modality in evaluating fluid production, cannulating and determining atypical breast epithelial cells.
Methods
Into this prospective study were consecutively registered 80 women between ages 28 to 67. Nipple aspiration was performed to identify all fluid-yielding ducts. According to the grading of specific features the interpretation of the sample included: normal/benign (category, 0), mild atypical (category, I), markedly atypical (category, II) or malignant (category, III) disorders.
Results
Ninety five percent (316/334) of the nipple aspirate fluid samples were classified as category 0, 4.8% (16/334) as category I and 0.2% (2/334) as category II changes. Category III disorders were not detected. Therefore, in 80% of the women examined results were within normal limits while 17.5% of the participants presented mild atypical and 2.5% markedly atypical rates.
Conclusion
DL collection procedure proved to be rapid as well as acceptable by the women studied. It retains the advantage over other methods of nipple aspirate fluid in that it is easy to perform, thereby removing most clinician variability. It also helped low risk women to discriminate those with breast disorders that require additional investigation, further follow-up or administration of preventive medication.
Breast cancer (BC) is the second leading cause of cancer death in women in Greece as well as in the Western European Countries and United States [1,2]. Risk biomarkers with a lifetime accepted positive predictive value for BC are limited to individuals with mutation in genes responsible for hereditary breast cancer (HBC), lobular carcinoma in situ or atypical hyperplasia. Thus, the vast majority of women interested in risk assessment would not qualify for genetic testing nor have they undergone a diagnostic biopsy for precancerous lesion detection [3]. Moreover, physical examination and mammographic imaging remain the only currently acceptable methods for investigation of breast lesions. Therefore, several early stage neoplastic disorders cannot be elucidated, especially if they arise in densely fibrotic breast tissue. Thus, there is an immense interest in developing new methods for BC screening that would allow prompt detection of neoplasms as well as precancerous lesions [4].
It is well known that the majority of BCs originate in the epithelium of the breast ducts. Recent investigations support that most lesions are slow growing and progress from precancerous cells, which present cellular and nuclear changes that can be identified microscopically [5]. Evidence of precancerous lesions - ductal epithelial atypia/atypical ductal hyperplasia (ADH) - has been correlated significantly with future BC development. Ductal lavage (DL) involves evaluation of the ductal system of the breast for detection of intra-ductal carcinomas and precursor lesions (ADH) by collecting breast epithelial cells from the lining of the ducts, using a small-gauge catheter inserted into a ductal orifice on the nipple, permitting direct access to exfoliated breast duct epithelial cells [6,7]. The majority of nipple aspirate fluid (NAF) studies estimating DL procedure were conducted in increased genetic risk women [8]. The aim of this survey was to analyze cytologic features of samples obtained from low-risk women with DL and to elucidate the efficacy of this diagnostic modality in evaluating fluid production, cannulating and determining atypical breast epithelial cells in this population.
Into this prospective study were consecutively registered 80 women between ages 28 to 67 years old who attended the Breast Clinic of our university hospital from 01/06/06 to 30/06/09. The Institutional Review Board approved the study, but since written consent was obtained in each case no Ethical Committee approval was necessary. Gail risk profile calculated at enrolment was used to characterise women as low risk. Exclusion criteria included: Gail risk ≥1.7%, pregnancy or lactation within 6 months of enrolment, identification of BC, ovarian cancer, history of ductal carcinoma in situ, breast irradiation, prior chemotherapy, allergy to xylocaine, peri-areolar breast surgery which might disrupt the ductal system of the breast, a breast implant or prior silicone injections and active infection or inflammation in the breast. Additional candidates who did not attend both pre- and post-DL clinic visits were excluded from the analysis (n=11). Standard preparation of the breast, including topical anaesthetic cream applied to the nipple/areola 60 minutes prior to the procedure, was provided to all DL participants. The nipple/areolar complex surface was gently probed with a micro dilator tip prior to DL to confirm adequate anaesthesia. In women who reported pain, additional topical anaesthesia and/or subcutaneous injections of xylocaine around the base of the nipple were administered. Nipple aspiration was performed to identify all fluid-yielding ducts. We attempted to reveal and cannulate all visible ducts, regardless of NAF status. After successful catheter insertion, 3-5 mL of 2% xylocaine was infused, followed by 20 mL of sterile normal saline, whenever possible. The breast was massaged to facilitate recovery of the DL fluid into the catheter collection chamber. An average of 5 mL was collected per duct and the lavage fluid was preserved in CytoLyt and stained by a standard Papanicolaou technique. This preparation maximized cell recovery and preservation along with direct comparison with nipple aspirate. DL was performed by one clinician and the preparation of the breast through the completion of the procedure required approximately an hour for each studied breast. The location of each lavaged duct was recorded in a standard scheme and stored in the participant's permanent medical record. All suitable DL specimens were screened by a cytologist experienced in the evaluation of NAFs. According to the grading of specific features (cell arrangement, size, variation, nuclear characteristics, nucleoli and background findings as nonepithelial cells, microcalcifications and necrosis) the interpretation of the sample included: normal/benign (category 0), mild atypical (category I), markedly atypical (category II) or malignant (category III) disorders [9,10].
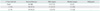
During the study period 80 women (n=80) were successfully enrolled and 334 ducts were examined by DL (mean number of ducts per person, 4.1). Overall characteristics of the study participants are summarized in Table 1. Average age was 45.81 years (range, 28 to 67 years). There was no significant difference between age and fluid production while 32 women (40%) proved fluid producers. Furthermore, 55% of women with a lactation history produced NAF while 25% of participants who never lactated were fluid producers. Mean Gail risk index was 1.1% (Table 2).
Final cytology results of the 334 available for evaluation specimens are summarized in Table 3. In case of multiple NAF values, the most abnormal was taken into consideration. Ninety five percent (316/334) of the NAF samples were classified as category 0, 4.8% (16/334) as category I and 0.2% (2/334) as category II changes. Category III disorders were not detected. Therefore, in 80% of the women examined results were within normal limits while 17.5% of the participants presented mild atypical and 2.5% markedly atypical rates. A total of 62 women (70%) were surveyed for procedure acceptance three weeks after the intervention. The average immediate postoperative comfort assessment rating was 6 on a scale of 1-10 (one being most comfortable). The nipple, areola, and breast areas were visually assessed immediately following the procedure. Major adverse events were not reported. DL was accomplished in all participants. Minor events including bleeding or small surface lacerations were apparent in two cases. These were treated with topical ointment and meticulous observation, and all symptoms resolved without further intervention. Eighty-three percent of the participants declared that they would repeat the DL procedure.
The 16 women presented with category I-II changes were referred again to the breast clinic of our institution for further examination. Concerning those with category I changes (n=14), they were informed that hyperplasia is considered to be a physiological response to a specific stimulus, while the cells of a hyperplastic growth remain subject to normal regulatory control mechanisms. Their appearance in the breast may be attributed to several causes, including increased demand (e.g., proliferation of basal layer of epidermis to compensate skin loss), chronic inflammatory response, hormonal dysfunctions, or compensation for damage or disease elsewhere. It was also noted that many authors support that hyperplasia is the earliest precursor for the development of breast premalignant changes, and this is something that is to be clarified in the future. Thus, it was explained that there was no need for further investigation and all women returned to their annual follow-up program.
For the two women (2.5%) with atypical hyperplasia a more detailed explanation included information that ADH is a definitely benign lesion of the breast that indicates an increased risk of BC. Since a thorough evaluation was conducted and imaging results were within normal ranges, a follow-up programme of mammograms and physician appointment every 6 months was implemented. Follow-up information was obtained for the next 3 years and all women with atypical hyperplasia remained asymptomatic [11].
In accordance with recent surveys atypical hyperplasia of the breast ductal epithelium is associated with an increased risk of subsequent development of BC [12-15]. In this prospective study we report cytologic examination of NAF samples collected from otherwise asymptomatic healthy women with DL. We suggest that it is technically feasible to detect normal as well as atypical breast ductal epithelial cells using routine cytologic preparation methods, even in low risk women. We also observed that 75% of the participants had adequate cellularity (defined as greater than 10 ductal epithelial cells present) which is similar to other studies that recorded cytology results, the mean number of ducts cannulated per person was 4, and only 11 nipples could not be examined as a result of incomplete catheterization. Nevertheless, women in whom lavage specimens had inadequate cellularity were not excluded from this analysis. Thus all included participants provided at least one adequate specimen.
Nipple aspiration, the former type of collecting nipple fluid, is characterized by the advantage of being a non-invasive, well tolerated, easy to perform and inexpensive route for evaluating breast epithelium. Its significance is limited by the small amounts of aspirate available for analysis, the relatively low cellular yield, and the fact that a number of women are not fluid yielders. DL, despite its invasiveness, produces material that is much more cellular than NAF that allows duct specific sampling. This method of obtaining breast ductal epithelial cells can be quickly performed in an office setting; patients do not need to be referred to a specialist and can potentially have the procedure by trained non-physician staff [16,17].
The current study highlights the same limitations described to other studies of DL or nipple fluid cytology. All women included in the study were visiting a breast clinic and the majority presented with breast symptoms for evaluation, mainly atypical pain. The ethnic make-up of this cohort was predominantly white and therefore the associated relative risks may not be applicable to other ethnicities with varying physiologic factors, influencing breast epithelium. Moreover, only 2/4 of the collecting ducts were sampled so it is essential to realize that only a small proportion of the ductal system of the breast is sampled by DL. As early detection of BC is critical for prompt cure, being able to identify women at high risk for neoplastic transformation would justify closer follow-up and the implementation of multiple methods to ensure early detection. NAF examination may enhance current risk prediction models and provide a convenient and inexpensive way to help screening individuals at increased risk for BC [18-20].
The DL procedure has been reported to be a feasible way to obtain NAF samples for cytological assessment and there are clear advantages to using it over manual collection techniques. Information regarding proliferative breast epithelium is currently obtained for use in the Gail model via biopsy, an invasive screening tool for large populations of women. Nevertheless, the obligatory use of biopsy for Gail model definition is not implemented as relevant reference about potential previous invasive procedure consists essential information during Gail model specification process. Breast biopsies are performed once a woman is symptomatic, limiting their ability to provide predictive value in determining who is at risk for BC. On the other hand, NAF assessment is not a diagnostic test for BC detection. NAF production and cytological assessment may be used in conjunction with the Gail model for risk prediction. Despite the absence of significant association between our cytology findings and patients' Gail score, cytological variation indicative of increased risk of BC development provides essential contribution in discriminating low risk women with malignant potential. Our experience suggests that DL has yielded enough numbers of exfoliated epithelial cells to permit reliable cytological diagnosis or to support further research activities. Therefore, it is likely to play a pivotal role in BC screening protocols.
Overall, the DL collection procedure was proved to be rapid as well as acceptable by the women studied as it posed little physical risk. It retains the advantage over other methods of NAF in that it is easy to perform, thereby removing most clinician variability. Despite the limited sample and restricted follow-up time it also helped low risk women to discriminate those with breast disorders that require additional investigation, further follow-up or administration of preventive medication. Nevertheless future studies are necessary to explain the association between our findings and increased BC risk. It is also necessary to test breast fluids for specific biomarkers indicative of malignancy related to genomic and proteomic analysis in order to further the research on etiologic factors involved in breast carcinogenesis and BC prevention [21].
Figures and Tables
References
1. Sathiakumar N, Delzell E, Morrisey MA, Falkson C, Yong M, Chia V, et al. Mortality following bone metastasis and skeletal-related events among women with breast cancer: a population-based analysis of U.S. Medicare beneficiaries, 1999-2006. Breast Cancer Res Treat. 2012. 131:231–238.
2. Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, et al. Cancer statistics, 2006. CA Cancer J Clin. 2006. 56:106–130.
3. Smigal C, Jemal A, Ward E, Cokkinides V, Smith R, Howe HL, et al. Trends in breast cancer by race and ethnicity: update 2006. CA Cancer J Clin. 2006. 56:168–183.
4. Hollingsworth AB, Singletary SE, Morrow M, Francescatti DS, O'Shaughnessy JA, Hartman AR, et al. Current comprehensive assessment and management of women at increased risk for breast cancer. Am J Surg. 2004. 187:349–362.
5. Pinder SE, Ellis IO. The diagnosis and management of preinvasive breast disease: ductal carcinoma in situ (DCIS) and atypical ductal hyperplasia (ADH) - current definitions and classification. Breast Cancer Res. 2003. 5:254–257.
6. King EB, Chew KL, Petrakis NL, Ernster VL. Nipple aspirate cytology for the study of breast cancer precursors. J Natl Cancer Inst. 1983. 71:1115–1121.
7. Baltzell KA, Moghadassi M, Rice T, Sison JD, Wrensch M. Epithelial cells in nipple aspirate fluid and subsequent breast cancer risk: a historic prospective study. BMC Cancer. 2008. 8:75.
8. Maddux AJ, Ashfaq R, Naftalis E, Leitch AM, Hoover S, Euhus D. Patient and duct selection for nipple duct lavage. Am J Surg. 2004. 188:390–394.
9. Buehring GC, Letscher A, McGirr KM, Khandhar S, Che LH, Nguyen CT, et al. Presence of epithelial cells in nipple aspirate fluid is associated with subsequent breast cancer: a 25-year prospective study. Breast Cancer Res Treat. 2006. 98:63–70.
10. Dooley WC, Ljung BM, Veronesi U, Cazzaniga M, Elledge RM, O'Shaughnessy JA, et al. Ductal lavage for detection of cellular atypia in women at high risk for breast cancer. J Natl Cancer Inst. 2001. 93:1624–1632.
11. O'Shaughnessy JA, Ljung BM, Dooley WC, Chang J, Kuerer HM, Hung DT, et al. Ductal lavage and the clinical management of women at high risk for breast carcinoma: a commentary. Cancer. 2002. 94:292–298.
12. Patil DB, Lankes HA, Nayar R, Masood S, Bryk M, Hou N, et al. Reproducibility of ductal lavage cytology and cellularity over a six month interval in high risk women. Breast Cancer Res Treat. 2008. 112:327–333.
13. Visvanathan K, Santor D, Ali SZ, Brewster A, Arnold A, Armstrong DK, et al. The reliability of nipple aspirate and ductal lavage in women at increased risk for breast cancer: a potential tool for breast cancer risk assessment and biomarker evaluation. Cancer Epidemiol Biomarkers Prev. 2007. 16:950–955.
14. Wrensch MR, Petrakis NL, Miike R, King EB, Chew K, Neuhaus J, et al. Breast cancer risk in women with abnormal cytology in nipple aspirates of breast fluid. J Natl Cancer Inst. 2001. 93:1791–1798.
15. London SJ, Connolly JL, Schnitt SJ, Colditz GA. A prospective study of benign breast disease and the risk of breast cancer. JAMA. 1992. 267:941–944.
16. Khan SA, Baird C, Staradub VL, Morrow M. Ductal lavage and ductoscopy: the opportunities and the limitations. Clin Breast Cancer. 2002. 3:185–191.
17. Loud JT, Beckjord EB, Nichols K, Peters J, Giusti R, Greene MH. Tolerability of breast ductal lavage in women from families at high genetic risk of breast cancer. BMC Womens Health. 2009. 9:20.
18. Khan SA, Lankes HA, Patil DB, Bryk M, Hou N, Ivancic D, et al. Ductal lavage is an inefficient method of biomarker measurement in high-risk women. Cancer Prev Res (Phila). 2009. 2:265–273.
19. Tice JA, Miike R, Adduci K, Petrakis NL, King E, Wrensch MR. Nipple aspirate fluid cytology and the Gail model for breast cancer risk assessment in a screening population. Cancer Epidemiol Biomarkers Prev. 2005. 14:324–328.
20. Cyr AE, Margenthaler JA, Conway J, Rastelli AL, Davila RM, Gao F, et al. Correlation of ductal lavage cytology with ductoscopy-directed duct excision histology in women at high risk for developing breast cancer: a prospective, single-institution trial. Ann Surg Oncol. 2011. 18:3192–3197.
21. Dubowy A, Raubach M, Topalidis T, Lange T, Eulenstein S, Hunerbein M. Breast duct endoscopy: ductoscopy from a diagnostic to an interventional procedure and its future perspective. Acta Chir Belg. 2011. 111:142–145.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download