Abstract
Objective
This study aim was to evaluate indications and outcomes of surgical interventions performed in patients with gestational trophoblastic neoplasm.
Methods
During January 1995 to December 2005, 110 patients with a diagnosis of persistent gestational trophoblastic neoplasm were treated in our Gynecologic Oncologic Department. Risk score calculation was carried out based on the revised FIGO 2000 scoring system for gestational trophoblastic neoplasm. Data from the patients' records and pathologic reports were analyzed by the chi-square and Fisher's exact tests and logistic regression. The Kaplan-Meier method including the log rank test was used to compare survival and recurrence.
Results
Eight patients did not complete their treatment and were excluded from the study. We evaluated treatment responses and outcomes in 102 patients. Seventy-nine patients (77.5%) responded fully to chemotherapy while 23 patients (22.5%) required surgery. Among 23 patients who underwent surgery, 10 cases (43.5%) had bleeding, and 13 cases (56.5%) had drug resistance. Several factors were found to be significantly different between the groups who responded to chemotherapy and those who needed surgery, including age (p=0.001), antecedent non-molar pregnancy (0.028), tumor stage (p=0.009), and pre-treatment risk scores (p=0.008). But, the total courses of chemotherapy (p=0.521), need to salvage chemotherapy (p=0.074), survival rates (p=0.714), and disease free survival rates (p=0.206) were not significantly different.
There are significant regional and racial differences in the incidence of gestational trophoblastic neoplasia (GTN) worldwide. The incidence of GTN is higher in Asia and Latin America than in western countries [1]. GTN is one of the most curable malignancies. The intrinsic sensitivity of the tumor to certain antineoplastic agents, in particular sensitive assays for human chorionic gonadotropin, has made it detectable and capable of being efficiently followed-up [2]. GTN requires chemotherapy, surgery or a combined treatment modality [3]. Chemotherapy is the main modality of treatment in patients with GTN. The cure rate in patients with low-risk GTN is approximately 100% and is estimated to exceed 80% in patients with high-risk GTN [4,5]. Surgical treatment such as a hysterectomy is rarely needed. However, in some countries, the incidence of hysterectomy has been estimated to be up to 35% in all cases of gestational trophoblastic disease [6].
Nowadays, surgery in the management of GTN is not the first-line therapy any more. However, it has been reported that one-third of patients need surgery to achieve favorable treatment for GTN. This is more important in patients with metastases. In addition, in those who do not have metastases, surgery by reducing the bulk of the tumor in the uterus may decrease morbidity and mortality [4-6]. The aim of this study was assessment of the efficacy of surgery in GTN patients and identification of pretreatment clinical parameters that may predict therapeutic response to surgery, and outcomes of surgical procedures performed in our university hospital in Tehran, Iran for patients with GTN.
In this retrospective study, medical records of patients who underwent surgical treatment for GTN in our hospital between January 1995 and December 2005 were reviewed. A total of 110 patients received chemotherapy in this center during the study period. Among them, only 23 patients underwent surgery in addition to chemotherapy.
The evaluated parameters included histological diagnosis, FIGO stage, risk score, antecedent pregnancy event, response to treatment, indication of surgery, and prognosis applied. Risk score calculation was based on the revised FIGO 2000 scoring system for GTN [7]. This scoring system conveniently predicts the potential for resistance to chemotherapy. A patient's total score is obtained by summing the individual score for each prognostic factor. The total score of ≤6 is considered low risk, whereas the total score of ≥7 is considered high risk. Patients of the high risk group require intensive combined chemotherapy to achieve remission [7].
The study protocol was approved by Ethics Committee of Tehran University of Medical Sciences. For statistical analyses, descriptive indices such as frequency, percentage, mean, and standard deviation (SD) were used to express data. To compare variables, the chi-square, Fisher's exact tests and logistic regression were used. The Kaplan-Meier method including the log rank test was used to compare survival and recurrence.
Of the 110 patients with persistent GTN, 80 were recognized as low risk and 30 as high risk patients. Eight patients (8/110) did not complete their treatment in our center and were thereby excluded from the study. Fig. 1 shows the follow up diagram of the study. Out of the remaining 102 patients who completed their treatment (34 patients had score ≥7 while others had scores below 7), 77.5% (79 patients) responded fully to chemotherapy while 22.5% (23 patients) required surgery. Of the 23 patients, 18 underwent hysterectomy (6 and 12 cases for bleeding and drug resistance, respectively), 1 underwent lung resection (for dyspenea and hemoptesis), 2 underwent uterine wedge resection (one for excision of isolated lesion in the uterus and another one for bleeding), 1 underwent small bowel resection (for bleeding), and 1 underwent craniotomy (for life-threatening cerebral hernia).
Thirteen out of 23 patients (56.5%) had a score ≥7 while others had scores below 7. All these patients received chemotherapy, but four of them needed additional chemotherapy with more than one regimen. As stated earlier, the majority of patients who needed surgery underwent hysterectomy (78.3%). The indications for hysterectomy included localized chemo-resistant disease (12/18) and intra-abdominal bleeding or uncontrollable vaginal bleeding (6/18), indicating that hysterectomy as an emergency procedure was necessary in six patients only. Sixteen out of these 18 patients had abnormal histology (9 invasive moles, 5 choriocarcinomas, and 2 placental site trophoblastic tumors), and two had normal histology. The incidence of hysterectomy was 17.6% among the patients with persistent GTN and 44.4% (8/18) of patients who needed hysterectomies were in the high risk group. All women in the low-risk group received single-agent chemotherapy in addition to hysterectomy, and all were cured.
Several factors were found to be significantly different between the groups whose response to chemotherapy and those who need surgery, including age (p=0.001), antecedent non-molar pregnancy (0.028), tumor stage (p=0.009), and pre-treatment risk scores (p=0.008). But, the total course of chemotherapy and need for salvage chemotherapy were not significantly different (p=0.521, p=0.074, respectively).
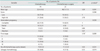
Median number of chemotherapy were 7 (range, 1 to 25) and 6 (range, 3 to 15), respectively, in the chemotherapy and combined groups. The association between all variables with type of treatment is summarized in Table 1. For 23 patients who underwent surgery, 10 cases (43.5%) had bleeding, and 13 cases (56.5%) had drug resistance. There was no statistically significant difference based on some variables such as age, stage, score, antecedent pregnancy, and histology (Table 2).
The survival rates of the chemotherapy and combined groups were 94.4% and 100% at 23 months (median time of follow-up), respectively, which remained stable to the end of follow-up in the combined group, but decreased to 86.6% in the chemotherapy group. But, this difference was not statistically significant (p=0.714) (Fig. 2A). The disease free survival rates were 94.5% and 88.9% at 23 months (median time of follow-up) respectively, in the chemotherapy and combined groups, which changed to 87.2% and 71.1% at the end of follow up (Fig. 2B). The mean disease free survival time was 64.2 months (95% CI, 60.1 to 68.3) in the chemotherapy group and 48.2 months (95% CI, 35.3 to 61.2) in the combined group, this difference was not significant (p=0.206).
There were 6 deaths among the total of 102 GTN registered patients. All deaths occurred in the high-risk metastatic group and one (1/23) occurred in the surgery group. This patient had placental site trophoblastic tumor (PSTT) as her primary pathological diagnosis. This 36-year-old patient, who had a history of a full-term pregnancy about five years earlier, underwent abdominal hysterectomy due to severe vaginal bleeding. Pathological examination confirmed PSTT. Stage of her tumor was 4 (with metastasis to the lung and brain). She underwent chemotherapy with etoposide, methotrexate and actinomycin D, alternating with cyclophosphamide plus vincristine (EMA/CO) and radiotherapy as well. However, after receiving 4 EMA-CO cycles, her chemotherapy regimen was changed to etoposide, methotraxate, actinomycin D plus cisplatin, and etoposide (EME-CE) due to non-response. After receiving 9 chemotherapy periods, she died of fever and leucopenia.
Chemotherapy is the main modality of treatment in patients with GTN, but surgery may be needed in patients with hemorrhagic or drug-resistant diseases [7]. We found that patient's age was a predictor for patients who needed surgery. Patients in the surgery group are recognized as a high risk group as indicated by their high pretreatment risk scores and stages. In our series, we found high-risk disease in 56.5% patients in the surgery group that was significantly different between two groups. Severe uncontrolled bleeding from GTN may occasionally necessitate surgery such as an emergency hysterectomy. However, surgery does not seem to have any effect on more courses of chemotherapy [8]. In the present study, emergency hysterectomy was indicated in 6 patients. Based on our findings, the incidence of hysterectomy was 17.6% in patients with persistent GTN. In the study by El-Lamie et al., [6] the overall incidence of hysterectomy was reported to be 35% in patients with persistent GTN. Our study showed that 44.4% of patients who needed hysterectomy were in the high risk group compared with 32% in study of El-Lamie et al. [6]. We showed 46.4% of high risk patients who underwent surgical procedures. This is in line with those reported by Laurin (48%) [9]. In the present study all women in the low-risk group received single-agent chemotherapy in addition to hysterectomy, and all were cured. This finding is similar to that of the study of El-Lamie et al. [6]. Tidy [10] found that 8.8% of women with high-risk disease required salvage hysterectomy following chemotherapy similar to the 11.8% obtained in this study. Pisal et al. [8] showed frequent use of salvage chemotherapy in patients needing hysterectomy, whereas, no increased need to more courses of chemotherapy or salvage chemotherapy was observed in the present study.
In the Newland study [4] of 13 women who underwent hysterectomy, only four showed any histological evidence of residual GTN, whereas in our study out of 18 women who underwent hysterectomy, 16 had abnormal histology. Local uterine resection may be considered if a patient is resistant to chemotherapy and desires to retain fertility. We performed conservative uterine surgery on two young patients with choriocarcinoma. When local resection is considered, ultrasound, MRI scan and/or arteriogram may identify the site of the resistant tumor.
PSTT is a known indication of hysterectomy particularly in those with localized disease who have completed their child-bearing [11]. Some studies show PSTT does not respond well to chemotherapy and metastatic disease associated with poor prognosis [11,12], whereas Schmid et al. [13] reported that performing surgery for stage I disease, and combined surgery and chemotherapy for stage II, III, and IV disease may improve the effectiveness of treatment for PSTTs. Application of "48 months" since antecedent pregnancy as a prognostic indicator of survival may help in selecting patients for risk-adapted treatment. There was one death in the chemotherapy-surgery group. This patient had PSTT as her primary pathological diagnosis. Her tumor stage was IV and it passed four years from her last pregnancy.
The gastrointestinal tract is a rare site of metastasis. Patients with metastasis to this tract may show symptoms of an acute abdomen [14]. One of our patients, who had stage IV GTN with a total score of 11, experienced a sudden episode of severe rectal hemorrhage following the first chemotherapy course. An emergency laparotomy was done and a lesion was discovered in the ascending colon and resected. Histological examination confirmed metastatic GTN to the colon.
The diagnosis of GTN may be confirmed only after a thoracotomy has been performed, particularly in those patients with a non-molar antecedent pregnancy. We had one such patient. Bleeding within cerebral metastasis can be catastrophic, and it is recommended to treat brain metastases with surgery or radiotherapy if raised intra-cranial pressure or abnormal neurological signs develops prior to the commencement of systemic chemotherapy [15,16]. We had one such patient. In our study we showed that surgery did not show any benefit on lesser courses of chemotherapy and patient prognosis. Feng et al. [17] also showed some patients may be unlikely to benefit from surgical management.
Although chemotherapy is the main modality of treatment in patients with GTN, surgery may be needed in selected patients with hemorrhagic or drug-resistant diseases. These patients are considered high risk. Patients who need surgery have more chance of being in the high risk group as indicated by their high pretreatment risk scores and stages, but it seems that surgery does not have any effect on more courses of chemotherapy. It is concluded that diagnosis in primary stages of disease has a significant importance, because considering the results of present study it seems that despite the increased need for surgery in late stages, except for emergency cases such as bleeding, surgery does not accelerate patient improvement. These findings might also be related to the small sample size, and hopefully future studies on drug resistance cases in a larger sample size will clarify this result.
Figures and Tables
 | Fig. 2(A) Kaplan-Meier curves of overall survival according to type of treatment. (B) Kaplan-Meier curves of disease-free survival according to type of treatment. |
ACKNOWLEDGMENTS
The authors wish to sincerely thank Ellen Barlow RN BN, from Gynecological Cancer Centre, The Royal Hospital for Women, Australia for editing this article. Also, the authors would like to thank Farzan Institute for Research and Technology for technical assistance.
References
1. Altieri A, Franceschi S, Ferlay J, Smith J, La Vecchia C. Epidemiology and aetiology of gestational trophoblastic diseases. Lancet Oncol. 2003. 4:670–678.
2. Ghaemmaghami F, Ashraf-Ganjooie T. Gestational trophoblastic neoplasia. Asia Pac J Clin Oncol. 2006. 2:9–21.
3. Ngan HY. The practicability of FIGO 2000 staging for gestational trophoblastic neoplasia. Int J Gynecol Cancer. 2004. 14:202–205.
4. Newlands ES. The management of recurrent and drug-resistant gestational trophoblastic neoplasia (GTN). Best Pract Res Clin Obstet Gynaecol. 2003. 17:905–923.
5. Ghaemmaghami F, Behtash N, Soleimani K, Hanjani P. Management of patients with metastatic gestational trophoblastic tumor. Gynecol Oncol. 2004. 94:187–190.
6. El-Lamie IK, Shehata NA, Abou-Loz SK, Ei-Lamie KI. Experience of the Gynecologic Oncology Unit at Ain Shams University in the treatment of gestational trophoblastic tumors. Int J Gynecol Cancer. 2000. 10:488–496.
7. Soper J, Creasman WT. Disaia PJ, Creasman WT, editors. Gestational trophoblastic disease. Clinical gynecologic oncology. 2007. 7th ed. Philadelphia: Mosby Elsevier;201–230.
8. Pisal N, North C, Tidy J, Hancock B. Role of hysterectomy in management of gestational trophoblastic disease. Gynecol Oncol. 2002. 87:190–192.
9. Lurain JR, Singh DK, Schink JC. Role of surgery in the management of high-risk gestational trophoblastic neoplasia. J Reprod Med. 2006. 51:773–776.
10. Tidy J. Hancock BW, Newlands ES, Berkowitz RS, Cole La, editors. The role of surgery in the management of gestational trophoblastic disease. Gestational trophoblastic diseases. 2009. 3rd ed. 430–446.
11. Feltmate CM, Genest DR, Wise L, Bernstein MR, Goldstein DP, Berkowitz RS. Placental site trophoblastic tumor: a 17-year experience at the New England Trophoblastic Disease Center. Gynecol Oncol. 2001. 82:415–419.
12. Gillespie AM, Liyim D, Goepel JR, Coleman RE, Hancock BW. Placental site trophoblastic tumour: a rare but potentially curable cancer. Br J Cancer. 2000. 82:1186–1190.
13. Schmid P, Nagai Y, Agarwal R, Hancock B, Savage PM, Sebire NJ, et al. Prognostic markers and long-term outcome of placental-site trophoblastic tumours: a retrospective observational study. Lancet. 2009. 374:48–55.
14. Balagopal P, Pandey M, Chandramohan K, Somanathan T, Kumar A. Unusual presentation of choriocarcinoma. World J Surg Oncol. 2003. 1:4.
15. Berkowitz RS, Goldstein DP. Berek JS, Hacker NE, editors. Gestational trophoblastic neoplasia. Gynecologic oncology. 2010. 5th ed. Philadelphia: Williams & Wilkins;593–613.
16. Newlands ES, Holden L, Seckl MJ, McNeish I, Strickland S, Rustin GJ. Management of brain metastases in patients with high-risk gestational trophoblastic tumors. J Reprod Med. 2002. 47:465–471.
17. Feng F, Xiang Y, Li L, Wan X, Yang X. Clinical parameters predicting therapeutic response to surgical management in patients with chemotherapy-resistant gestational trophoblastic neoplasia. Gynecol Oncol. 2009. 113:312–315.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download