Abstract
Objective
To evaluate whether human papillomavirus (HPV) genotype is associated with poor prognosis of uterine cervical cancer treated primarily with radiotherapy.
Methods
HPV genotyping was performed in 181 radiotherapy patients using SPF10 polymerase chain reaction and HPV reverse hybridization line probe assay. Univariate and multivariate Cox regression analysis was performed to explore the prognostic factors. Bivariate analysis was performed to investigate any association between HPV genotype and the rest of the prognostic factors.
Results
HPV type 18 was associated with poor disease-free survival on univariate analysis but the statistical significance was abolished when multivariate analysis was applied. Bivariate analysis was performed to examine the possible confounding factors influencing the effect of HPV 18 on prognosis. As a result, adeno/adenosquamous carcinoma histology reduced the prognostic importance of HPV 18 by 66% (2.4 to 1.6), and was the only factor which reduced the hazard ratio of HPV 18. When compared to non-18 squamous cell carcinoma, type 18 increased the risk of recurrence up to 4-fold in adeno/adenosquamous/HPV 18 and 3.7 in adeno/adenosquamous/non-18, and to 2-fold in squamous carcinoma/HPV 18, respectively.
Conclusion
Our data suggest that the prognostic significance of HPV 18 genotype is substantial on radiotherapy outcome, but can be underestimated because of the close association of the HPV 18 and adenocarcinoma/adenosquamous carcinoma histology. Both HPV 18 and histologic type should be regarded as strong prognostic factors in considering the treatment outcome of the uterine cervical cancer.
The significance of human papillomavirus (HPV) 18 genotype in treatment outcome is one of the most controversial issues regarding HPV-related human tumors [1-7]. In most of the studies regarding this subject, low frequency of HPV 18 infection (around 10% to 20%) often resulted in borderline or less than a statistically significant impact on prognosis [1,4,5,7]. Likewise, Kim et al. [7] showed a tendency for the HPV 18 genotype to be associated with poor disease-free survival (DFS) and with a trend for poor local control. However, the significance of HPV 18 was lost in multivariate analysis in that study.
Because a recent large-scale study showed that HPV 18 is a strong prognostic factor for relapse-free survival in patients with early-stage cervical cancer treated by surgery [4], the authors felt that it was important to clarify that the tumors with HPV 18 infection are also associated with poor outcome after radiotherapy. If such an association exists, it would be necessary to make efforts to develop a new treatment method in this subset of patients.
This study was performed under the approval of our Institutional Review Board, and informed consent was obtained from all patients. The patients included 181 consecutive radiotherapy patients with International Federation of Gynecology and Obstetrics (FIGO) stage IIA-IVB cervical cancer treated between July 2003 and December 2008 at the National Cancer Center, Korea. Of 181 patients, 167 patients were included in our previous study [7]. Staging work-up included bimanual physical examination, posterior-anterior chest radiography, cystoscopy, and rectosigmoidoscopy in all patients. Magnetic resonance imaging of the pelvis±abdomen was obtained in 180 patients, and either positron emission tomography (PET) scan or PET/CT scan was obtained in 140 patients. Thirty-seven patients included in the previous institutional protocol undertook laparoscopic lymph node staging prior to radiotherapy.
Radiotherapy consisted of whole pelvic external beam radiotherapy (EBRT) and high-dose-rate (HDR) brachytherapy. Midline block was inserted at 36-45 Gy, giving a whole pelvic radiotherapy dose of 45-50.4 Gy. HDR brachytherapy was performed at the beginning of midline block with fractional doses of 4-5 Gy and 5-7 fractions twice a week. Median treatment duration was 58 days (interquartile range, 54 to 64). Most patients were treated with concomitant weekly cisplatin 40 mg/m2 during EBRT, except the 9 patients of stage IVB patients who received concurrent 5-fluorouracil/cisplatin chemotherapy with extended-field radiotherapy. Chemotherapy was not given at all in 19 (10.5%) patients because of their advanced age and expected poor compliance to concomitant chemoradiotherapy. After the conclusion of primary treatment, patients were followed up at 3-month intervals in the first 2 years, at 4-month intervals in the third year, and every 6 months thereafter. Two patients with tumors that showed negative HPV DNA in both HC2 and HPV genotyping were excluded from the study due to the lack of HPV genotype information. Patients with multiple infections including the HPV 18 were grouped as HPV 18 infection.
Genomic DNA was extracted from paraffin-embedded tissue sections or frozen tissues using the QIAamp DNA mini kit (Qiagen, Hilden, Germany). The SPF10 polymerase chain reaction was performed and the amplimers were subsequently analyzed by reverse hybridization on the HPV reverse hybridization line probe assay (INNO-LiPA HPV Genotyping CE [LiPA]; Innogenetics N.V., Gent, Belgium) under the manufacturer's instructions. LiPA permits the specific detection of 16 HPV genotypes, including 14 high-risk HPV (16, 18, 31, 33, 40, 45, 51, 53, 54, 58, 59, 66, 68, 70) and 2 low-risk HPV (HPV 6, 11).
Demographic and clinical characteristics are presented as counts and percentages for categorical variables; median and range are supplied for continuous variables. The distributional differences between groups were assessed using the Pearson chi-square test or Fisher's exact test. As measures of prognostic outcome, DFS and local recurrence-free survival were considered. The multivariate Cox proportional hazards model was employed to adjust the effects of other potential confounding factors such as age, HPV type 18, stage group, nodal status, tumor size, histologic grade, histologic type, and smoking status. The final multivariate Cox model was chosen based on the combination of a stepwise procedure and the hierarchical selection method, as well as consideration of the clinical or biological importance of the variables in the model. A bivariate Cox regression was performed for HPV 18 with other parameters to detect the factor(s) which might have influenced the prognostic significance of HPV 18. All statistical analyses were performed using SAS ver. 9.1 (SAS Inc., Cary, NC, USA). Kaplan-Meier curves were generated using STATA ver. 10 (Stata Co., College Station, TX, USA). All reported p-values are two-sided.
From the beginning of the observed study period until the time of analysis, 54 patients had disease progression, including 40 distant metastases and 18 local recurrences. Five patients developed both local and distant recurrences. The patients were followed up for a median period of 33 months (range, 2 to 72 months). The median follow-up for the patients without recurrence was 42 months (range, 6 to 72 months).
HPV 18 was detected in 20 of the 181 patients (11%) as a single (11) or multiple infections (9). Adenocarcinoma (AD) histology was 17 with 11 AD and 6 adenosquamous carcinoma (ASC). Patients' characteristics are shown in Table 1 in relation to HPV 18.
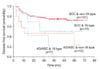
Both HPV 18 and AD/ASC histology were associated with poor DFS in univariate analysis, with hazard ratios of 2.37 and 3.56, respectively (Fig. 1, Table 2). Other prognostic parameters for DFS included HPV 18, advanced stages, presence of nodal metastasis, poorly-differentiated histologic grade, and tumor size larger than 4 cm. In multivariate analysis, advanced stages and AD/ASC histologic type were significantly related to DFS (Table 2).
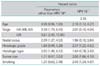
HPV 18 was also associated with larger tumor size, positive nodal status, and also marginally associated with poor histologic differentiation (χ2 test, p=0.04, 0.05, 0.06, respectively). Most prominently, tumors with HPV 18 type were associated with AD/ASC (92% vs. 8% in squamous cell carcinoma [SCC], 59% vs. 41% in AD/ASC for non-18 vs. 18 type, χ2 test, p=0.001). When bivariate Cox regression analysis was performed, the hazard ratio of each parameter remained the same regardless of HPV 18 genotype except for the histologic type for which the hazard ratio has significantly decreased from 2.38 to 1.64 (Table 3). When a combinational group of HPV 18 vs. non-HPV 18, and AD/ASC vs. SCC histology was made and compared, univariate Cox regression analysis revealed that the hazard ratio was increased to 2.1 (95% confidence interval [CI], 0.87 to 4.86; p=0.10), 3.67 (95% CI, 1.54 to 8.74; p=0.003), and 4.05 (95% CI, 1.58 to 10.33; p=0.003), for SCC/HPV 18, AD/ASC/non-HPV 18, and AD/ASC/HPV 18, respectively (Fig. 2) compared to the risk of SCC/non-HPV 18 group. Although statistical significance was not shown, there was a strong tendency for patients with SCC/HPV 18 infection to do worse than SCC/HPV non-18 infection. Five of seven (71.4%) in 18 type in AD/ASC and 6/10 (60%) in non-18 type in AD/ASC relapsed. Four out of 5 ASC showed HPV 18 infection and all of them failed locally and distantly.
In the present analysis, we tried to show the effect of HPV 18 on the outcome of patients with cervical cancer treated with concomitant radiochemotherapy. From the results of our study, it is hard to conclude that HPV 18 is a strong prognosticator on its own, because prognostic significance remains stronger for tumor histology than HPV genotype in multivariate analysis. Our bivariate analysis showed that the effect of HPV 18 on the inferior post-radiotherapy survival was negatively influenced by the relationship between HPV 18 and AD/ASC histology. However, the authors were not able to clearly show the interaction of HPV 18 and AD/ASC histology because the number of patients with AD/ASC tumors was only 17, and also the prognosis of patients with AD/ASC was poor on its own in the absence of HPV 18 infection. The effect of HPV 18 is only supported by the poorer survival which was observed in SCC/HPV 18 tumors compared to the SCC/non-HPV 18 tumors. In our study, the poor prognosis of AD/ASC tumors is mainly contributed by the poor prognosis of ASC tumors. There were 5 patients with ASC tumors and all of the patients failed locally or in distant sites; one patient had non-HPV 18 type and 4 tumors had HPV 18 type. For AD tumors, there was 1 failure in 3 HPV 18 types; however, there were also 5 failures in 9 non-HPV 18 types, making the conclusion that the poor prognosis of AD/ASC tumors is entirely due to the high proportion of HPV 18. The finding that 4 out of 5 cases of ASC showed HPV 18 infection is worth noting because many other authors reported that ASC histology is closely associated with HPV 18 infection. Fujiwara et al. [2] reported 11 patients with ASC who all showed HPV 18 infection in their tumors. HPV 18 was frequently associated with AD/ASC in our study and also in other studies [1,8-15].
We suggest the following common patient characteristics which can be observed in both HPV 18 and AD/ASC tumors. Firstly, median age of the patients is younger in patients with AD/ASC than in patients with SCC tumors [7,16-18], and also in patients with HPV 18 tumors than with non-HPV 18 tumors [5,19], which may indicate shorter period of carcinogenesis. Secondly, viral load is significantly lower in AD/ASC and HPV 18 tumors compared with SCC and non-HPV 18, respectively. In AD/ASC tumors, HPV detection rate ranges from 0-95% and 33.3-100% respectively and is frequently found to be lower than that of SCC [20]. It is not uncommon to find no detectable HPV DNA in AD/ASC [21-24]. The lower viral load of AD/ASC was also shown in our previous study and in other studies [7,20, 21]. It is also known that HPV 18 shows significantly low viral copy number in many studies [23]. Thirdly, AD of the cervix is increasing in incidence worldwide especially in developed countries [24,25]. According to a recent report, HPV16 cervical tumors are decreasing in incidence while those with HPV 18 do not [26]. All of these common clinical characteristics suggest a distinct biology of the two minor but important types of cervical tumors for which mechanisms of carcinogenesis needs to be explicated. Our analysis suggests that there are overlapping cancer biology between AD/ASC and HPV 18. In HPV 18 cervical cancer, earlier integration of the viral genome compared with other types is considered to occur during carcinogenesis, which in turn causes greater chromosomal instability, higher growth rates, and rapid progression of disease [16]. These biological characteristics are likely to cause radioresistance, chemoresistance, and finally poor prognosis which is supported by many preceding reports [27-38]. Further investigation is necessary to reveal the host factors lying behind our observation, along with the possible viral factors.
Figures and Tables
 | Fig. 1Disease-free survival (DFS) by HPV type (A) and histologic types (B). HPV: human papillomavirus, SCC: squamous cell carcinoma, AD/ASC: adenocarcinoma/adenosquamous carcinoma. |
 | Fig. 2Disease-free survival in 4 histology/HPV18 combined groups. SCC: squamous cell carcinoma, AD/ASC: adenocarcinoma/adenosquamous carcinoma, HPV: human papillomavirus. |
Table 2
Univariate and multivariate analyses for disease-free survival with clinicopathologic prognostic factors

Notes
No potential conflict of interest relevant to this article was reported. Goyang, Korea (Grant 1010870), and was conducted under Research Agreement E33024 (Optimizing Treatment of Cervix Cancer Using Radiotherapy and Analysis of Virally-Associated Cellular Resistance) of the International Atomic Energy Agency, Vienna, Austria.
References
1. Burger RA, Monk BJ, Kurosaki T, Anton-Culver H, Vasilev SA, Berman ML, et al. Human papillomavirus type 18: association with poor prognosis in early stage cervical cancer. J Natl Cancer Inst. 1996. 88:1361–1368.
2. Fujiwara H, Mitchell MF, Arseneau J, Hale RJ, Wright TC Jr. Clear cell adenosquamous carcinoma of the cervix: an aggressive tumor associated with human papillomavirus-18. Cancer. 1995. 76:1591–1600.
3. Kitagawa K, Yoshikawa H, Onda T, Kawana T, Taketani Y, Yoshikura H, et al. Genomic organization of human papillomavirus type 18 in cervical cancer specimens. Jpn J Cancer Res. 1996. 87:263–268.
4. Lai CH, Chang CJ, Huang HJ, Hsueh S, Chao A, Yang JE, et al. Role of human papillomavirus genotype in prognosis of early-stage cervical cancer undergoing primary surgery. J Clin Oncol. 2007. 25:3628–3634.
5. Lombard I, Vincent-Salomon A, Validire P, Zafrani B, de la Rochefordiere A, Clough K, et al. Human papillomavirus genotype as a major determinant of the course of cervical cancer. J Clin Oncol. 1998. 16:2613–2619.
6. Im SS, Wilczynski SP, Burger RA, Monk BJ. Early stage cervical cancers containing human papillomavirus type 18 DNA have more nodal metastasis and deeper stromal invasion. Clin Cancer Res. 2003. 9:4145–4150.
7. Kim JY, Park S, Nam BH, Roh JW, Lee CH, Kim YH, et al. Low initial human papilloma viral load implicates worse prognosis in patients with uterine cervical cancer treated with radiotherapy. J Clin Oncol. 2009. 27:5088–5093.
8. Andersson S, Rylander E, Larson B, Sigurdardottir S, Backlund I, Sallstrom J, et al. Types of human papillomavirus revealed in cervical adenocarcinomas after DNA sequencing. Oncol Rep. 2003. 10:175–179.
9. Iwasawa A, Nieminen P, Lehtinen M, Paavonen J. Human papillomavirus DNA in uterine cervix squamous cell carcinoma and adenocarcinoma detected by polymerase chain reaction. Cancer. 1996. 77:2275–2279.
10. Schellekens MC, Dijkman A, Aziz MF, Siregar B, Cornain S, Kolkman-Uljee S, et al. Prevalence of single and multiple HPV types in cervical carcinomas in Jakarta, Indonesia. Gynecol Oncol. 2004. 93:49–53.
11. Tase T, Okagaki T, Clark BA, Manias DA, Ostrow RS, Twiggs LB, et al. Human papillomavirus types and localization in adenocarcinoma and adenosquamous carcinoma of the uterine cervix: a study by in situ DNA hybridization. Cancer Res. 1988. 48:993–998.
12. Tase T, Sato S, Wada Y, Yajima A, Okagaki T. Prevalence of human papillomavirus type 18 DNA in adenocarcinoma and adenosquamous carcinoma of the uterine cervix occurring in Japan. Tohoku J Exp Med. 1988. 156:47–53.
13. Teshima H, Beaudenon S, Koi S, Katase K, Hasumi K, Masubuchi K, et al. Human papillomavirus type 18 DNA sequences in adenocarcinoma and adenosquamous carcinoma of the uterine cervix. Arch Gynecol Obstet. 1997. 259:169–177.
14. Uchiyama M, Iwasaka T, Matsuo N, Hachisuga T, Mori M, Sugimori H. Correlation between human papillomavirus positivity and p53 gene overexpression in adenocarcinoma of the uterine cervix. Gynecol Oncol. 1997. 65:23–29.
15. Yamakawa Y, Forslund O, Teshima H, Hasumi K, Kitagawa T, Hansson BG. Human papillomavirus DNA in adenocarcinoma and adenosquamous carcinoma of the uterine cervix detected by polymerase chain reaction (PCR). Gynecol Oncol. 1994. 53:190–195.
16. Yoshida T, Sano T, Oyama T, Kanuma T, Fukuda T. Prevalence, viral load, and physical status of HPV 16 and 18 in cervical adenosquamous carcinoma. Virchows Arch. 2009. 455:253–259.
17. Reimers LL, Anderson WF, Rosenberg PS, Henson DE, Castle PE. Etiologic heterogeneity for cervical carcinoma by histopathologic type, using comparative age-period-cohort models. Cancer Epidemiol Biomarkers Prev. 2009. 18:792–800.
18. Saint-Paul MT, Brémond A, Rochet Y. Cervical cancer before 35 years of age: epidemiological and prognostic aspects. Retrospective study of 46 cases of cervical cancer before 35 years of age in a series of 449 cases in stages IA2 and IV. J Gynecol Obstet Biol Reprod (Paris). 1993. 22:737–742.
19. Barnes W, Delgado G, Kurman RJ, Petrilli ES, Smith DM, Ahmed S, et al. Possible prognostic significance of human papillomavirus type in cervical cancer. Gynecol Oncol. 1988. 29:267–273.
20. Ogura K, Ishi K, Matsumoto T, Kina K, Nojima M, Suda K. Human papillomavirus localization in cervical adenocarcinoma and adenosquamous carcinoma using in situ polymerase chain reaction: review of the literature of human papillomavirus detection in these carcinomas. Pathol Int. 2006. 56:301–308.
21. Lee MF, Chang MC, Wu CH. Detection of human papillomavirus types in cervical adenocarcinoma by the polymerase chain reaction. Int J Gynaecol Obstet. 1998. 63:265–270.
22. Liebrich C, Brummer O, Von Wasielewski R, Wegener G, Meijer C, Iftner T, et al. Primary cervical cancer truly negative for high-risk human papillomavirus is a rare but distinct entity that can affect virgins and young adolescents. Eur J Gynaecol Oncol. 2009. 30:45–48.
23. Botezatu A, Socolov D, Goia CD, Iancu IV, Ungureanu C, Huica I, et al. The relationship between HPV16 and HPV 18 viral load and cervical lesions progression. Roum Arch Microbiol Immunol. 2009. 68:175–182.
24. Castellsague X, Diaz M, de Sanjose S, Munoz N, Herrero R, Franceschi S, et al. Worldwide human papillomavirus etiology of cervical adenocarcinoma and its cofactors: implications for screening and prevention. J Natl Cancer Inst. 2006. 98:303–315.
25. Hildesheim A, Berrington de Gonzalez A. Etiology and prevention of cervical adenocarcinomas. J Natl Cancer Inst. 2006. 98:292–293.
26. Wheeler CM, Hunt WC, Joste NE, Key CR, Quint WG, Castle PE. Human papillomavirus genotype distributions: implications for vaccination and cancer screening in the United States. J Natl Cancer Inst. 2009. 101:475–487.
27. Eifel PJ, Burke TW, Delclos L, Wharton JT, Oswald MJ. Early stage I adenocarcinoma of the uterine cervix: treatment results in patients with tumors less than or equal to 4 cm in diameter. Gynecol Oncol. 1991. 41:199–205.
28. Eifel PJ, Burke TW, Morris M, Smith TL. Adenocarcinoma as an independent risk factor for disease recurrence in patients with stage IB cervical carcinoma. Gynecol Oncol. 1995. 59:38–44.
29. Eifel PJ, Morris M, Oswald MJ, Wharton JT, Delclos L. Adenocarcinoma of the uterine cervix: prognosis and patterns of failure in 367 cases. Cancer. 1990. 65:2507–2514.
30. Kjorstad KE, Bond B. Stage IB adenocarcinoma of the cervix: metastatic potential and patterns of dissemination. Am J Obstet Gynecol. 1984. 150:297–299.
31. Kosary CL. FIGO stage, histology, histologic grade, age and race as prognostic factors in determining survival for cancers of the female gynecological system: an analysis of 1973-87 SEER cases of cancers of the endometrium, cervix, ovary, vulva, and vagina. Semin Surg Oncol. 1994. 10:31–46.
32. Lea JS, Sheets EE, Wenham RM, Duska LR, Coleman RL, Miller DS, et al. Stage IIB-IVB cervical adenocarcinoma: prognostic factors and survival. Gynecol Oncol. 2002. 84:115–119.
33. Matthews CM, Burke TW, Tornos C, Eifel PJ, Atkinson EN, Stringer CA, et al. Stage I cervical adenocarcinoma: prognostic evaluation of surgically treated patients. Gynecol Oncol. 1993. 49:19–23.
34. Nakanishi T, Ishikawa H, Suzuki Y, Inoue T, Nakamura S, Kuzuya K. A comparison of prognoses of pathologic stage Ib adenocarcinoma and squamous cell carcinoma of the uterine cervix. Gynecol Oncol. 2000. 79:289–293.
35. Reagan JW, Fu YS. Histologic types and prognosis of cancers of the uterine cervix. Int J Radiat Oncol Biol Phys. 1979. 5:1015–1020.
36. Recoules-Arche A, Rouzier R, Rey A, Villefranque V, Haie-Meder C, Pautier P, et al. Does adenocarcinoma of uterine cervix have a worse prognosis than squamous carcinoma? Gynecol Obstet Fertil. 2004. 32:116–121.
37. Samlal RA, van der Velden J, Ten Kate FJ, Schilthuis MS, Hart AA, Lammes FB. Surgical pathologic factors that predict recurrence in stage IB and IIA cervical carcinoma patients with negative pelvic lymph nodes. Cancer. 1997. 80:1234–1240.
38. Farley JH, Hickey KW, Carlson JW, Rose GS, Kost ER, Harrison TA. Adenosquamous histology predicts a poor outcome for patients with advanced-stage, but not early-stage, cervical carcinoma. Cancer. 2003. 97:2196–2202.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download