Abstract
Objective
To evaluate the clinicopathologic characteristics and prognostic factors of ovarian granulosa cell tumors.
Methods
Medical records of 113 patients presenting between January 1995 and December 2007 were retrospectively reviewed.
Results
One-hundred two patients had adult type disease, with a mean age of 46.2 years (range, 18 to 83 years) and a mean follow-up period of 54.7 months (range, 1 to 155 months). The distribution of FIGO stages was 86 patients at stage I, 11 at stage II, and 5 at stage III. During follow-up, ten patients recurred at a mean time of 48 months (range, 4 to 109 months). Among them, three patients died after a mean of 57 months (range, 25 to 103 months). In recurrence analysis, advanced stage (p=0.032) and presence of residual disease (p=0.012) were statistically significant, and age<40 years, premenopause and positive washing cytology were marginally significant (p<0.1). In multivariate analysis, stage was the only factor associated with recurrence; adjuvant chemotherapy and fertility-sparing surgery were not statistically significant. Among 36 patients with fertility-sparing operations, eight patients had nine pregnancies and delivered seven babies. Eleven patients had juvenile type tumors; the mean age was 20.0 years (range, 8 to 45 years) and the mean follow-up period was 69.8 months (range, 20 to 156 months). The distribution of FIGO stage was nine patients at stage I and two at stage III. There were no recurrences or deaths reported. Four patients had seven pregnancies and delivered six babies.
Granulosa cell tumors of the ovary (GCTs), first described by Rokitansky [1], are rare malignancies that account for approximately 3-5% of ovarian tumors [2,3]. There are two distinct histological types - adult GCT (AGCT) and juvenile GCT (JGCT). AGCTs are more common and are usually seen in perimenopausal and postmenopausal women, with a peak incidence at 50-55 years. JGCTs are rare tumors, representing 5% of all GCTs and occurring in premenarchal girls and young women [4].
Because these tumors are rare and recur 5 to 30 years after initial diagnosis [5], there are few studies on the prognostic factors for AGCT and JGCT with an adequate number of patients and a sufficiently long follow-up period. The aims of this study are to evaluate the clinicopathologic characteristics of GCT and to determine the prognostic factors affecting the disease-free interval.
Between 1995 and 2007, 113 new diagnoses of GCT were made across five hospitals; 102 patients were diagnosed with AGCT and 11 patients were diagnosed with JGCT. Data was retrospectively collected from medical records, including patient characteristics, clinical presentation, pathologic reports, extent of surgery, postoperative adjuvant therapy, recurrence, and follow-up status. The disease-free interval was defined as the time from the date of initial operation to the date of recurrence or the date of the final follow-up.
Statistical analysis was performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). The Kaplan-Meier method was used to assess the disease-free interval, and multivariate analyses were performed using the Cox regression model. A p-value of <0.05 was considered to be statistically significant.
One-hundred two patients (90.3%) were diagnosed with AGCTs; clinicopathologic characteristics and treatment methods are summarized in Tables 1 and 2. Age at diagnosis ranged from 24 to 83 years, with a mean age of 47.1 years. The peak incidence was in the fifth decade, and 60 patients (58.8%) were postmenopausal. The mean gravity and parity were 3.5 and 2.3, respectively. Vaginal bleeding (28.4%) and palpable abdominal mass (28.4%) were the most common presenting symptoms, followed by abdominal pain (17.6%), amenorrhea (3.9%), and other symptoms (2.9%). Only 23 patients (22.5%) were asymptomatic. The mean tumor diameter was 9.7 cm (range, 3 to 24 cm). The tumors were right-sided in 52 patients (55.9%), left-sided in 48 patients (47.1%), and bilateral in two patients (2.0%). Preoperative CA-125 was checked in 76 patients, with only ten patients (9.8%) having an elevated level (>35 IU/mL). Endometrial evaluation was available in 68 patients (66.7%); results included ten (9.8%) cases of simple hyperplasia without atypia, one (1.1%) case of simple hyperplasia with atypia, two (2.0%) cases of complex hyperplasia without atypia, three (2.9%) cases of complex hyperplasia with atypia, and two (2.0%) cases of endometrial cancer. Eighteen patients (17.6%) had endometrial abnormalities, and one patient with endometrial cancer died due to recurrence.
All patients underwent surgical procedures. Ascites was present in 19 patients (18.6%), and six patients (5.9%) were cancer cell-positive. Peritoneal cytologies including ascites or washings were available in 57 patients (55.9%), and 12 patients (11.8%) showed positive for cancer cells. Preoperative rupture was seen in 18 patients (17.6%), with 16 cases (15.7%) of rupture occurring during surgery. Capsule invasion was seen in ten patients (9.8%). For the treatment of the primary tumor, 37 patients (36.3%) underwent a staging operation, 29 (28.4%) underwent hysterectomy and bilateral salpingo-oophorectomy, 27 (26.5%) underwent unilateral salpingo-oophorectomy, six (5.9%) underwent unilateral salpingo-oophorectomy including a staging operation, and three (2.9%) underwent cystectomy. The distribution of staging was 86 (843.3%) at stage I, 11 (10.8%) at stage II, five (4.9%) at stage III, and none at stage IV. Complete resection was performed in 100 patients (98.0%), whereas two patients (2.0%) underwent incomplete resection (with about 95% percent of the tumor removed).
Postoperative chemotherapy was administered in 31 patients (30.4%). The regimens included bleomycin, etoposide, and cisplatin (BEP) in 24 patients; cyclophosphamide, adriamycin, and cisplatin (CAP) in five patients; vincristine, bleomycin, and cisplatin (VBP) in one patient; and cyclophosphamide, pirarubicin, and cisplatin in one patient.
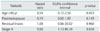
The mean follow-up period was 54.7 months (range, 1 to 155 months). Recurrence was observed in ten patients (9.8%), and the mean time from initial surgery to recurrence was 48 months (range, 4 to 92 months). In recurrence analysis, advanced stage (p=0.032) and presence of residual disease (p=0.012) were statistically significant, while age<40 years, premenopause, and positive washing cytology were marginally significant (p<0.1). Tumor size, bilateral tumors, capsule invasion, ascites, tumor rupture, operation type, postoperative chemotherapy, and elevated CA-125 were not associated with recurrence (Tables 3 and 4). In multivariate analysis, stage was the only factor associated with recurrence (Table 5). Recurrence rates associated with stage were 8.1% (7/86) in stage I, 9.1% (1/11) in stage II, and 40.0% (2/5) in stage III. During the follow-up period, three patients died of disease at a mean time of 69 months (range, 42 to 103 months), two patients had stage III disease and one patient had stage II disease.
Of the 36 patients (35.3%) receiving a fertility-sparing operation, eight patients had a total of nine pregnancies. All patients had stage I disease, with the exception of one patient with stage II disease. Six patients delivered seven healthy babies at term; one patient was lost to follow-up at 10+4 weeks. The last patient delivered one healthy baby and recurred at the second pregnancy, so she underwent hysterectomy with a staging operation.
JGCT was diagnosed in 11 patients (9.7% of GCTs). Clinicopathologic characteristics and treatment methods are summarized in Table 6. The mean age was 20.0 years (range, 8 to 45 years), although more than half of the patients were diagnosed prior to the age of 20, and five patients (45.5%) were premenarchal. With the exception of one, all patients had symptoms. The most common symptom was abdominal mass (45.5%), while three patients presented with vaginal bleeding (27.3%) and two patients presented with abdominal pain (28.3%). The mean tumor diameter was 12.4 cm (range, 5 to 26 cm), and all tumors were unilateral (right-sided in seven patients [63.6%] and left-sided in four [50.0%]). Preoperative CA-125 was measured in ten patients, with only five patients (45.5%) having elevated levels (>35 IU/mL).
All patients initially underwent surgical treatment. Surgery included unilateral salpingo-oophorectomy with a staging operation in six patients (54.5%), unilateral salpingo-oophorectomy in three patients (27.3%), hysterectomy and bilateral salpingo-oophorectomy in one patient (9.1%), and cystectomy in one patient (9.1%). Ascites were present in three patients (27.3%); no ascites or cytology washes were cancer-cell positive. Tumor rupture occurred during surgery in three patients (27.3%), although capsule invasion was not seen in any of the patients. No patients had residual lesions. Nine patients (81.8%) had stage I disease, and two patients (18.2%) had stage III disease. Three patients (32.3%) received adjuvant chemotherapy with BEP.
The mean follow-up period was 69.8 months (range, 20 to 156 months), and there were no recurrences or deaths. During the follow-up period, four patients had a total of seven pregnancies, including six normal deliveries at term and one cornual pregnancy.
Compared to epithelial ovarian cancers, GCTs have different biology and clinical presentation due to their retained ability to produce estrogen [6]. Estrogen production results in menstruation problems and leads to early presentation; as such, these tumors are detected 80-90% of the time in stage I [3,7]. In our study, 36 patients (31.9%) presented with menstrual symptoms such as vaginal bleeding or amenorrhea, and only 24 patients (21.2%) were symptom-free. Ninety-five patients (84.1%) had stage I disease, and only seven patients (6.2%) had stage III disease. Also, estrogen production may result in endometrial abnormalities; according to the literature, the incidence of endometrial carcinoma ranges from 3-22%, and that of endometrial hyperplasia ranges from 32-85% [8]. In our study of AGCTs, 16 patients had endometrial hyperplasia and two had endometrial carcinoma. Therefore, efforts to identify associated endometrial abnormalities are required.
There has been some controversy in the detection of prognostic factors; however, stage is accepted as the most important prognostic factor in most studies. Published ten-year survival rates are 84-95% in stage I, 50-65% in stage II, and 17-33% in stages III-IV in studies with long follow-up periods [9,10]. Similarly, we found that stage was the only factor affecting recurrence in univariate and multivariate analyses. The five-year disease-free survival rates were 92% for stage I, 89% for stage II, and 50% for stage III.
The effect of age on prognosis has been controversial. Chan et al. [11] found that age less than 50 years was an independent prognostic factor for improved survival (hazard ratio [HR], 0.217; 95% confidence interval [CI], 0.067 to 0.706), and Zhang et al. [12] also demonstrated that women under the age of 50 years had a 10% survival advantage in a series of 376 women. However, Ayhan et al. [13] reported that patients aged 60 years and younger had longer survival times (154.5 vs. 89.2 months, p=0.015) and experienced less mortality (4.9% vs. 21.1%, p=0.05), but age was not found to be a significant prognostic factor in multivariate analysis. In contrast to previous studies, age less than 40 years was associated with a high recurrence rate in our study. The five-year and ten-year disease-free survival rates were 82% and 48% for patients ages 40 years and under, and were 93% and 84% for patients older than 40 years, although the difference between the groups was only marginally significant (p=0.068). Postmenopausal women also had significantly lower recurrence rates than premenopausal women (p=0.051).
Tumor size is another factor that has been controversial, with some studies having reported that tumor size is an important prognostic factor [7,11]. Miller et al. [14] found that 33% of patients with recurrence and 13% of patients without recurrence had tumors larger than 15 cm, and recurrent patients had significantly larger tumors (13.5 cm vs. 10 cm; p=0.029). Other studies were unable to validate the prognostic significance of tumor size [5,12,15]. There were no differences in recurrence and survival based on tumor size (with a cutoff of 10 cm) in our study.
As is the case in epithelial ovarian carcinoma, postoperative residual lesions have been suggested as an important factor in AGCTs. Al-Badawi et al. [16] reported on 55 patients with GCT of stage IC or greater. All patients with gross residual disease (>2 cm) were dead within four years, and the only statistically significant factor affecting survival was the presence of macroscopic residual disease (82% vs. 22%). A recent study also found that absence of residual disease was an independent predictor for improved survival (HR, 0.162; 95% CI, 0.043 to 0.610) [11]. In our study, patients with residual lesions had a lower recurrence rate than that of patients without (50.0% vs. 9%, p=0.012), but this difference was not significant in multivariate analysis.
In our study, we evaluated prognostic factors that had not been reported in previous studies. Positive cytology (p=0.099) was marginally significant, but bilateral disease, ascites, tumor rupture, and capsule invasion were not associated with differences in recurrence rates. However, there have been few studies focusing on these factors. In one study, 25-year survival rates were 86% in intact stage I patients and 60% in patients with ruptured tumors [15]. Further studies with more patients are required to demonstrate these results.
Although many chemotherapy regimens have been used in ovarian carcinoma, the relatively low incidence and late recurrence of GCT leads to difficulty in forming a consensus. In addition, there is no evidence that postoperative adjuvant chemotherapy prevents recurrence [16-18]. Our study also showed that patients who received postoperative chemotherapy had a high recurrence rate and a low survival rate. This result may be due to the high incidence of adjuvant chemotherapy in patients with advanced stages. However, Homesley et al. [19] have reported the efficacy of BEP in incompletely resected stages II-IV or recurrent disease in a GOG study. Thirty-seven percent (14/38) of these patients had negative findings on second-look laparotomy, and six complete responders had a long median duration (24.4 months). Further, Schumer and Cannistra [20] reported that the clinical significance of postoperative adjuvant chemotherapy for high-risk patients has not been demonstrated through prospective randomized trials, but that the use of adjuvant chemotherapy and radiation therapy have sometimes been associated with prolonged disease-free survival in high-risk patients.
Surgery is the initial treatment for ovarian carcinoma. However, the extent of the surgical procedure is controversial, particularly in JGCT, which presents at a younger age and therefore makes fertility-sparing surgery an important issue. Pautier et al. [8] reported that nine patients with stage IA tumors and who had undergone radical surgery had no relapses, but relapse was observed in three of the six patients with stage IA tumors who were treated with conservative surgery. Busby and Anderson [21] and Evans et al. [22] also found a high relapse rate and a low survival rate associated with conservative surgery. However, Norris and Taylor [23] and Novak et al. [24] reported no differences in relapse rates between conservative and radical surgeries for stage IA patients. In a recent study, Zhang et al. [12] reported on 132 patients 50 years of age or younger and who had stage I disease, of which 61 (46%) underwent standard surgical treatment (including hysterectomy) and 71 (54%) had a uterine-sparing procedure. The five-year survival rates of these respective women were 97% and 98%. In our study, 36 patients (35.3%) underwent fertility-sparing surgery, and they exhibited no statistically significant difference in recurrence or survival compared with those having undergone non-fertility-sparing surgery. In this study, eight patients experienced a total of nine pregnancies, and one patient had stage II disease. Considering the fact that AGCT has a good survival rate and a late recurrence pattern, fertility-sparing surgery is an option for women with stage I or II ovarian carcinoma who wish to retain fertility. Colombo et al. [25] concluded that fertility-sparing surgery is a reasonable approach if the disease is limited to one ovary.
JGCTs are also rare, constituting less than 5% of ovarian tumors in children and adolescents. About 90% of patients are diagnosed at stage I and have a good prognosis [26]. There are reports of advanced-stage tumors successfully treated with platinum-based chemotherapy [19,20]. Schneider et al. [27] published a prospective study of 54 ovarian sex cord-stromal tumors in children and adolescents, including 45 JGCTs. They determined that chemotherapy should be used in stage IC tumors with preoperative rupture or malignant ascites, especially those tumors with high mitotic activity. Cisplatin-based chemotherapy seems to be effective for the treatment of advanced-stage tumors. In our study, we used adjuvant chemotherapy in two patients with stage III disease, and no recurrence was detected. Of the two patients with stage IC disease, one received adjuvant chemotherapy and one did not; neither experienced recurrence.
This study has some weaknesses. First, it is a retrospective study. However, due to the rarity and characteristics of these tumors, it would be not be possible to execute a prospective study. We were able to determine the prognostic factors affecting disease-free survival after reviewing the medical records from five hospitals. Second, several hospitals were involved, and each institution had some degree of difference in patient management. Currently, there is no consensus on the management of these tumors, and the data from this and other studies can be used to develop consensus guidelines.
This study also has several strengths. First, it is the first multicenter study of GCTs in Korea. It is difficult to detect the statistical significance of these tumors based only on the small number of cases from a single institution. Second, some studies on GCTs have been performed; however, there are only a few studies regarding pathologic and operative findings, such as ascites, cytology, tumor rupture, capsule invasion, and bilaterality. Third, we reported not only on AGCTs but also on the less-common JGCTs and their pregnancy results.
In conclusion, our results show that most AGCTs are detected in the early stages and have excellent survival outcomes. Stage is the only prognostic factor predicting recurrence; additional studies about age, menopause, postoperative residual lesions, and positive washing cytology are required. The recurrence rate observed was not high, but the interval from initial surgery to recurrence was relatively long, thus requiring long-term follow-up. Furthermore, for women with early-stage AGCT who want to retain fertility, fertility-sparing surgery with or without chemotherapy is a reasonable treatment option that does not compromise survival. Our studies of JGCTs demonstrate that prognosis is good, and the same management methods can be addressed, although small in numbers. In the future, a prospective multicenter study with uniform protocols may be necessary to confirm these results and to study additional factors.
Figures and Tables
ACKNOWLEDGMENTS
This study was supported by Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education, Science and Technology (2010-0016732).
References
1. Rokitansky CV. Uber abnormalitiaten des corpus luteum. Allg Wien Med Z. 1859. 4:253–258.
2. Kent SW, McKay DG. Primary cancer of the ovary an analysis of 349 cases. Am J Obstet Gynecol. 1960. 80:430–438.
3. Schweppe KW, Beller FK. Clinical data of granulosa cell tumors. J Cancer Res Clin Oncol. 1982. 104:161–169.
4. Calaminus G, Wessalowski R, Harms D, Gobel U. Juvenile granulosa cell tumors of the ovary in children and adolescents: results from 33 patients registered in a prospective cooperative study. Gynecol Oncol. 1997. 65:447–452.
5. Malmstrom H, Hogberg T, Risberg B, Simonsen E. Granulosa cell tumors of the ovary: prognostic factors and outcome. Gynecol Oncol. 1994. 52:50–55.
6. McNatty KP, Makris A, DeGrazia C, Osathanondh R, Ryan KJ. The production of progesterone, androgens, and estrogens by granulosa cells, thecal tissue, and stromal tissue from human ovaries in vitro. J Clin Endocrinol Metab. 1979. 49:687–699.
7. Fox H, Agrawal K, Langley FA. A clinicopathologic study of 92 cases of granulosa cell tumor of the ovary with special reference to the factors influencing prognosis. Cancer. 1975. 35:231–241.
8. Pautier P, Lhomme C, Culine S, Duvillard P, Michel G, Bidart JM, et al. Adult granulosa-cell tumor of the ovary: a retrospective study of 45 cases. Int J Gynecol Cancer. 1997. 7:58–65.
9. Pankratz E, Boyes DA, White GW, Galliford BW, Fairey RN, Benedet JL. Granulosa cell tumors: a clinical review of 61 cases. Obstet Gynecol. 1978. 52:718–723.
10. Schwartz PE, Smith JP. Treatment of ovarian stromal tumors. Am J Obstet Gynecol. 1976. 125:402–411.
11. Chan JK, Zhang M, Kaleb V, Loizzi V, Benjamin J, Vasilev S, et al. Prognostic factors responsible for survival in sex cord stromal tumors of the ovary: a multivariate analysis. Gynecol Oncol. 2005. 96:204–209.
12. Zhang M, Cheung MK, Shin JY, Kapp DS, Husain A, Teng NN, et al. Prognostic factors responsible for survival in sex cord stromal tumors of the ovary: an analysis of 376 women. Gynecol Oncol. 2007. 104:396–400.
13. Ayhan A, Salman MC, Velipasaoglu M, Sakinci M, Yuce K. Prognostic factors in adult granulosa cell tumors of the ovary: a retrospective analysis of 80 cases. J Gynecol Oncol. 2009. 20:158–163.
14. Miller BE, Barron BA, Wan JY, Delmore JE, Silva EG, Gershenson DM. Prognostic factors in adult granulosa cell tumor of the ovary. Cancer. 1997. 79:1951–1955.
15. Bjorkholm E, Silfversward C. Prognostic factors in granulosa-cell tumors. Gynecol Oncol. 1981. 11:261–274.
16. Al-Badawi IA, Brasher PM, Ghatage P, Nation JG, Schepansky A, Stuart GC. Postoperative chemotherapy in advanced ovarian granulosa cell tumors. Int J Gynecol Cancer. 2002. 12:119–123.
17. Gershenson DM, Copeland LJ, Kavanagh JJ, Stringer CA, Saul PB, Wharton JT. Treatment of metastatic stromal tumors of the ovary with cisplatin, doxorubicin, and cyclophosphamide. Obstet Gynecol. 1987. 70:765–769.
18. Uygun K, Aydiner A, Saip P, Kocak Z, Basaran M, Dincer M, et al. Clinical parameters and treatment results in recurrent granulosa cell tumor of the ovary. Gynecol Oncol. 2003. 88:400–403.
19. Homesley HD, Bundy BN, Hurteau JA, Roth LM. Bleomycin, etoposide, and cisplatin combination therapy of ovarian granulosa cell tumors and other stromal malignancies: a Gynecologic Oncology Group study. Gynecol Oncol. 1999. 72:131–137.
20. Schumer ST, Cannistra SA. Granulosa cell tumor of the ovary. J Clin Oncol. 2003. 21:1180–1189.
21. Busby T, Anderson GW. Feminizing mesenchymomas of the ovary: includes 107 cases of granulosa-, granulosa-theca-cell, and theca-cell tumors. Am J Obstet Gynecol. 1954. 68:1391–1320.
22. Evans AT 3rd, Gaffey TA, Malkasian GD Jr, Annegers JF. Clinicopathologic review of 118 granulosa and 82 theca cell tumors. Obstet Gynecol. 1980. 55:231–238.
23. Norris HJ, Taylor HB. Prognosis of granulosa-theca tumors of the ovary. Cancer. 1968. 21:255–263.
24. Novak ER, Kutchmeshgi J, Mupas RS, Woodruff JD. Feminizing gonadal stromal tumors. Analysis of the granulosa-theca cell tumors of the Ovarian Tumor Registry. Obstet Gynecol. 1971. 38:701–713.
25. Colombo N, Parma G, Zanagnolo V, Insinga A. Management of ovarian stromal cell tumors. J Clin Oncol. 2007. 25:2944–2951.
26. Powell JL, Otis CN. Management of advanced juvenile granulosa cell tumor of the ovary. Gynecol Oncol. 1997. 64:282–284.
27. Schneider DT, Calaminus G, Wessalowski R, Pathmanathan R, Selle B, Sternschulte W, et al. Ovarian sex cord-stromal tumors in children and adolescents. J Clin Oncol. 2003. 21:2357–2363.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download