Abstract
Objective
This study examined the risk factors for preterm birth and the efficacy of prophylactic cerclage in patients who had undergone cervical conization due to cervical intraepithelial neoplasia before pregnancy.
Methods
We reviewed the medical records of all patients who gave live singleton births between May 1996 and April 2009, after having cervical conization. Delivery before 37 gestational weeks was considered as preterm birth. The pregnancy outcomes were analyzed with independent sample t-test, chi-square test, and multiple logistic regression using the SPSS ver. 12.0.
Results
Sixty five cases were found. The mean gestational age at delivery was 37 weeks (SD, 3.5). Eighteen patients (27.7%) had preterm delivery. The type of conization, the volume of the specimen, and second trimester cervical length were related to preterm birth (p≤0.001, p=0.019, p≤0.001, respectively). In multivariate analysis, only mid-trimester cervical length was statistically significant for preterm birth (p=0.012; odds ratio, 0.194; confidence interval, 0.055 to 0.693). Six out of 65 patients had undergone prophylactic cerclage, and three (50%) of them had preterm births, while 15 (25%) patients without cerclage had preterm births.
Conclusion
The type of conization, the volume of specimen, and second trimester cervical length may be the risk factors for preterm birth in patients who have a prior history of cervical conization. Prophylactic cerclage may not be helpful in preventing preterm birth, therefore more careful consideration should be paid in deciding cerclage after conization during prenatal counseling.
The incidence of abnormal cervical cytology is rising; especially among women of reproductive age.1,2 Consequently, we can expect a higher percentage of pregnancies with a previous conization than before. To treat cervical intraepithelial neoplasia (CIN), various procedures including conization, cryotherapy, laser, and loop electrosurgical excision procedure (LEEP) have been used.3 Among them, LEEP has become the most widely used method. LEEP is cheaper, does not require general anesthesia or an operating room facility, and is an office- based procedure that is therefore more convenient for both the physician and the patient than cold knife conization.4,5 Although it is still controversial, conization of the cervix for the treatment of CIN is known to be related with adverse pregnancy outcomes in subsequent pregnancies, including preterm delivery, low birth weight infants, incompetent cervix, and cervical stenosis.6-12
Most of all, preterm birth is the most notable complication because it can be a major cause of perinatal morbidity and mortality. In particular, infants who are born at earlier gestational ages are at the greatest risk of illness, injury, and handicap.13 The rate of preterm birth is generally increasing despite improvements in perinatal care over the past two decades.14 Regarding the risk factors of preterm birth in patients with prior conization, many factors have been suggested, including cervical length, specimen volume, and the interval between LEEP procedure and delivery.9,12,15 As for the need for prophylactic cerclage, controversy still exists.9
Therefore, in this study, we investigated the risk factors for preterm birth and the efficacy of prophylactic cerclage in pregnant women who had undergone cervical conization due to cervical intraepithelial lesions prior to the pregnancy.
We retrospectively reviewed the medical records of all patients who gave live singleton births at Yonsei University Health System in Seoul, Korea, between May 1996 and April 2009, who had received cervical conization. We documented the mothers' age, parity, prior medico-surgical and obstetric history, gestational age at delivery, interval between conization and delivery, times and type of conization, mid-trimester cervical length, the volumes of conization specimen, and cerclage data. Delivery before 37 gestational weeks was considered as a preterm birth. The types of conization include LEEP and cold knife conization. The mid-trimester cervical length was measured by ultrasonography between 14 to 28 gestational weeks based on previous studies.16-18 Cervical length less than 2.5 cm was considered to be short.16,19 Each conization specimen consisted of 1 to 3 fragments. The volumes of the conization specimen were the sum of all fragments from the pathology report. Only the first subsequent pregnancies were included in this study. The study was approved by the institutional review board. The pregnancy outcomes were analyzed with independent sample t-test, chi-square test, and multiple logistic regression using the SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). A probability value of p≤0.05 was considered significant.
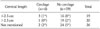
Sixty five cases were found in the medical records. Among them, 18 patients (27.7%) delivered before term (less than 37 gestational weeks), and 47 patients (72.3%) delivered at term. The overall mean gestational age at delivery was 37 weeks (SD, 3.5), and the overall mean interval between conization and delivery was 20.5 months (SD, 12.5). The mean volume of the specimen was 6.0 cm3 (SD, 3.5), and the mean mid-trimester cervical length was 2.4 cm (SD, 0.9). Fifty five patients had a conization once, and 10 had two conizations before the pregnancy. Fifty one received LEEP and 14 received cold knife conizations. In univariate analysis, the type of conization, volume of specimen, and second trimester cervical length were related with preterm birth (p≤0.001, p=0.019, p≤0.001, respectively), but age, parity, a prior history of preterm birth, and the interval between cervical conization and delivery and the times of cervical conization were not associated with preterm birth (Table 1). However, in multivariate analysis, only mid-trimester cervical length was statistically significant for preterm birth (p=0.012; odd ratio [OR], 0.194; confidence interval [CI], 0.055 to 0.693) while the specimen volume showed a weak association (p=0.062; OR, 1.383; CI, 0.984 to1.944) (Table 2).
Only six out of 65 patients had undergone prophylactic cerclage. All of them received the McDonald's operation. Two were not performed in our institute. Three (50%) out of six patients with cerclage had preterm deliveries, while only 15 (25%) patients without cerclage had preterm births (Table 3).
Mid-trimester cervical length was measured in 39 patients only. The cervical length was short (length less than 2.5 cm) in 19 patients. Only three of them (15.8%) had cerclage. Seven (25.9%) had preterm deliveries among patients whose cervical length was not checked (Table 4).
Cervical cancer is still the most common malignancy affecting Korean women, but the mortality rate has declined with the efforts to detect precancerous lesions earlier using cervical cytology and colposcopy.20 As the most prevalent age is in the 30's, the need for conservative treatment is rising.21 Since the introduction of cervical conization in the late 1950's, many studies on cervical conization and pregnancy outcomes have been published. In particular, many studies have emphasized on the relationship between conization and preterm birth.7,14,22-26 Even though some authors found no relationship,22,27 many authors have agreed on the significant correlation between cervical conization and preterm delivery.7,14,23-26 They suggested various associated factors including short cervical length,28-30 size of the specimen removed,9,12,31,32 the time interval between conization and delivery,4,15,33 and type of conization.34
In this study, the results showed that the type of conization, the volume of specimen, and second trimester cervical length were related to preterm birth in univariate analysis, and in multiple regression analysis, second trimester cervical length was found to influence the gestational age at birth.
The results are consistent with previous studies. Michelin et al.34 demonstrated that LEEP was the procedure of choice for the patients who wanted to be pregnant, because more miscarriages and preterm pregnancies occur in conization cases than in LEEP cases.
As for the size of the conization specimen, few studies are available; especially regarding the "volume" rather than the "depth" of conization have been seldom published. Leiman et al.9 suggested that a large cone of more than 4 mL of volume is associated with preterm delivery.
Many studies performed on the cervical length measurement by transvaginal ultrasonography.16,19,28,29,35 They reported that cervical length measurement by transvaginal ultrasonography is an accurate and valid method of measuring the cervix,35 and may be a useful method of predicting who is at risk for preterm delivery.16,19 This hypothesis turned out to be true with postconization patients.28 The cervical length appears to be inversely proportional to the risk of preterm birth.19 Our study strongly supports this result.
Our study also revealed the interval between conization and delivery is inversely proportional to the risk of preterm birth. Many studies demonstrated that the healing process is completed in 3 months after conization.33,36 Himes and Simhan33 suggested that a short conization-to-pregnancy interval, especially shorter than 2-3 months, increases the risk of preterm delivery. The length of the cervix is shortened when measured by ultrasonographic measurement just after conization.15 However, after adequate healing time after LEEP, the length does not remain shortened.4
Not much is known regarding the times of conization. It is interesting that our results showed no statistical significance in preterm delivery with the times of conization. The mean interval between conizations was 4.4 months with the standard deviation of 6.95 months. Gentry's suggestion4 mentioned above also explains this result.
The benefit of prophylactic cerclage in women with a history of conization is not clear.37 Leiman et al.9 concluded that all postcone pregnancies should be regarded as high risk, and recommended cerclage in pregnancies following extensive cone biopsy. In contrast, Kullander and Sjoberg38 concluded that cerclage should be avoided because they were unable to show that it reduces the incidence of preterm delivery in women after conization. Myllynen and Karjalainen39 and Zeisler et al.40 and proposed that prophylactic cerclage should be used more sparingly, because it does not prevent preterm delivery, and tends to induce preterm uterine contractions. They reported that cerclage itself may be a risk factor. Sutures can act as a foreign body and lead to uterine irritability and contractions after a cerclage procedure.41 Moreover, some authors reported a significant increase in pathogenic flora in the vagina and cervix after cerclage.42 They insisted that the release of prostaglandins by bacteria in the vagina may induce chorioamnionitis, preterm premature rupture of membranes, preterm delivery, and sepsis.43 In this study, preterm births occurred in 50% (n=3) of patients after cerclage. The number of patients was too small to compare the efficacy of the cerclage, but cerclage may not be helpful in preventing preterm delivery, and can only add complications following operative procedures. A further study with a large number of patients may be done on the efficacy of cerclage according to the cervical length, the gestational age at delivery, and the indication of cerclage.
In previous studies on pregnancy outcome after conization, most studies have dealt whether there are adverse perinatal outcomes such as preterm birth, low birth weight, or whether conization itself may be a risk factor for preterm birth. We focused on the associated factors for preterm birth, and we integrated all associated factors together rather than as a single factor. There are few studies on the risk factors for preterm birth after conization. We included "volume removed" rather than "depth (or height)" of the specimen that most previous studies have dealt with.
This study contains the largest numbers of Korean patients ever published on this subject, but the sample size is still small. Moreover, as this study was a retrospective cohort study, there may have been confounders not identified or controlled. A further prospective study with a larger sample size is needed.
In conclusion, in patients with a prior history of cervical conization, the type of conization, volume of conization, and second trimester cervical length influence preterm delivery with statistical significance. Thus close observation, especially with the mid-trimester cervical length is needed for the management of such patients. Since the need for prophylactic cerclage remains questionable in this study, we suggest that prudent decision should be made regarding prophylactic cerclage during prenatal counseling.
Figures and Tables
References
1. Crane JM. Pregnancy outcome after loop electrosurgical excision procedure: a systematic review. Obstet Gynecol. 2003. 102:1058–1062.
2. Kainz C, Gitsch G, Heinzl H, Breitenecker G. Incidence of cervical smears indicating dysplasia among Austrian women during the 1980s. Br J Obstet Gynaecol. 1995. 102:541–544.
3. Jolley JA, Wing DA. Pregnancy management after cervical surgery. Curr Opin Obstet Gynecol. 2008. 20:528–533.
4. Gentry DJ, Baggish MS, Brady K, Walsh PM, Hungler MS. The effects of loop excision of the transformation zone on cervical length: implications for pregnancy. Am J Obstet Gynecol. 2000. 182:516–520.
5. Prendiville W. Large loop excision of the transformation zone. Clin Obstet Gynecol. 1995. 38:622–639.
6. Arbyn M, Kyrgiou M, Simoens C, Raifu AO, Koliopoulos G, Martin-Hirsch P, et al. Perinatal mortality and other severe adverse pregnancy outcomes associated with treatment of cervical intraepithelial neoplasia: meta-analysis. BMJ. 2008. 337:a1284.
7. Kristensen J, Langhoff-Roos J, Kristensen FB. Increased risk of preterm birth in women with cervical conization. Obstet Gynecol. 1993. 81:1005–1008.
8. Kyrgiou M, Koliopoulos G, Martin-Hirsch P, Arbyn M, Prendiville W, Paraskevaidis E. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: systematic review and meta-analysis. Lancet. 2006. 367:489–498.
9. Leiman G, Harrison NA, Rubin A. Pregnancy following conization of the cervix: complications related to cone size. Am J Obstet Gynecol. 1980. 136:14–18.
10. Luesley DM, McCrum A, Terry PB, Wade-Evans T, Nicholson HO, Mylotte MJ, et al. Complications of cone biopsy related to the dimensions of the cone and the influence of prior colposcopic assessment. Br J Obstet Gynaecol. 1985. 92:158–164.
11. Moinian M, Andersch B. Does cervix conization increase the risk of complications in subsequent pregnancies? Acta Obstet Gynecol Scand. 1982. 61:101–103.
12. Raio L, Ghezzi F, Di Naro E, Gomez R, Luscher KP. Duration of pregnancy after carbon dioxide laser conization of the cervix: influence of cone height. Obstet Gynecol. 1997. 90:978–982.
13. Jones JM, Sweetnam P, Hibbard BM. The outcome of pregnancy after cone biopsy of the cervix: a case-control study. Br J Obstet Gynaecol. 1979. 86:913–916.
14. Joseph KS, Kramer MS, Marcoux S, Ohlsson A, Wen SW, Allen A, et al. Determinants of preterm birth rates in Canada from 1981 through 1983 and from 1992 through 1994. N Engl J Med. 1998. 339:1434–1439.
15. Ricciotti HA, Burke L, Kobelin M, Slomovic B, Ludmir J. Ultrasound evaluation of cervical shortening after loop excision of the transformation zone (LETZ). Int J Gynaecol Obstet. 1995. 50:175–178.
16. Berghella V. Novel developments on cervical length screening and progesterone for preventing preterm birth. BJOG. 2009. 116:182–187.
17. Berghella V, Talucci M, Desai A. Does transvaginal sonographic measurement of cervical length before 14 weeks predict preterm delivery in high-risk pregnancies? Ultrasound Obstet Gynecol. 2003. 21:140–144.
18. Owen J, Yost N, Berghella V, Thom E, Swain M, Dildy GA 3rd, et al. Mid-trimester endovaginal sonography in women at high risk for spontaneous preterm birth. JAMA. 2001. 286:1340–1348.
19. Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, Das A, et al. The length of the cervix and the risk of spontaneous premature delivery: National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996. 334:567–572.
20. Kim YT. Current status of cervical cancer and HPV infection in Korea. J Gynecol Oncol. 2009. 20:1–7.
21. Herbert A, Smith JA. Cervical intraepithelial neoplasia grade III (CIN III) and invasive cervical carcinoma: the yawning gap revisited and the treatment of risk. Cytopathology. 1999. 10:161–170.
22. Acharya G, Kjeldberg I, Hansen SM, Sorheim N, Jacobsen BK, Maltau JM. Pregnancy outcome after loop electrosurgical excision procedure for the management of cervical intraepithelial neoplasia. Arch Gynecol Obstet. 2005. 272:109–112.
23. Jakobsson M, Gissler M, Paavonen J, Tapper AM. Loop electrosurgical excision procedure and the risk for preterm birth. Obstet Gynecol. 2009. 114:504–510.
24. Jakobsson M, Gissler M, Sainio S, Paavonen J, Tapper AM. Preterm delivery after surgical treatment for cervical intraepithelial neoplasia. Obstet Gynecol. 2007. 109:309–313.
25. Klaritsch P, Reich O, Giuliani A, Tamussino K, Haas J, Winter R. Delivery outcome after cold-knife conization of the uterine cervix. Gynecol Oncol. 2006. 103:604–607.
26. Samson SL, Bentley JR, Fahey TJ, McKay DJ, Gill GH. The effect of loop electrosurgical excision procedure on future pregnancy outcome. Obstet Gynecol. 2005. 105:325–332.
27. Althuisius SM, Schornagel IJ, Dekker GA, van Geijn HP, Hummel P. Loop electrosurgical excision procedure of the cervix and time of delivery in subsequent pregnancy. Int J Gynaecol Obstet. 2001. 72:31–34.
28. Berghella V, Pereira L, Gariepy A, Simonazzi G. Prior cone biopsy: prediction of preterm birth by cervical ultrasound. Am J Obstet Gynecol. 2004. 191:1393–1397.
29. Grimes-Dennis J, Berghella V. Cervical length and prediction of preterm delivery. Curr Opin Obstet Gynecol. 2007. 19:191–195.
30. Masamoto H, Nagai Y, Inamine M, Hirakawa M, Okubo E, Ishisoko A, et al. Outcome of pregnancy after laser conization: implications for infection as a causal link with preterm birth. J Obstet Gynaecol Res. 2008. 34:838–842.
31. Ferenczy A, Choukroun D, Falcone T, Franco E. The effect of cervical loop electrosurgical excision on subsequent pregnancy outcome: North American experience. Am J Obstet Gynecol. 1995. 172:1246–1250.
32. Sadler L, Saftlas A. Cervical surgery and preterm birth. J Perinat Med. 2007. 35:5–9.
33. Himes KP, Simhan HN. Time from cervical conization to pregnancy and preterm birth. Obstet Gynecol. 2007. 109:314–319.
34. Michelin MA, Merino LM, Franco CA, Murta EF. Pregnancy outcome after treatment of cervical intraepithelial neoplasia by the loop electrosurgical excision procedure and cold knife conization. Clin Exp Obstet Gynecol. 2009. 36:17–19.
35. Jackson GM, Ludmir J, Bader TJ. The accuracy of digital examination and ultrasound in the evaluation of cervical length. Obstet Gynecol. 1992. 79:214–218.
36. Wright TC, Kurman RJ, Ferenczy A. Kurman RJ, editor. Precancerous lesions of the cervix. Blaustein's pathology of the female genital tract. 1994. 4th ed. New York: Springer-Verlag;260.
37. Larsson G, Grundsell H, Gullberg B, Svennerud S. Outcome of pregnancy after conization. Acta Obstet Gynecol Scand. 1982. 61:461–466.
38. Kullander S, Sjoberg NO. Treatment of carcinoma in situ of the cervix uteri by conization: a five-year follow-up. Acta Obstet Gynecol Scand. 1971. 50:153–157.
39. Myllynen L, Karjalainen O. Pregnancy outcome after combined amputation and conization of the uterine cervix. Ann Chir Gynaecol. 1984. 73:345–349.
40. Zeisler H, Joura EA, Bancher-Todesca D, Hanzal E, Gitsch G. Prophylactic cerclage in pregnancy: effect in women with a history of conization. J Reprod Med. 1997. 42:390–392.
41. Robichaux AG 3rd, Stedman CM, Hamer C. Uterine activity in patients with cervical cerclage. Obstet Gynecol. 1990. 76:1 Suppl. 63S–66S.
42. Charles D, Edwards WR. Infectious complications of cervical cerclage. Am J Obstet Gynecol. 1981. 141:1065–1071.
43. Jewelewicz R. Incompetent cervix: pathogenesis, diagnosis and treatment. Semin Perinatol. 1991. 15:156–161.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download