Abstract
We report a rare co-occurrence of an adenoma malignum and an adenocarcinoma in a 30-year-old woman with Peutz-Jeghers syndrome. The woman was diagnosed with Peutz-Jeghers syndrome based on an endoscopic biopsy after vaginal bleeding. A pelvic examination and an MRI revealed the co-occurrence of a 4×5 cm protruding adenocarcinoma of FIGO stage Ib2 based on a punch biopsy and a 4.5×5.7 cm multilocular cystic mass above the solid cancer. The patient received two courses of neoadjuvant chemotherapy, followed by a laparoscopic radical hysterectomy with pelvic lymph node dissection. Pathologic findings were consistent with adenocarcinoma (40%) and adenoma malignum (60%) confined to the cervix. Three courses of adjuvant chemotherapy were performed and no clinical evidence of recurrence was seen during a 12 month follow-up period. This study will contribute to defining the best diagnosis and treatment for these rare complicating tumors.
Peutz-Jeghers syndrome (PJS) is a rare autosomal-dominant inherited disorder that is characterized by gastrointestinal hamartomatous polyps and mucocutaneous melanin pigmentation. Patients with this syndrome are at increased risk of developing various neoplasms of the gastrointestinal and extraintestinal organs.1-8 The overall incidence of carcinoma in these patients varies from 20% to 50%, and the cumulative risk of cervical cancer occurring between the ages of 15 to 64 years is 10%.9,10
Adenoma malignum, often referred to as 'minimal deviation adenocarcinoma' is a rare variant type of adenocarcinoma that comprises 1 to 3% of all cervical adenocarcinomas.11 Despite its benign appearance, it can be aggressive and have a poor prognosis.
Most uterine cervical malignancies in PJS are adenoma malignum. Co-occurrence of an adenoma malignum and an adenocarcinoma is rare, and co-occurrence in PJS is extremely rare. In this report, we describe a case of dual uterine cervical cancers in a patient with PJS.
A woman suffering from diffuse abdominal pain was admitted for endoscopic evaluation of the stomach, small intestine, and colon. Endoscopic findings were multiple polypoid masses of the stomach, small intestine, and colon with some mucocutaneous pigmentation. The pathologic report indicated multiple hamartomatous polyps based on samples from multiple polypectomy and mucocutaneous melanin pigmentation. The patient was diagnosed with Peutz-Jeghers syndrome based on endoscopic biopsy results (Fig. 1). For further evaluation, an MRI was performed, and revealed a 4.5×5.7 cm multilocular cystic mass on the uterine cervix (Fig. 2). Physical examination showed a 4×5 cm sized mass protruding from the lower cervical lip with a bulky cervical body, and a negative fornix and parametrium. The protruding cancerous mass was determined to be an adenocarcinoma based on punch biopsy results. The tumor markers SCC, CA-125, and CA 19-9 were within normal ranges. A colonoscopy, intravenous pyelogram, and cystoscopy showed no evidence of metastatic disease. The tumor was classified as FIGO stage Ib2.
Two courses of neoadjuvant chemotherapy following a paclitaxel-carboplatin regimen were administered. After chemotherapy, ultrasonography showed that the multiloculated cystic mass was decreased in size by approximately 34% from 5.3×4.7 cm to 4.8×3.4 cm, while the second protruding cervical mass was decreased in size by approximately 83% from 4×5 cm to 1.7×2.0 cm. The patient underwent a laparoscopic radical hysterectomy with nerve-sparing, bilateral pelvic lymph node dissection, and bilateral para-aortic lymph node sampling. Histopathologic figures were consistent with adenoma malignum and endocervical type adenocarcinoma with moderate differentiation confined to the cervix without any extracervical tumors, such as parametrium invasion or lymph node metastasis (Fig. 3).
Microscopic examination showed that the polypoid growing tumor was a moderately-differentiated endocervical type adenocarcinoma with a distinct desmoplastic stromal reaction. The tumor was located mainly in the squamo-columnar junction and it comprised approximately 40% of the total tumor mass. The other adenocarcinoma was characterized by numerous irregularly-shaped mucinous glands in the more endocervical portion, characteristic of an adenoma malignum. It comprised 60% of the total tumor mass. These two carcinomas were partly admixed in some regions, but relatively well delineated in others. Immunohistochemical findings also indicated the presence of two tumor types. Ki-67 staining showed diffuse proliferation in the endocervical type adenocarcinoma, but focal staining in the adenoma malignum (Fig. 4).
Postoperatively, the patient received three courses of adjuvant chemotherapy following a paclitaxel-carboplatin regimen. There was no clinical evidence of recurrence during a 12 month follow-up period. The patient is currently being followed at our institution.
PJS is now recognized as a cancer predisposition syndrome. The incidence of cancer among PJS patients has been estimated to be 15-fold higher than the incidence of cancer in the general population.9 Genital tract neoplasms have been reported in patients with PJS and include sex cord tumors with annular tubules (SCTAT), the most common ovarian neoplasm, as well as adenoma malignum of the cervix and adenocarcinoma of the endometrium. A total of four cases of PJS with multiple genital tract tumors at different sites have been reported from 1986 to date. Genital tract neoplasms in female PJS patients are, therefore, rare and cases with multiple tumors at different sites are even rarer. Our case of a patient with PJS and dual cervical cancer (adenoma malignum and an adenocarcinoma) is, therefore, very rare.
The prognosis of cervical adenoma malignum is poor as this tumor is highly aggressive. However, at present, no treatment guidelines for this tumor have been proposed. Furthermore, prognosis and treatment guidelines for a co-occurrence of adenoma malignum and an adenocarcinoma in PJS have not been established.
In our case, to reduce the tumor size for laparoscopic operability, we performed two courses of neoadjuvant chemotherapy using paclitaxel-carboplatin. The size of the adenoma malignum, however, was not significantly decreased by the treatment, in contrast to the endocervical type adenocarcinoma. Postoperatively, the patient received three courses of adjuvant chemotherapy following a paclitaxel-carboplatin regimen. There was no clinical evidence of recurrence during a 12 month follow-up period. The patient is currently being monitored closely to evaluate recurrence.
In conclusion, dual presentation of uterine cervical cancer in PJS is rare. Hence, there is no standardized treatment method. More case reports and studies are required to formulate a standardized method of treatment.
Figures and Tables
 | Fig. 1Peutz-Jeghers polyp of the colon. An arborizing smooth muscle core separates colonic glands into vague lobules (×12.5) (A). A band of smooth muscle fibers between lobules of colonic glands can be seen at higher magnification (×40) (B) (H&E). |
 | Fig. 2Enhanced T1-weighted MRI showing septal enhancement of a multiloculated cystic mass (long arrow, adenoma malignum) and enhancement of the solid portion (short arrow, endocervical type adenocarcinoma). |
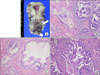 | Fig. 3Histopathologic findings (B-D: H&E, ×200). (A) Gross features showing a large exophytic tumor (short arrow: adenoma malignum) arising from the transformation zone, and a diffuse, bulging mass (long arrow: endocervical type adenocarcinoma) involving the endocervix. (B) The region composed of an adenoma malignum (left) and an endocervical type (right) adenocarcinoma. (C) An adenoma malignum showing irregular glands lined by deceptively bland, mucin rich columnar cells with basal nuclei and occasional mitosis. (D) An endocervical type adenocarcinoma showing cellular stratification, high nuclear atypism, and increased mitosis. |
 | Fig. 4Immunohistochemistry findings (×200). (A) P16 staining is diffuse positive in endocervical typed adenocarcinoma.(B) P16 staining is focal positive in minimal deviation variant. (C) Ki-67 staining shows diffuse proliferation in endocervical typed adenocarcinoma. (D) Ki-67 staining is focal in minimal deviation variant. |
References
1. Dozois RR, Judd ES, Dahlin DC, Bartholomew LG. The Peutz-Jeghers syndrome: is there a predisposition to the development of intestinal malignancy? Arch Surg. 1969. 98:509–517.
2. Payson BA, Moumgis B. Metastasizing carcinoma of the stomach in Peutz-Jeghers syndrome. Ann Surg. 1967. 165:145–151.
3. Lin JI, Caracta PF, Lindner A, Guzman LG. Peutz-Jeghers polyposis with metastasizing duodenal carcinoma. South Med J. 1977. 70:882–884.
4. Cordts AE, Chabot JR. Jejunal carcinoma in a child. J Pediatr Surg. 1983. 18:180–181.
5. Hsu SD, Zaharopoulos P, May JT, Costanzi JJ. Peutz-Jeghers syndrome with intestinal carcinoma: report of the association in one family. Cancer. 1979. 44:1527–1532.
6. Miller LJ, Bartholomew LG, Dozois RR, Dahlin DC. Adenocarcinoma of the rectum arising in a hamartomatous polyp in a patient with Peutz-Jeghers syndrome. Dig Dis Sci. 1983. 28:1047–1051.
7. Srivatsa PJ, Keeney GL, Podratz KC. Disseminated cervical adenoma malignum and bilateral ovarian sex cord tumors with annular tubules associated with Peutz-Jeghers syndrome. Gynecol Oncol. 1994. 53:256–264.
8. Aideyan UO, Kao SC. Gastric adenocarcinoma metastatic to the testes in Peutz-Jeghers syndrome. Pediatr Radiol. 1994. 24:496–497.
9. Giardiello FM, Welsh SB, Hamilton SR, Offerhaus GJ, Gittelsohn AM, Booker SV, et al. Increased risk of cancer in the Peutz-Jeghers syndrome. N Engl J Med. 1987. 316:1511–1514.
10. Entius MM, Keller JJ, Westerman AM, van Rees BP, van Velthuysen ML, de Goeij AF, et al. Molecular genetic alterations in hamartomatous polyps and carcinomas of patients with Peutz-Jeghers syndrome. J Clin Pathol. 2001. 54:126–131.
11. Kaminski PF, Norris HJ. Minimal deviation carcinoma (adenoma malignum) of the cervix. Int J Gynecol Pathol. 1983. 2:141–152.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download