Abstract
Cancer has become an important public health problem with over 800,000 new cases occurring every year in India. It is estimated that there are nearly 2.5 million cases in the country with nearly 400,000 deaths occurring due to cancer. Cancers of the female reproductive tract and breast has a high incidence amongst Indian women. Cancer registries have also highlighted that more than 70% of cancers in females occur in the age group of 35-64, and that these cancers exercise an adverse influence on the productive role of women in our society. Over 70% of patients report for diagnostic and treatment services at an advanced stage of disease, resulting in poor survival and high mortality rates. More than 50% were compliant to treatment protocol, less than 30% default during adjuvant therapy and 20% default after the preliminary investigation. Overall, 30% complete follow up in the regional institutes and 70-80% in private comprehensive care centers for five years.
Cancer has become an important Public Health Problem with over 800,000 new cases occurring every year, and is one of the ten leading causes of death in India. At any point of time, it is estimated that there are nearly 2.5 million cases in the country with nearly 400,000 deaths occurring due to cancer. Cancer incidence in India is estimated to be around 70-90 per 100,000 population. From the population based registries in India covering 28-30 million population from different parts of the country, the age adjusted incidence rates vary from 44-122 per 100,000 population in males, and 52-128 per 100,000 females.1 Cancer registries have also highlighted that more than 80% of cancer in females occur in the age group of 35-64, and 3.5% to 4.5% in childhood, thereby suggesting the impact of cancer as a major public health problem in the most productive age group. Nearly 1,500,000 people require facilities for diagnosis, treatment and follow-up at a given time.
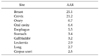
Data from population based registries under the National Cancer Registry Program indicate that the leading sites of cancer among women are the cervix uteri, breast, and oral cavity. About 50-60% of all cancers among women in India are related mainly to the four organs; cervix uteri, breast, corpus uteri, and ovaries, as shown in Table 1.1 These cancers exercise an adverse influence on the productive role of women in our society. Over 70% of the women report for diagnostic and treatment services at an advanced stage of disease, resulting in poor survival and high mortality rates.
More than 70,000 new cases of cervical uteri, 3-8% of ovarian, 0.5-4.8% of corpus uteri, 1-3% of vulvar and gestational trophoblastic tumors, and over 75,000 of breast cancers are reported in India every year. India's National Cancer Control Program emphasizes the importance of early detection and treatment. But there is no organized screening program and the majority of Indian women lack both awareness about the disease and access to prevention and treatment facilities. Although cancer screening programs are presently available in all the regional cancer centers and comprehensive cancer care specialty hospitals, which include Pap smears, as well as colposcopy, it is restricted to limited population coverage. In addition, nearly 75,000 Indian women die annually from cervical cancer disease (58%).
Nearly 70% of India's population live in rural areas where the measure of health and living standards are low. Rural women are vulnerable to most of the risk factors for cervical cancer such as early marriage, early childbirth, multiparity, poor genital hygiene, and chronic infection with sexually transmitted disease.
India, a country of more than one billion people, lacks organized Pap smear programs, and screening has not reached the vast majority of women in need. Pap smear screening is not feasible due to lack of infrastructure, cost and necessity of follow-up visits. Meta analysis of the publications on Pap screening indicates that the sensitivity of a single Pap smear is 50% and not 80%. As a result of these difficulties, many Indian women seek care only when the cancer is advanced and not amenable to curative treatment.
There are 27 regional cancer centers, and many specialty hospitals are equipped with comprehensive cancer care facilities. However, very few centers have a gynecologic oncology division served by gynecologists trained in gynecological oncology (proportionately infrastructure vs. trained gynecological oncology is lacking).
In our regional cancer center, more than 16,000 new cases have been registered, of which 8,000 cases are diagnosed with cancer annually and, of which 1,500 to 2,000 will be gynecologic cancers.2 However more than 50% were compliant to treatment protocol, and less than 30% default during the adjuvant therapy and 20% default after the preliminary investigations. Overall, 30% complete follow-up for three years in regional cancer centers and 70-80% in comprehensive care centers.
Recently, many corporate private hospitals in urban India are provided with most of the high tech facilities for diagnosis and treatment, where the complaints to treatment and follow up has much improved as most of women who have insurance coverage belong to the upper middle class. However, this constitutes less than 10% of the population coverage.
India launched its National Cancer Control Program in 1975-1976 in response to the incidence of various cancers affecting women and men. The program goals include the primary prevention of cancers through health education, secondary prevention through early detection and diagnosis, strengthening of cancer treatment facilities and patient care for patients with advanced cancer.
In 1990-91 & 1998-99, the national government established a District Cancer Control Program (DCCP) and subsequently modified the District Cancer Control Program in an effort to extend prevention and early detection services to rural communities. However, the program was not focused on cervical cancer and very little impact was observed. There was no provision for follow-up or treatment of cancer patients once diagnosed in the screening program.
Recent programs at different states have taken the initiative to overcome the pitfalls of the earlier ones to reach common women in the public sector, community level, and referral in appropriate time to the institution so as to benefit from the treatment protocol and survival benefits. However, many non-governmental organizations, professional bodies, philanthropic trusts, and their commitments, co-operation and coordinations from all parts including women motivation in her own health care system makes any program successful. The Association of Gynecological Oncologists of India (AGOI) has proposed to the Health & Family Welfare, Government of India a simple program for the prevention and early detection of cervical cancer, and also for the formal certified fellowship training program for the development of subspeciality of gynecological oncology in India, and telemedicine for the improved pattern of care for women suffering from gynecological malignancies. The association also proposed to bring the AGOI guidelines for the practicing gynecological oncologists, gynecologists, and other oncologists.
The majority of the women with cervical cancer present with advanced stage, where surgery may not be suitable. However, cervical precancerous lesions were treated according to the age and with concern to fertility issues. Early invasive cervical cancer of stage Ia1 is treated with extrafascial hysterectomy, stage Ia2 without lymphovascular space invasion is subjected to extended type II radical hysterectomy with pelvic lymphadenectomy, and stage Ib1 to stage IIa (selected cases) are subjected to radical hysterectomy (RH type III) with retroperitoneal pelvic lymphadenectomy with or without salpingo-oophorectomy. Depending upon the surgico-pathological prognostic risk factors, postoperative adjuvant radiotherapy or chemoradiation is recommended. Low risk patients are kept on regular follow up, intermediate risk patients are subjected to adjuvant brachytherapy with or without pelvic radiation, and in patients high risk prognostication, chemoradiation is recommended. Cervical cancer stage IIb to stage IIIb and selected stage Ib2-IIa chemoradiation is recommended. Few patients who partially responded to chemoradiation or external pelvic radiotherapy, and not suitable for intracavitary brachytherapy were subjected to surgery when the parametrium clinically appeared free of disease with residual disease confined to the cervix. However, those women with advanced disease, not affordable for chemotherapy, radiation therapy is recommended. Some women with bulky early disease are subjected to neoadjuvant chemotherapy for 2-3 cycles, followed by surgery at 2-3 week intervals. Clinically proved stage IV disease with good performance status, either with distant metastases or locally invasive will be subjected to diversion colostomy followed by palliative chemoradiation or palliative chemotherapy.
Most often ovarian neoplasms are either referred with radiological diagnosis or present with pelvic or abdomino-pelvic masses with or without ascites, and rarely with distant metastases. Depending upon the performance status and feasibility of surgery, the majority of women are subjected to primary cytoreductive surgery followed by six courses of adjuvant chemotherapy, either paclitaxel with carboplatin based, or single agent carboplatinum or cisplatinum with cyclophosphamide chemotherapy. Some of the women with poor performance status, not suitable for primary surgery are subjected to 2-3 courses of neoadjuvant chemotherapy followed by interval debulking surgery IDS, either after confirmation by cytological or histopathological diagnosis for ovarian cancer. Those women present with inadequate staging or suboptimal surgery referred from other hospitals are either subjected to re-exploratory staging laparotomy or adjuvant chemotherapy followed by completion surgery. The majority of stage IV disease were treated with neoadjuvant chemotherapy followed by interval debulking surgery depending upon the response and performance status, and postoperatively followed by three more cycles of chemotherapy. Few of those with cardiopulmonary compromise or medically co-morbid conditions and therefore unfit for surgery receive only palliative chemotherapy after confirmed diagnosis for ovarian malignancy. Depending upon platinum sensitivity, site of recurrence, and disease-free interval, either secondary cytoreduction followed by second-line chemotherapy or second-line chemotherapy is recommended.
Adolescent girls presented with ovarian neoplasms were subjected to comprehensive surgical staging with unilateral salpingo-oophorectomy, omentectomy with or without retroperitoneal lymphadenectomy. Except for stage Ia pure dysgerminomas and grade 1 immature teratomas, all others were subjected to adjuvant chemotherapy (BEP regimens) for 3-4 cycles.
The majority of women present with either postmenopausal or perimenopausal bleeding prior to being diagnosed as endometrial cancer, or primary inadequately staged for corpus uteri cancers were referred for further management. Primarily presented patients with histopathology reports were subjected to extrafascial hysterectomy with retroperitoneal lymphadenectomy and peritoneal cytology. Depending upon the surgico-pathological prognostication, regular surveillance was recommended for low-risk groups (endometeroid adenocarcinoma, stage Ia, b, grade1, 2), while intermediate groups (stage Ia, b, grade3, selected stage II) were subjected to brachytherapy. For stage Ic all grade, clear cell carcinoma, papillary serous carcinoma, adenosquamous carcinoma, and undifferentiated carcinoma, they were recommended with adjuvant pelvic radical radiotherapy. Stage IIIa was subjected to with or without chemotherapy (adriamycin based) when the adenexa were involved, and when the uterine serosa was involved, radical radiotherapy is recommended. Stage IIIb-IIIc was recommended with radiotherapy with or without chemotherapy. Those women who had been operated from elsewhere with inadequate staging were recommended to radiotherapy, as most of the patients were not willing to undergo further staging laparotomy after the first surgery.
This most often occurs in elderly women (1-3%), with or without co-morbid medical conditions. However, the majority of undergo radical vulvectomy and inguinofemoral lymphadenectomy. Depending upon the surgico-pathological prognosticators, patients will be subjected to either regular follow-up in early stage low risk patients or adjuvant therapy whenever indicated.
Reproductive young women rarely (<1%) present with either highly raised value of beta serum hCG, or metastatic disease followed by evacuation of molar pregnancy, post abortion or postterm. All these women were subjected to WHO Prognostic score and accordingly treated with either single agent (Methotrexate/D-actinomycin for low risk) or multi-agent chemotherapy (EMA-CO/EMA-EP regimens for high risk) as recommended, with regular monitoring of beta serum hCG after therapy until three consecutive values of beta serum hCG reach normal (<10 mIU/ml), and two more cycles for low risk women and three more cycles for high risk women is recommended. Thereafter, low risk patients were regularly monitored for one year with beta serum hCG and advised contraception, and for high risk patients two years minimum follow up was recommended.
Women treated for gynecological malignancies were kept on surveillance at three monthly interval for two years and then six monthly for the next three years and annually thereafter until the lifespan. During the follow up, if the recurrent disease was detected, patients were treated accordingly. However, in the public sector hospitals, despite providing free transportation train pass and other facilities, due to financial constraints, the majority of the patient dropout on follow-up.
Figures and Tables
ACKNOWLEDGEMENTS
The author would like to acknowledge Dr. C. Ramesh, M. Sc; PhD; Dr. Ramachandra Reddy, M.Sc; PhD; Mr. K. Venkatesh, MSc; staff of Department of Epidemiology, Biostatistics & Hospital Cancer Registry, staff of Gyanecological Oncology, Medical Records, Director & Medical Superindent, Kidwai Memorial Institute of Oncology, Bangalore, Karnataka State, India.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download