Abstract
Objective
The colposcopic vision guided loop electrosurgical excisional procedure (LEEP) was studied for the effective diagnosis of cervical cancer and cervical intraepithelial neoplasia (CIN).
Methods
A total of 199 patients participated in this study. Individual cases were from gynecologic outpatients at Thammasat University Hospital, Thailand. These had diagnoses for CIN and were selected for treatment with colposcopic guided LEEP. The average age of patients in this study was 45. Menopausal women represented 31%, (61/199) of the patients. The most frequently found Pap smear result among these women (44%, 88/199), was that of high-grade squamous intraepithelial lesion. The next most frequent Pap smear result (32%, 64/199) was low-grade squamous intraepithelial lesion. Patients' medical records and outcomes were evaluated for consistency of pathological examination between colposcopic directed biopsy and LEEP. Discrepancies between initial diagnosis and the final diagnosis were also analyzed.
Results
The colposcopic guided LEEP accurately determined 100% of the cervical cancer cases and 84.8 % of the high-grade squamous intraepithelial lesion cases. Involvement of the ectocervical or endocervical margin regions was found to be 5% and 10% respectively, in this study. Excessive bleeding complication, either during the excision and/or postoperative recovery was found in 3% and 6% of cases, respectively.
Cervical intraepithelial neoplasia (CIN) II-III of the uterine cervix are now classified as high-grade precancerous lesions. Treatment requires an aggressive surgical approach. CIN I cases, on the other hand are still treated in Thailand with a "wait-and-see" approach.
Cervical conization is the treatment of choice for high-grade precancerous lesions. Loop electrosurgical excision procedure (LEEP) is one of the accepted techniques for cervical conization. It has been widely used in gynecologic oncology practices worldwide. This is because the technique allows the simultaneous collection of specimens for further histopathological and therapeutic diagnostics and can be performed in an outpatient setting using local anesthesia.1,2
Generally in Thailand, by contrast, the LEEP technique is usually performed in an operating room (OR). Physician performs the procedure in an OR, based on colposcopic record from an outpatient examination without the help of optical equipment. LEEP in OR consumes operating room time and requires a large number of operating room personnel. This practice has resulted in high costs for the patients.
Incomplete excision using LEEP is also a major problem. The relative risk (RR) of precancerous lesions post-treatment of any grade, including high-grade lesions are 5.47 (95% CI, range 4.37 to 6.83) and 6.09 (95% CI, range 3.87 to 9.60) from a 40-year worldwide meta-analysis, respectively. This is in comparison with the reference group, who all had complete excision of the lesion.3 Other reports revealed that an incomplete excision after LEEP was a significant predictor for both persistence and recurrence of CIN during follow up.4-6
The American Society for Colposcopy and Cervical Pathology (ASCCP) still recommends a repeat excision as the first option in women who had CIN II-III with cone margin involvement after LEEP.7
In the colposcopic unit of Thammasat University Hospital, we perform LEEP in all women who have an indication for cervical conization. We use local anesthetic injection of the cervix under colposcopic vision in an ambulatory care setting. This procedure minimizes incomplete excision of the lesion. It can be performed as an outpatient procedure and the women can go home afterwards. Accordingly, this study was conducted to evaluate the effectiveness of LEEP under colposcopic vision.
This investigation received the approval from the ethic committee on clinical research of the Faculty of Medicine, Thammasat University in 2007. One hundred and ninety nine women with indications for cervical conization were found to require LEEP from among 703 women with abnormal Pap smears. This represented 100% of all suitable patients, who attended Thammasat University Hospital colposcopy clinic from July 2002 to June 2007.
Recruited patients, after confirmation of their abnormal Pap smears, received colposcopic biopsies and endocervical curettage (ECC). They then came in to the clinic after two weeks to get their histopathological results and diagnosis. The further treatment plan, namely outpatient cervical conization, was given out to the patients at this stage. All subjects agreed to the plan and then received LEEP under colposcopic vision procedure in the same day. LEEP was conducted with a local anesthetic injection.
Size of the loop used in each patient varied to ensure complete removal of the precancerous lesion. A 5-mm hemostatic ball electrode in pure coagulation mode was used to stop the bleeding without Monsel's solution. A vaginal gauze tampon with antibiotic ointment was then applied to the LEEP site for 6 hours. Patients were sent home with instruction for self care.
Patients were requested to come in for LEEP histopathological reports in two weeks. Final diagnosis was confirmed and further treatment suggested, along with 4 weeks and 6 months follow up gynecological examinations.
Cervical biopsy reports, LEEP histological reports and final diagnosis were all collected for this report. Data were analyzed with SPSS 11.0.
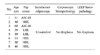
All recruited subjects were walk-in cases requesting cervical cancer screening. Age distribution of subjects in this study is presented in Table 1. The average age of subjects was 45 years old. Sixty-one women (31%) were of menopause age. Thirty-two and twenty-seven percent constituting the majority cases were 31-40 and 41-50 years old respectively.
The most frequently found Pap smear in this investigation was high-grade squamous intraepithelial lesion (HSIL), followed by low-grade squamous intraepithelial lesion (LSIL) (44% and 32% respectively). Unfortunately we found 2 invasive cervical carcinoma cases in women of age less than 30 years old. Both of them were diagnosed from LEEP biopsies.
The final histopathological diagnostic judgment was the most severe histopathological report from either colposcopic or LEEP biopsies.
Final histopathological reports revealed that 9 patients had cervical cancer. Only 3 of these 9 cases (33%) presented cervical cancer cells based on their cytology report (Table 1). The other 6 cervical cancer cases were identified by cytology result as HSIL. All 9 cases were small lesion cervical cancer, difficult to detect by colposcopic biopsy.
Correlation of LEEP histopathology and final histopathological diagnostic judgement case is presented in Table 2.
Of 129 patients with a HSIL from final diagnosis, 108 (84%) had histologically proven high-grade dysplasia while 21 (16%) had only low-grade dysplasia from LEEP biopsies. Of 82 patients with a low-grade dysplasia or none from LEEP biopsies, 21 (26%) had histologically high-grade dysplasia from colposcopic biopsies.
In this study 8 subjects had no pathologic finding from both colposcopic and LEEP biopsies. They all decided to undergo LEEP due to the indication of unsatisfactory colposcopy as shown in Table 3.
The incidence of unrecognized invasive cervical carcinoma in other studies was 0.9 to 9.6%.10-13 These reports came from cases of positive endocervical margin in LEEP or conization specimens. In the present study, 9 women (5%) who underwent LEEP had invasive cervical carcinoma although only 3 had previously been suspected of having cervical carcinoma from Pap smear results. The percentage falls into the same range and is comparable to other studies. We also found 19 positive endocervical margin cases (10%). All of them had no invasive cervical carcinoma.
Gold standard reference and cases with HSIL or higher are of major interest in this investigation. The final histopathological diagnoses were classified based on the most pathological severity either from colposcopic or LEEP biopsies. See and treat LEEP was not performed here.14-18 This explains why some colposcopic biopsy cases had more severe histopathology than LEEP biopsies.
When a precancerous lesion was very small, the remaining cervix would have the same or less severe pathology than that of colposcopic biopsies. This explains why overall LEEP under colposcopic vision here yielded less than perfect correlation (84.8%) with the final diagnosis.
LEEP under colposcopic vision gave 100% specificity and positive predictive value (PPV)(Table 4). Negative predictive value (NPV) is 74.4%. This negative predictive value is satisfactory for HSIL or higher cases since the disease development takes a long period of time. One can also use HPV DNA testing or liquid-based Pap smear in the follow-up of the disease.
We use final diagnosis to evaluate the concept of LEEP under colposcopic vision. An acetic acid solution (3%) was soaked in gauze and applied to the cervix to create acetowhite lesion prior to the procedure. This condition is transient. This may explain the 9 cases (5%) with positive ectocervical margin involvement.
In conclusion, 100% invasive cervical carcinoma and HSIL were diagnosed with 100 and 84.8% accuracy from this technique in correlation with the final diagnosis. LEEP under colposcopic vision is a recommended technic for ambulatory management of precancerous lesion and early diagnosis of cervical cancer. This technique significantly reduces the observed rate of positive ectocervical cone margin involvement by earlier detection.
Figures and Tables
Table 3
Detail of subjects with no dysplasia finding or higher from both colposcopic and LEEP biopsies
References
1. Wright TC, Gagnon S, Richart RM, Ferency A. Treatment of intraepithelial neoplasia using the loop electrosurgical excision procedure. Obstet Gynecol. 1991. 79:173–178.
2. Prendiville W, Cullimore J, Norman S. Large loop excision of the transformation zone (LLETZ): a new method of management for women with cervical intraepithelial neoplasia. Br J Obstet Gynaecol. 1989. 96:1054–1060.
3. Ghaem-Maghami S, Sagi S, Majeed G, Soutter WP. Incomplete excision of cervical intraepithelial neoplasia and risk of treatment failure: a meta-analysis. Lancet Oncol. 2007. 8:985–993.
4. Felix JC, Muderspach LI, Duggan BD, Roman LD. The significance of positive margins in loop electrosurgical cone biopsies. Obstet Gynecol. 1994. 84:996–1000.
5. Brockmeyer AD, Wright JD, Gao F, Powell MA. Persistent and recurrent cervical dysplasia after loop electrosurgical excision procedure. Am J Obstet Gynecol. 2005. 192:1379–1381.
6. Das N, Naik R, Jackson S, De Barros Lopes A, Monaghan JM, Godfrey KA, et al. Recurrent smear abnormalities where repeat loop treatment is not possible: is hysterectomy the answer? Gynecol Oncol. 2005. 97:751–754.
7. Wright TC Jr, Cox JT, Massad LS, Carlson J, Twiggs LB, Wilkinson EJ. American Society for Colposcopy and Cervical Pathology 2001 consensus guidelines for the management of women with cervical intraepithelial neoplasia. Am J Obstet Gynecol. 2003. 189:295–304.
8. Huang LW, Hwang JL. A comparison between loop electrosurgical excision procedure and cold knife conization for treatment of cervical dysplasia: residual disease in a subsequent hysterectomy specimen. Gynecol Oncol. 1999. 73:12–15.
9. Panoskaltsis T, Ind TE, Perryman K, Dina R, Abrahams Y, Soutter WP. Needle versus loop diathermy excision of the transformation zone for the treatment of cervical intraepithelial neoplasia: randomized controlled trial. BJOG. 2004. 111:748–753.
10. Husseinzadeh N, Shbaro I, Wesseler T. Predictive value of cone margins and post-cone endocervical curettage with residual disease in subsequent hysterectomy. Gynecol Oncol. 1989. 33:198–200.
11. Whiteley PF, Olah KS. Treatment of cervical intraepithelial neoplasia: experience with low voltage diathermy loop. Am J Obstet Gynecol. 1990. 162:1272–1277.
12. Natee J, Therasakvichaya S, Boriboonhirunsarn D. Prevalence and risk factors for residual cervical neoplasia in subsequent hysterectomy following LEEP or conization. J Med Assoc Thai. 2005. 88:1344–1348.
13. Kietpeerakool C, Khunamornpong S, Srisomboon J, Siriaunkgul S, Suprasert P. Cervical intraepithelial neoplasia II-III with endocervical cone margin involvement after cervical loop conization: is there any predictor for residual disease? J Obstet Gynaecol Res. 2007. 33:660–664.
14. Keijser KG, Kenemans P, van der Zanden PH, Schijf CP, Vooijs GP, Rolland R. Diathermy loop excision in the management of cervical intraepithelial neoplasia: diagnosis and treatment in one procedure. Am J Obstet Gynecol. 1992. 166:1281–1287.
15. Ferris DG, Hainer BL, Pfeninger JL, Zuber TJ. See and treat electrosurgical loop excision of the cervical transformation zone. J Fam Pract. 1996. 42:253–257.
16. Bigrigg MA, Codling BW, Pearson P, Read MD, Swingler GR. Colposcopic diagnosis and treatment of cervical dysplasia at a single clinic visit: experience of low-voltage diathermy in 1000 patients. Lancet. 1990. 336:229–231.
17. Darwish A, Gadallah H. One-step management of cervical lesions. Int J Gynaecol Obstet. 1998. 61:261–267.
18. Wootipoom V, Chicharoen S, Bungachat R. Loop electrosurgical excision procedure (LEEP) and colposcope. Songkla Med J. 1999. 17:133–138.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download