Abstract
Objective
The risk factors associated with early ventral site hernia development following cancer surgery are ill defined and associated with an undetermined incidence.
Methods
We analyzed 1,391 gynecologic cancer patient charts to identify the number of post-operative ventral site hernias over a nearly 6 year period. The following study variables were noted for evaluation: patient demographics, disease co-morbidity (hypertension, cardiovascular disease, diabetes), body mass index (BMI), treatment (e.g., chemotherapy regimen), intra-operative (e.g., bleeding) and postoperative (e.g., infection) complications, time to hernia development and length of hospital stay.
Results
Twenty-six gynecologic cancer patients who developed a post-operative ventral hernia and subsequently underwent herniorrhaphy by our gynecologic oncology service were identified. The patient group's overall time to initial hernia development was 11.23 months. Following a multiple regression analysis, we found that treatment (e.g., bevacizumab, liposomal doxorubicin or radiotherapy associated with compromised wound healing [p=0.0186] and disease co-morbidity [0.0432]) were significant prognostic indicators for an accelerated time to hernia development. Moreover, five patients underwent treatment associated with compromised wound healing and also had disease co-morbidity. In this sub-group, post-operative hernia development occurred more rapidly (3.8 months) than the overall group of patients. BMI and age did not impact time to hernia development (p>0.05).
Conclusion
In the present gynecologic cancer patient series, a tendency for early post-operative hernia development appeared to coincide with treatment associated with compromised wound healing and disease co-morbidity. Gynecologic cancer surgeons should anticipate this potential complication and consider employing prophylactic intra-operative mesh to potentially prevent this condition.
An incisional hernia is a common postoperative complication and major source of patient morbidity.1 Ventral hernias originate from a previous surgical incision and can be caused by the stretching of scar tissue during the resumption of normal activities.2 In abdominal surgery, there appears to be a high incidence of hernias associated with vertical midline abdominal incisions, with a reported risk of 5-15%.3,4 Moreover, an increased risk of ventral site hernia development may significantly coincide with an adverse health status.5
Select surgical studies have attempted to address the specific factors that potentially contribute to the premature manifestation of ventral site hernias.2,6-8 In particular, they have examined time to hernia development, patient co-morbidity, the impact of specific treatment (e.g., with or without mesh).9,10 However, since many gynecologic cancer patients are immuno-compromised, present with extensive disease or are susceptible to wound dehiscence, they may be at greater risk for a post-operative ventral site hernia.11
In an attempt to appropriately explicate these issues, we conducted a retrospective data review documenting our gynecologic cancer patient management experience with post-operative ventral site hernias. We speculate that a patient's unfavorable pre-operative health status (>25 body mass index [BMI], history of cardiovascular disease or diabetes) may significantly precipitate ventral hernia development subsequent to gynecologic cancer surgery.
We retrospectively reviewed the charts of 1,391 gynecologic cancer patients who were treated by our gynecologic oncology service from August 2003 until April 2009. We also included ovarian cystadenoma patients since this disease subtype is associated with a potential for malignant transformation.12 One hundred and five patients with post-operative hernias were identified, 26 of whom were treated and followed by a gynecologic oncologist. The remaining hernia patients were referred out to general surgery and relevant follow-up data were not available. Institutional review board approval was obtained prior to any data collection and investigation.
Pre-operative cancer evaluation was confirmed via biopsy in all cases. Serum albumin levels were available on 8 patients (mean score=3.91). Patients were all classified as P2 using the standards of the American Society of Anesthesiologists. The following clinical data were collected for the completion of this study: patient co-morbidity/medical history, BMI, treatment (surgery type, chemotherapy or radiotherapy [RT]), estimated blood loss, intra-operative complications (e.g., hemorrhage), postoperative complications (e.g., infection) length of hospital stay, and time to initial hernia development.
All statistical analyses were conducted using MedCalc ver. 9.5.1 (MedCalc Software bvba, Mariakerke, Belgium). The initial data analysis was conducted by employing a descriptive statistical approach, which underwent further examination via multiple regression and 2-sided p-values (<0.05) to determine significance.
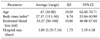
Following a review of gynecologic cancer surgery records, 26 patients who developed a post-operative ventral site hernia were identified. The study subjects' mean age was 67 years (95% CI, 62.60 to 70.71), height was 63.7 inches (95% CI, 62.41 to 64.97), and weight was 149 pounds (95% CI, 128.64 to 169.36). Patient mean BMI was 27.37 (95% CI, 23.84 to 30.90) (Table 1). Thirteen patients were normal weight, nine patients were obese, three were overweight, and one patient was underweight.13
The majority of subjects underwent a laparotomy, total abdominal hysterectomy, bilateral salpingo-oophorectomy, and bilateral pelvic lymphadenectomy. Twelve patients received adjuvant paclitaxel and carboplatin chemotherapy alone and four patients received bevacizumab in conjunction with paclitaxel and carboplatin. Three patients received liposomal doxorubicin and two patients underwent radiotherapy for the treatment of recurrent cancer. Five patients did not have any adjuvant therapy.
There were no intra-operative or post-operative complications associated with herniorrhaphy and EBL was 53.27 ml (95% CI, 48.88 to 57.65). Mean hospital stay was 3.89 days (95% CI, 3.19 to 4.58). Twenty-one patients underwent hernioplasty with mesh. Time to initial hernia development was 11.23 months (95% CI, 7.55 to 14.91) (Table 2).
In a multivariate regression analysis, we examined the prognostic impact of age, BMI, disease progression, EBL, inclusion of treatment (e.g., bevacizumab, liposomal doxorubicin or RT) associated with compromised or delayed wound healing and disease co-morbidity (e.g., diabetes, hypertension, cardiovascular disease) on time to hernia development. Treatment associated with compromised wound healing was the most significant predictor for time to hernia development (R2=-2.533, p=0.0186). The second most significant prognostic variable for time to hernia development was patient co-morbidity (R2=-2.139, p=0.0432), while BMI and patient age were not significant indicators (p>0.05).
The nine patients who underwent treatment associated with compromised or delayed wound healing exhibited a mean time of 5.1 months until hernia development. Nine patients also had disease co-morbidity and demonstrated a mean time of 4.6 months until hernia development. Interestingly, the five patients who underwent treatment associated with compromised wound healing and also had disease co-morbidity, exhibited a mean time of 3.8 months until to hernia development.
Approximately 100,000 ventral hernia repairs are performed each year in the United States.3 Ventral hernias can develop from heavy straining, increased age, acute injury or strain and an infection at the site of surgery. They can occur spontaneously or manifest years following the surgical procedure.
The incidence of ventral site hernia development following abdominal surgery has been previously reported,3 but the potential contributing factors associated with gynecologic cancer surgery have not been extensively studied.9,10,13 Therefore, the purpose of this retrospective study was to identify the relevant prognostic factors inherent in early ventral hernia development following gynecologic cancer surgery.
In the current investigation, a significant relationship between relevant disease co-morbidity, such as diabetes, cardiovascular disease or hypertension, and time to hernia manifestation was identified. The nine patients who had one of or a combination of the aforesaid co-morbid conditions developed a post-operative hernia much sooner than the overall group, consistent with previously reported research.14,15 In particular, their average time to hernia development occurred at over twice the rate of the overall, present study population. Since diabetics are markedly prone to micro-vascular disease and are at risk for compromised or delayed post-operative wound healing, the faster rate of hernia development is presumably related to the narrowing of the small vessels (i.e., micro-vascular disease) involved in this condition.14,16
The impact of treatment (e.g., liposomal doxorubicin, bevacizumab and RT) associated with compromised wound healing also correlated with a faster time to hernia development.17 In the subgroup of patients who received this particular treatment, initial hernia manifestation occurred nearly two times faster than the overall group, a rate which is consistent with prior research.13 Surprisingly, BMI was not a significant predictive variable considering that obesity and overweight are classically identified as factors in the development of post-operative hernias (i.e., the incidence of post operative hernias is three times higher in these patients).18
Studies have reported that liposomal doxorubicin has been associated with compromised wound healing,19,20 particularly when administered within 3 months post surgery. Similarly, bevacizumab has been correlated with impaired bowel mucosal renewal or neovascularization, which may contribute to the manifestation of bowel perforations.21-23 Consequently, we elect to initiate bevacizumab at cycle 2 (i.e., delaying treatment by approximately one month) during induction chemotherapy to minimize the risk of surgical wound or bowel anastomotic healing complications.22 Moreover, we recognize that any appreciable treatment impact on ventral hernia development is confounded by the nonstandard timing (i.e., first line or 2nd line therapy) and type of therapy for the participants in the present study.
Interestingly, we also found that the current study patients with disease co-morbidity (N=5) who also received treatment associated with compromised wound healing (i.e., two risk factors), developed post-operative hernias even more rapidly than the subjects who had only one risk factor (3.8 months vs. 5.1 or 4.6 months). Initially, we wanted to analyze this issue but the limited patient numbers precluded further evaluation. Nevertheless, we conjecture that the heightened proclivity for hernia development in these patients is attributed to an aggregate number of risk factors.24
Since patients who have a determining co-morbid disease or were treated with a therapy associated with wound healing complications may be predisposed to developing a post-operative hernia, gynecologic cancer surgeons may consider employing intra-operative prophylactic mesh to address the potential weakness and prevent this event.8,24 In fact, studies have indicated that prosthetic mesh has significantly reduced the recurrence rates for incisional ventral hernia repair and therefore, utilizing mesh at the time of initial surgery may avert this complication.7,8
We propose that a metric or scale should be developed for the pre-operative evaluation of gynecologic cancer surgery candidates. This measurement schema should consider specific high-risk criteria in determining which gynecologic cancer patients may be more predisposed to developing a post-operative hernia. If necessary, prophylactic subfascial, non-absorbable mesh reinforcement in these high-risk patients can be used safely and effectively to bolster the strength of the surgically compromised area, thereby preventing wound dehiscence and a subsequent incisional hernia.7,8 Conversely, to mitigate the incidence of incisional hernia without exacerbating wound pain or suture sinus frequency, slowly absorbable, continuous sutures may be indicated for fascial closure.5,25
In high risk patients, relevant management in the form of nutritional evaluation, diabetes or cardiovascular education, and routine medical follow-up are essential to assure favorable surgical and medical outcomes.26 However, since the incidence of hernias in this group of patients is rather low, a cost analysis to investigate the value of preventive surgical intervention during gynecologic cancer surgery may be warranted.
We recognize that serum albumin levels would have been an interesting variable to consider, particularly given that this protein has been studied extensively as an indirect measure of nutrition and appears to be associated with inferior outcomes in ovarian cancer surgery.27 Moreover, since cervical cancer patients undergo adjuvant chemotherapy and would be more vulnerable to a ventral hernia, the study would have benefited from the inclusion of these patients. We suspect an absence of these patients or any additional inadvertently excluded subjects was attributed to either a coding issue limiting the chart selection process, or because of general surgery referrals.
The limited number of patients and non-randomized nature of this single institutional study preclude any definitive conclusions regarding the appropriate management of ventral site hernias in gynecologic cancer patients. However, we contend that our data are provocative and underscore the potential significance of considering the prophylactic inclusion of mesh in high risk gynecologic cancer surgery patients. Additional study of these prognostic variables and corresponding outcomes in a larger gynecologic cancer patient population is warranted.
References
1. Singh R, Omiccioli A, Hegge S, McKinley C. Does the extraction-site location in laparoscopic colorectal surgery have an impact on incisional hernia rates? Surg Endosc. 2008. 22:2596–2600.
2. Hadad I, Small W, Dumanian GA. Repair of massive ventral hernias with the separation of parts technique: reversal of the 'lost domain'. Am Surg. 2009. 75:301–306.
3. Cheng H, Rupprecht F, Jackson D, Berg T, Seelig MH. Decision analysis model of incisional hernia after open abdominal surgery. Hernia. 2007. 11:129–137.
4. Millikan KW. Incisional hernia repair. Surg Clin North Am. 2003. 83:1223–1234.
5. El-Khadrawy OH, Moussa G, Mansour O, Hashish MS. Prophylactic prosthetic reinforcement of midline abdominal incisions in high-risk patients. Hernia. 2009. 13:267–274.
6. Larusson HJ, Zingg U, Hahnloser D, Delport K, Seifert B, Oertli D. Predictive factors for morbidity and mortality in patients undergoing laparoscopic paraesophageal hernia repair: age, ASA score and operation type influence morbidity. World J Surg. 2009. 33:980–985.
7. Wassenaar EB, Schoenmaeckers EJ, Raymakers JT, Rakic S. Recurrences after laparoscopic repair of ventral and incisional hernia: lessons learned from 505 repairs. Surg Endosc. 2009. 23:825–832.
8. Gangopadhyay N, Perrone JM, Soper NJ, Matthews BD, Eagon JC, Klingensmith ME, et al. Outcomes of laparoscopic paraesophageal hernia repair in elderly and high-risk patients. Surgery. 2006. 140:491–498.
9. Schneider A, Kohler C, Erdemoglu E. Current developments for pelvic exenteration in gynecologic oncology. Curr Opin Obstet Gynecol. 2009. 21:4–9.
10. O'Hanlan KA, Dibble SL, Fisher DT. Total laparoscopic hysterectomy for uterine pathology: impact of body mass index on outcomes. Gynecol Oncol. 2006. 103:938–941.
11. Munro MG. Laparoscopic access: complications, technologies, and techniques. Curr Opin Obstet Gynecol. 2002. 14:365–374.
12. Mahdavi A, Kumtepe Y, Nezhat F. Laparoscopic management of benign serous neoplasia arising from persistent ovarian remnant. J Minim Invasive Gynecol. 2007. 14:654–656.
13. Hoer J, Lawong G, Klinge U, Schumpelick V. Factors influencing the development of incisional hernia: a retrospective study of 2,983 laparotomy patients over a period of 10 years. Chirurg. 2002. 73:474–480.
14. Vermulst N, Vermeulen J, Hazebroek EJ, Coene PP, van der Harst E. Primary closure of the skin after stoma closure: management of wound infections is easy without (long-term) complications. Dig Surg. 2006. 23:255–258.
15. Hoogwerf BJ. Postoperative management of the diabetic patient. Med Clin North Am. 2001. 85:1213–1228.
16. Shermak MA. Hernia repair and abdominoplasty in gastric bypass patients. Plast Reconstr Surg. 2006. 117:1145–1150.
17. Geller MA, Argenta PA, Thomas SG, Dusenbery KE, Judson PL, Boente MP. Feasibility and morbidity of using saline filled tissue expanders to reduce radiation-induced bowel injury in patients with gynecologic malignancies. Eur J Obstet Gynecol Reprod Biol. 2009. 143:93–97.
18. Langer C, Schaper A, Liersch T, Kulle B, Flosman M, Fuzesi L, et al. Prognosis factors in incisional hernia surgery: 25 years of experience. Hernia. 2005. 9:16–21.
19. Zatkone Puskas G. The significance of extravasation in oncological care. Magy Onkol. 2008. 52:75–80.
20. Phillips TL, Fu KK. Acute and late effects of multimodal therapy on normal tissues. Cancer. 1977. 40:1 Suppl. 489–494.
21. Tsopanoglou NE, Maragoudakis ME. Inhibition of angiogenesis by small-molecule antagonists of protease-activated receptor-1. Semin Thromb Hemost. 2007. 33:680–687.
22. Micha JP, Goldstein BH, Rettenmaier MA, Genesen M, Graham C, Bader K, et al. A phase II study of outpatient first-line paclitaxel, carboplatin and bevacizumab for advanced stage epithelial ovarian, peritoneal, and fallopian tube cancer. Intl J Gynecol Cancer. 2007. 17:771–776.
23. Simpkins F, Belinson JL, Rose PG. Avoiding bevacizumab related gastrointestinal toxicity for recurrent ovarian cancer by careful patient screening. Gynecol Oncol. 2007. 107:118–123.
24. Rai S, Chandra SS, Smile SR. A study of the risk of strangulation and obstruction in groin hernias. Aust N Z J Surg. 1998. 68:650–654.
25. van't Riet M, Steyerberg EW, Nellensteyn J, Bonjer HJ, Jeekel J. Meta-analysis of techniques for closure of midline abdominal incisions. Br J Surg. 2002. 89:1350–1356.
26. Harvey PW, Petkov JN, Misan G, Fuller J, Battersby MW, Cayetano TN, et al. Self-management support and training for patients with chronic and complex conditions improves health-related behaviour and health outcomes. Aust Health Rev. 2008. 32:330–338.
27. de Jong D, Eijkemans MJ, Lie Fong S, Gerestein CG, Kooi GS, Baalbergen A, et al. Preoperative predictors for residual tumor after surgery in patients with ovarian carcinoma. Oncology. 2007. 72:293–301.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download