Abstract
Objective
To evaluate treatment outcomes and prognostic factors in uterine cervical cancer patients treated with postoperative extended field radiation therapy (POEFRT) with or without chemotherapy.
Methods
Between 1983 and 2006, 35 patients with a pathologically confirmed positive para-aortic node (PAN) or common iliac node (CIN) who underwent a radical hysterectomy with bilateral pelvic lymph node dissection and PAN dissection received POEFRT with (N=23) or without (N=12) chemotherapy. Prognostic factors such as age, stage, size, parametrium invasion, lymphovascular space invasion, nodal station, depth of stromal invasion and use of chemotherapy were analyzed.
Results
With a median follow-up of 44 months, the 5-year overall survival (OS), disease-free survival (DFS), distant failure-free survival (DFFS) and loco-regional failure-free survival rates were 51%, 51%, 59% and 93%, respectively. The use of chemotherapy significantly improved the 5-year OS rate (61% vs. 48%, p=0.004), the 5-year DFS rate (54% vs. 38%, p=0.004) and the 5-year DFFS rate (57% vs. 48%, p=0.009). PAN involvement resulted in a compromised 5-year DFS rate (42% vs. 73%, p=0.002) and 5-year DFFS rate (47% vs. 82%, p=0.004) as compared to CIN involvement. Grade 3 or higher hematological toxicity was observed more frequently in patients who received POEFRT combined with chemotherapy as compared to patients who received POEFRT alone (52% vs. 17%, p=0.04).
Radical hysterectomy with bilateral pelvic lymph node dissection (PLND) and para-aortic lymph node sampling is frequently employed with a curative intent in early stage cervical cancer patients. However, as several pathological risk factors such as deep stromal invasion, bulky tumor size, lymphovascular space invasion, lymph node metastasis, involvement of the resection margin, and involvement of the parametrium have been identified to compromise treatment outcomes, postoperative radiotherapy has been recommended for patients with high risk factors.1,2 Among the risk factors, the presence of a common iliac node (CIN) and/or a para-aortic node (PAN) metastasis represents the most significant negative prognostic factor.3,4 Although several studies have reported that extended-field radiation therapy (EFRT) may cure patients with a PAN metastasis, the survival outcome of these patients is poor, with 5-year survival rates ranging from 25% to 40%.5-7 The addition of chemotherapy (CTx) to EFRT is the next step to improve treatment outcome. In two prospective randomized studies, this approach has been used to evaluate treatment outcomes.8,9 The reported survival rates at two to three years as determined from these studies were approximately 39% to 47%, but high rates of toxicity were observed.8,9 Contrary to these studies where EFRT with or without CTx was used with a curative purpose, few studies have investigated the use of postoperative EFRT (POEFRT).
In this study, we have attempted to review treatment outcomes and prognostic factors in uterine cervical cancer patients with a pathologically confirmed positive CIN or PAN who underwent radical hysterectomy with bilateral PLND and PAN dissection, and received POEFRT with or without CTx.
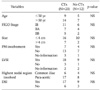
Between September 1983 and March 2006, 40 patients with a pathologically confirmed positive PAN or CIN who underwent a radical hysterectomy with bilateral PLND and PAN dissection received POEFRT at the Seoul National University Hospital. Of the 40 patients, five patients were excluded due to following reasons: three patients underwent incomplete radiotherapy and two patients were lost to follow-up. The median age of patients was 51 years (range, 33 to 65 years). Preoperative staging was performed according to the guidelines issued by the International Federation of Gynecology and Oncology (FIGO) (stage IB: 16 patients, stage IIA: 10 patients, stage IIB: 9 patients). Patient and tumor characteristics are shown in Table 1. Two of 35 patients had an involved vaginal resection margin. PAN and CIN involvement was found in pathological specimens in 24 and 11 patients, respectively.
EFRT was delivered using a megavoltage photon beam through parallel-opposed ports or the four-field box technique. The upper margin of the EFRT port was the T12-L1 junction and the lower margin was 2 cm below the vaginal cuff. The lateral margin of the pelvic portion of the field was 1.5 cm to 2 cm lateral to the widest margin of the bony pelvis; the lateral margin of the para-aortic portion of the field was placed at the transverse processes of the vertebrae. The anterior and posterior margins of the pelvic portion of the lateral fields were the anterior aspect of the symphysis pubis and the posterior margin was the S2-S3 interspace, respectively. Anterior blocks were placed approximately 2 cm in front of the vertebral bodies and the posterior blocks split the vertebral bodies. Radiotherapy was delivered at a dose of 1.8 Gy per fraction once daily, five days per week. The median doses to the whole pelvis and paraaortic field were 50.4 Gy and 45 Gy, respectively. For two patients with a positive vaginal resection margin, intracavitary radiation was delivered using a Fletcher-Suit unit with 137Cs and was prescribed to 0.5 cm from the surface of the vaginal cuff. The median dose of intracavitary radiation was 34.6 Gy. Of 35 patients, 23 patients received adjuvant CTx. CTx regimens administered during the study period were TC, TP, FP and FAC (T: paclitaxel, C: cyclophosphamide, P: cisplatin, F: 5-fluorouracil, A: doxorubicin). The TC regimen was the most commonly employed regimen (13/23) and the median number of CTx cycles administered was 4 (range, 2 to 7).
After completion of treatment, all 35 patients underwent follow-up with pelvic and digital rectal examinations, a Papanicolaou smear and radiographic studies, if required. The median duration of follow-up was 44 months (range, 9 to 116 months). Overall survival (OS) was defined as the length of time until death, regardless of cause, and the disease-free survival (DFS) was defined as the length of time before the first evidence of recurrence, including loco-regional recurrence or a distant metastasis. Survival analysis was performed using the Kaplan-Meier method. Differences of survival, locoregional relapse (LRR) and patterns of failure were assessed by the log rank test. Prognostic factors were analyzed by the Cox regression model. All p-values were two-sided, and a value of p≤0.05 was considered as statistically significant.
With a median follow-up of 44 months, the 2-year and 5-year OS, DFS, distant failure-free survival (DFFS) and loco-regional failure-free survival (LRFFS) rates were 75%/51%, 70%/51%, 73%/59% and 93%/93%, respectively (Fig. 1). At the time of this analysis, 17 patients (48%) experienced recurrence. Most patients (15/17) had a distant metastasis, and loco-regional failure was observed in three patients with all vaginal recurrences. One patient had both loco-regional recurrence and a distant metastasis. Patterns of failure are summarized in Table 2. The most common metastatic site of a distant metastasis was the supraclavicular lymph node (6/15), and only 1 patient had relapse with a PAN.
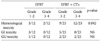
Survival rates were compared according to clinical and pathological factors. The results of the analyses are presented in Table 3. Patients with PAN involvement had lower 5-year DFS (42% vs. 73%, p=0.002) and 5-year DFFS (47% vs 82%, p=0.004) rates. The use of CTx was associated with improved OS, DFS, and DFFS rates. The 5-year OS rates in patients with or without CTx were 61% and 48%, respectively (p=0.004), the 5-year DFS rates were 54% and 38%, respectively (p=0.004), and the 5-year DFFS were 57% and 48%, respectively (p=0.009). Clinicopathological variables were well balanced between the use of POEFRT alone and POEFRT combined with CTx (Table 4). There was a trend of an increasing risk of distant metastasis in patients who did not receive CTx. Seven of 12 patients (58%) who received POEFRT alone and 8 of 23 patients (35%) who received POEFRT combined with CTx developed distant metastasis.
The presence of complications was estimated by a review of medical records (radiation oncology records and referring notes), and complications were graded using the Radiation Therapy Oncology Group (RTOG) criteria. Acute toxicities are summarized in Table 5. The most common type of toxicity was hematological complication, occurring in 26 patients (74%). Grade 3-4 hematological toxicity was observed more frequently in patients who received POEFRT combined with CTx as compared to patients who received POEFRT alone (52% vs. 17%, p=0.04). Although 8 patients experienced grade 1-2 gastrointestinal (GI) complications (POEFRT alone: 3 patients, POEFRT and CTx: 5 patients), no patient experienced a grade 3-4 GI complication. Grade 3-4 genitourinary (GU) complications were observed in 2 patients treated with POEFRT combined with CTx.
Several factors such as involvement of the parametrium, involved resection margin, a pelvic/para-aortic lymph node metastasis, large clinical tumor diameter, lymphovascular space invasion, and deep stromal invasion are known to be associated with a poor prognosis.1,2 Among these factors, a lymph node metastasis has the most important prognostic significance. Several studies have reported a 5-year survival rate of 90% for patients treated surgically with no evidence of a lymph node metastasis, as compared with rates of 20-60% for patients with a positive pelvic or PAN metastasis.10,11 As cells can sequentially metastasize to lymph node stations, a CIN metastasis may be an independent risk factor for PAN involvement. Hence, POEFRT that includes both the aortic and pelvic areas have been used to reduce recurrence and to improve survival in patients with a CIN and/or PAN metastasis.
The aim of this study was to evaluate treatment outcomes and prognostic factors in patients treated with POEFRT with or without CTx. In this study, the 5-year OS and DFS rates were 51% and 51%, respectively, which results were similar to findings of other studies.6,12 When we analyzed the prognostic factors, the level of the involved lymph node station and administration of CTx were found to be independently predictive of survival. However, other factors such as involvement of the parametrium, involved resection margin, large clinical tumor diameter, lymphovascular space invasion, and deep stromal invasion had no influence on survival. These findings indicate that the tumor burden itself and treatment factors may be more important in patients with a lymph node metastasis located above the common iliac area.
Since Peters et al.13 reported that the addition of concurrent CTx to postoperative radiotherapy was superior to the use of radiation alone in patients with a positive pelvic lymph node and/or positive resection margin and/or parametrium involvement, postoperative concurrent chemoradiotherapy was established as the standard for the treatment of high-risk cervical cancer patients. For this reason, POEFRT combined with CTx might be considered in patients with a pathologically confirmed PAN or CIN metastasis. Contrary to several retrospective studies that have examined the role of radical extended-field radiation therapy with CTx,8,9,14,15 very few studies have investigated the feasibility of POEFRT with CTx.16,17 In our institution, prior to 2000, radiation alone had been mostly employed as a mode of adjuvant therapy. However, since trials have demonstrated the superiority of chemoradiation in high-risk patients, POEFRT combined with CTx has been provided for patients with a CIN and/or PAN metastasis after surgery, and we were able to evaluate treatment outcomes according to the addition of CTx to POEFRT. The administation of CTx was an important prognostic factor that influenced OS, DFS and DFFS in this study. We also anticipated less distant metastases in patients treated with POEFRT combined with CTx, as compared to patients treated with POEFRT alone. There was a trend of an increasing risk of distant metastasis in patients that did not receive CTx. Seven of 12 patients (58%) who received POEFRT alone and 8 of 23 patients (35%) who received POEFRT combined with CTx developed distant metastasis.
Despite the benefit of POEFRT combined with CTx, there is a great concern for complications resulting from this treatment scheme. Toxicity associated with POEFRT alone has been reported to be approximately 0% to 20%.6,14,18-21 However, toxicity will be expected to be higher when CTx is added to POEFRT, mainly due to hematological toxicities. Since we determined the TC regimen to be very efficacious and well tolerated as an adjuvant CTx regimen, the TC regimen has been the most commonly employed regimen in our institution.22 In this study, the most common type of toxicity was a hematological complication, occurring in 26 patients (74%). Patients treated with POEFRT combined with CTx experienced more grade 3-4 hematological toxicity as compared to patients treated with POEFRT alone (52% vs. 17%, p=0.04). However, treatment delay was minimal regardless of the addition of CTx, and hematological toxicities were managed with supportive treatment. In addition, other complications such as GI or GU toxicity were not different between patients treated with POEFRT combined with CTx and patients treated with POEFRT alone.
A limitation of this study was that the investigation was conducted based on retrospective data and the small number of patients were analyzed. Furthermore, various CTx regimens and schedules were employed in this study. As a small number of patients were treated with different regimens and schedules, we were not able to analyze the effect of the respective CTx regimens and schedules on treatment outcomes. However, as there is still controversy regarding which regimen and schedule should be used in an adjuvant setting, we think that these factors would not influence the results of the study.
In conclusion, the use of POEFRT resulted in an excellent loco-regional control rate in patients with a CIN and/or PAN metastasis. The addition of CTx may improve outcomes in patients who have received POEFRT, with higher but manageable toxicity. In addition, considering that a distant metastasis is the most common pattern of failure, maintenance CTx should be intensified to improve survival outcome.
Figures and Tables
Fig. 1
Overall survival (OS) and disease-free survival (DFS) for 35 patients analyzed in this study.

References
1. Petereit DG, Eifel PJ, Thomas GM. Gunderson LL, Tepper JE, editors. Cervical cancer. Clinical radiation oncology. 2007. 2nd ed. Philadelphia, PA: Churchill Livingstone;1323–1357.
2. Sedlis A, Bundy BN, Rotman MZ, Lentz SS, Muderspach LI, Zaino RJ. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: a Gynecologic Oncologic Group study. Gynecol Oncol. 1999. 73:177–183.
3. Stehman FB, Bundy BN, DiSaia PJ, Keys HM, Larson JE, Fowler WC. Carcinoma of the cervix treated with radiation therapy: a multi-variate analysis of prognostic variables in the Gynecologic Oncology Group. Cancer. 1991. 67:2776–2785.
4. Delgado G, Bundy BN, Fowler WC Jr, Stehman FB, Sevin B, Creasman WT, et al. A prospective surgical pathological study of stage I squamous carcinoma of the cervix: a Gynecologic Oncology Group study. Gynecol Oncol. 1989. 35:314–320.
5. Podczaski E, Stryker JA, Kaminski P, Ndubisi B, Larson J, DeGeest K, et al. Extended-field radiation for carcinoma of the cervix. Cancer. 1990. 66:251–258.
6. Grigsby PW, Perez CA, Chao KS, Herzog T, Mutch DG, Rader J. Radiation therapy for carcinoma of the cervix with biopsy-proven positive para-aortic lymph nodes. Int J Radiat Oncol Biol Phys. 2001. 49:7338.
7. Berman ML, Keys H, Creasman W, DiSaia P, Bundy B, Blessing J. Survival and patterns of recurrence in cervical cancer metastatic to periaortic lymph nodes (a Gynecologic Oncology Group study). Gynecol Oncol. 1984. 19:8–16.
8. Varia MA, Bundy BN, Deppe G, Mannel R, Averette HE, Rose PG, et al. Cervical carcinoma metastatic to para-aortic nodes: extended field radiation therapy with concomitant 5-fluorouracil and cisplatin chemotherapy. A Gynecologic Oncology Group study. Int J Radiat Oncol Biol Phys. 1998. 42:1015–1023.
9. Grigsby PW, Lu JD, Mutch DG, Kim RY, Eifel PJ. Twice-daily fractionation of external irradiation with brachytherapy and chemotherapy in carcinoma of the cervix with positive paraaortic lymph nodes: phase II study of the Radiation Therapy Oncology Group 92-10. Int J Radiat Oncol Biol Phys. 1998. 41:817–822.
10. Delgado G, Bundy B, Zaino R, Sevin BU, Creasman WT, Major F. Prospective surgical-pathological study of disease-free interval in patients with stage IB squamous cell carcinoma of the cervix: a Gynecologic Oncology Group study. Gynecol Oncol. 1990. 38:352–357.
11. Stehman FB, Randall ME, Michael H, Morken JV. Hoskins WJ, Perez CA, Young RC, Barakat R, Markman M, Randall M, editors. Uterine cervix. Principles and practice of gynecologic oncology. 2005. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins;761.
12. Lovecchio JL, Averette HE, Donato D, Bell J. 5-year survival of patients with periaortic nodal metastases in clinical stage IB and IIA cervical carcinoma. Gynecol Oncol. 1989. 34:43–45.
13. Peters WA 3rd, Liu PY, Barrett RJ 2nd, Stock RJ, Monk BJ, Berek JS, et al. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000. 18:1606–1613.
14. Saad A, Lo SS, Han I, Keole S, Lee C, Tekyi-mensah S, et al. Radiation therapy with or without chemotherapy for cervical cancer with periaortic lymph node metastasis. Am J Clin Oncol. 2004. 27:256–263.
15. Malfetano JH, Keys H. Aggressive multimodality treatment for cervical cancer with paraaortic lymph node metastases. Gynecol Oncol. 1991. 42:44–47.
16. Hacker NF, Wain GV, Nicklin JL. Resection of bulky positive lymph nodes in patients with cervical carcinoma. Int J Gynecol Cancer. 1995. 5:250–256.
17. Sood BM, Timmins PF, Gorla GR, Garg M, Anderson PS, Vikram B, et al. Concomitant cisplatin and extended field radiation therapy in patients with cervical and endometrial cancer. Int J Gynecol Cancer. 2002. 12:459–464.
18. Vigliotti AP, Wen BC, Hussey DH, Doornbos JF, Staples JJ, Jani SK, et al. Extended field irradiation for carcinoma of the uterine cervix with positive periaortic nodes. Int J Radiat Oncol Biol Phys. 1992. 23:501–509.
19. Gaspar LE, Cheung AY, Allen HH. Cervical carcinoma: treatment results and complications of extended-field irradiation. Radiology. 1989. 172:271–274.
20. Nori D, Valentine E, Hilaris BS. The role of paraaortic node irradiation in the treatment of cancer of the cervix. Int J Radiat Oncol Biol Phys. 1985. 11:1469–1473.
21. Crawford JS, Harisiadis L, McGowan L, Rogers CC. Paraaortic lymph node irradiation in cervical carcinoma without prior lymphadenectomy. Radiology. 1987. 164:255–257.
22. Kim K, Chie EK, Wu HG, Ha SW, Kim JS, Kim IA, et al. Efficacy of paclitaxel and carboplatin as a regimen for postoperative concurrent chemoradiotherapy of high risk uterine cervix cancer. Gynecol Oncol. 2006. 101:398–402.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download