Abstract
Objective
The aim of this study was to ascertain whether all cervical cancer patients who received adjuvant concurrent chemoradiation (CCRT) for high risk of treatment failure after radical hysterectomy are at the same risk of treatment failure, and if not, to propose trial treatment modification.
Methods
Between January 1999 and December 2007, 58 patients with FIGO stage Ib-IIa cervical cancer received adjuvant CCRT due to high risk factors such as positive lymph nodes or positive parametrium, or positive vaginal resection margins. Patients were divided into two Groups. Group A were patients with negative parametrium, negative vaginal resection margins, and only unilateral lymph node metastasis (involved L/N≤2). Group B were those with either bilateral pelvic lymph node involvement, or more than 2 lymph node involvement, or positive parametrium with lymph node involvement.
Results
During a median follow-up period of 34 months (range, 6 to 102 months), 9 patients (15.5%) experienced recurrence; among whom 2 patients (2/28, 7.1%) were Group A, and 7 patients (7/30, 23.3%) were Group B. At 3 years, the estimated progression-free survival rate of all 58 patients was 78.3%, and the overall survival rate was 89.7%. Patients in Group A had significantly better progression-free survival (88.2% vs. 68.2%, p=0.042) and overall survival rate (100% vs. 78.8%, p=0.034) than Group B.
Since the randomized study by the Gynecologic Oncology Group (GOG) in 1991, adjuvant concurrent chemoradiation (CCRT) after radical hysterectomy for cervical cancer has been shown to improve survival of patients with high-risk factors for treatment failure, such as pelvic lymph node metastasis, parametrial invasion, and positive surgical margins. The results published in 1999 by Peters et al.1 showed that in 268 high-risk patients after surgery, the 4-year progression-free survival was significantly greater in the adjuvant concurrent chemoradiotherapy group compared to adjuvant radiotherapy alone group (80% vs. 63%, respectively).
However, several questions still remain regarding the optimal CCRT treatment, such as the regimen, dose, and scheduling of chemotherapy and radiation. Moreover, identification of more specified high-risk group in CCRT-candidate patients would be helpful to improve survival by trial of a new adjuvant treatment modality.
At present, there are several known risk factors associated with high risk for treatment failure. Bilateral positive pelvic lymph nodes portend a less favorable prognosis (22-40%) survival rate than the presence of unilateral pelvic nodes (59-70%).2,3 The presence of more than three positive lymph nodes is accompanied by a 68% recurrence rate, compared with 30% to 50% when three or fewer lymph nodes are positive.4,5 In addition, patients with parametrial spread have a better 5-year survival rate compared to those with negative parametrium. When the parametrium is involved and pelvic lymph nodes are also positive, the 5-year survival rate falls from 39% to 42%.6,7
In the present study, we divided the patients into two risk Groups, because disparate prognosis has been observed among the above subcategories. In each Group, prognosis and patterns of recurrence were compared, and the efficacy of adjuvant chemoradiotherapy was evaluated.
Between January 1999 and December 2007, 255 patients with histologically confirmed with invasive carcinoma of the uterine cervix underwent radical hysterectomy and pelvic lymphadenectomy with or without paraaortic lymphadenectomy at the Department of Obstetrics and Gynecology, Ajou University School of Medicine. Eligible patients were those with FIGO stage Ib-IIa with high risk factors such as positive lymph nodes or positive parametrium, or positive vaginal resection margins. A total of 58 patients were eligible for this study. The Institutional Review Board approved this study.
Patients were divided into two Groups according to risk factors. The Group A were patients with negative parametrium, negative vaginal resection margins, and only unilateral lymph node metastasis, which numbered not more than two. The Group B had either bilateral pelvic lymph node involvement or more than 2 lymph node8 involvement, or positive PM with lymph node involvement. The recurrence and survival rates of the two Groups of patients were compared.
All 58 patients underwent radical hysterectomy with bilateral pelvic lymphadenectomy with or without paraaortic lymphadenectomy, and all patients received concurrent chemoradiation. The first anticancer chemotherapy cycle was initiated within 2-3 weeks after surgery and then repeated for a total of four cycles at 4-week intervals. Each chemotherapy cycle consisted of cisplatin (70 mg/m2) on day 1 of each cycle, continuous infusion of 5-FU (1000 mg/m2/day) from days 2 to 5, and concurrent chemotherapy and radiotherapy during the second and third cycles. Radiotherapy of the pelvis did not commence at the beginning of the first chemotherapy cycle but at the beginning of the second cycle in order to avoid wound disruption. Each patient received external beam radiation therapy (EBRT), utilizing a 15MV linear accelerator (CLINAC 2000C/D, Varian), to the whole pelvis for a total dose of 45 Gy. The daily fraction size was 1.8 Gy, administered 5 times per week. Four-field box technique was used to spare the small bowel anterior to the iliac nodes. The superior border of the pelvic portal was at the L4-L5 interspace to include all the external iliac and hypogastric lymph nodes. The fields were extended to the T12-L1 interspace for coverage of the paraaortic nodes in cases with high pelvic nodes involvement or paraaortic node involvement. For patients with positive parametria and/or positive surgical margins, barchytherapy of 28 Gy, with 4 Gy per fraction, was administered to boost doses to the upper vaginal or parametrial tissues. After completion of all whole treatment, the patients were followed every 3 months during the first 2 years, and every 6 months thereafter. Clinical examination, vaginal stump cytology (and/or biopsy), chest x-ray, and abdominopelvic MRI were performed. Patients with recurrent disease were managed with cisplatin-based salvage chemotherapy.
Overall survival was measured from the date of radical hysterectomy to the date of death, or for living patients, to the date of last follow up. Disease-free survival was measured from the date of radical hysterectomy to the date of detection of recurrence. Side effects during chemotherapy were assessed according to the GOG toxicity criteria. Late toxicity of radiation was assessed using the Late Radiation Morbidity Scoring Scheme of the Radiation Therapy Oncology Group.
Statistical analysis was performed by linear association and independent sample test. The overall and progression-free survival curves were calculated by the Kaplan-Meier method. p values less than 0.05 were considered statistically significant. Analyses were performed using SPSS ver. 12.0k (SPSS Inc., Chicago, USA).
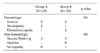
Between January 1999 to December 2007, 58 patients with early stage cervix cancer received postoperative adjuvant concurrent chemoradiation after radical hysterectomy and were enrolled in this study. Table 1 shows the patients' characteristics.
The median age was 45 years (range, 32 to 70 years). The number of patients according to each FIGO stage was 49 in stage IB1 (84.5%), 2 in stage IB2 (3.5%), and 7 in stage IIA (12%). The histology was squamous cell carcinoma in 42 patients (72.4%) and other cell types in 16 patients (27.6%). The number of patients in Group A was 28, and that of Group B was 30. There was no statistical difference in terms of age, histopathologic distribution, and tumor size when compared each other. But patients with stage IIa were all in Group B (Table 1).
A total of 53 (91.3%) patients completed 4 cycles of planned chemotherapy, while 3 patients completed 3 cycles and 2 patients completed 2 cycles only. Reasons for discontinuation of chemotherapy were severe leukopenia, severe nausea and vomiting, poor performance status, and refusal of further chemotherapy by the patient (Table 2).
Seven (12.1%) out of the 58 patients developed grade 2 gastrointestinal toxicity induced by radiotherapy, and responded to conservative management such as diet modification or corticosteroid therapy.
During a median follow-up period of 34 months (range, 6 to 102 months), 9 patients (15.5%) experienced recurrence, of whom 2 patients (7.1%) were in Group A, and 7 patients (23.3%) were in Group B (all 9 patients with Stage Ib disease).
The sites of failure were mainly distant recurrences (Table 3).
At 3 years, the estimated progression-free survival rate of all 58 patients was 78.3% (95% CI, 65-91) (Fig. 1A), and the overall survival rate was 89.7% (95% CI, 79-99)(Fig. 1B). Group A had significantly better 3-year progression-free survival than Group B (88.2% vs. 68.2%, p=0.042) (Fig. 2A), and 3-year overall survival rate (100% vs. 78.8%, p=0.034) (Fig. 2B).
Concurrent chemoradiation is the standard adjuvant treatment of choice in early stage disease with high risk for recurrence such as positive pelvic lymph nodes, positive parametrial extension, or positive vaginal resection margins at the completion of radical hysterectomy.1 It is also a primary treatment of choice in locally advanced stage disease.9 The inclusion of 3 cycles of cisplatin plus 5-FU chemotherapy substantially reduced both local and distant recurrences of cervical cancer, leading to higher overall and disease-free survival rates. Although chemotherapy increased the hematologic toxicity, this effect was reversible and the incidence of late side effects was similar in the chemoradiation and radiation only groups. We also reported manageable side effects in our previous report.10
Among several high risk factors, lymph node metastasis has been one of the strongest prognostic factors in patients with cervical cancer.11,12 Lymph node status is an important factor when deciding which treatment is appropriate. As for the number of positive nodes, the prognostic significance of this factor is controversial. Some reports did not find that it correlated significantly with prognosis7,13 while others reported contrasting results.8,14,15 Also, other nodal characteristics, such as laterality of positive nodes, common iliac node involvement, and paraaortic lymph node metastasis, were found to be independent prognostic factors in several reports.11,16
With regard to results of adjuvant CCRT, an intergroup trial involving the Gynecologic Oncologic Group, the Southwestern Oncology Group, and the Radiation Therapy Oncology Group reported that postoperative concurrent chemradiation had 4-year disease free survival (DFS) of 81%.17 In this study, DFS of the total 58 patients was 78.3%, which corresponds to the interGroup result. But when the patients were divided into two groups, the DFS was significantly different (Group A 88.2% vs. Group B 68.2%, p=0.042). Five patients in Group B had disease recurrence within 9 months, and the sites of recurrence were mainly distant recurrences. The survival difference observed in the present study may be possibly due to more prominent micrometastases in the Group B patients. This hypothesis can be supported from a report that observed pelvic lymph node involvement persisted in about 16% of patients after primary chemoradiation for locally advanced cervical cancer.18
Recently Choi et al.19 reported a phase II study of consolidation chemotherapy after concurrent chemoradiation in locally advanced cervical cancer, based on Wong et al's hypothesis that too short a duration of chemotherapy may not effectively eradicate micrometastases.20 The aim of the consolidation chemotherapy was the complete eradication of potential undetected micrometastases. Thirty patients (30/32, 94%) received 3 more cycles of consolidation chemotherapy (5-FU+ cisplatin, total 6 cycles). Consolidation chemotherapy after CCRT was well tolerated in general and led to an encouraging survival rate.19 Compared with a 3 year PFS rate of 58-69% with CCRT alone,21-23 the trials by Choi et al.19 showed a 3 year PFS of 83%. Although 3 more cycles of consolidation chemotherapy after CCRT has not yet been validated in randomized controlled trial, it is our opinion that this may be applicable for such patients as in Group B for enhancing the survival rate.
Although there are some limitations in this study due to the small number of patients and its retrospectiveness, the survival difference observed in this study suggests that we should pursue more effective treatment for the patients with higher risk for treatment failure (bilateral pelvic lymph node involvement, more than 2 lymph node involvement, positive PM with lymph node involvement). For enhancement of survival of patients with very high risk Group such as those in Group B of our study, it is our opinion that the concept of consolidation chemotherapy (such as 2-3 more cycles of 5-FU+cisplatin) after primary CCRT for locally advanced cervical cancer may be extended to the area of adjuvant treatment after radical hysterectomy. This hypothesis would be worthy of a prospective phase II study for confirmation.
Figures and Tables
 | Fig. 1(A) Kaplan-meier estimates of disease-free survival curve for all the 58 patients who were treated with adjuvant concurrent chemoradiation after radical hysterectomy. (B) Kaplan-Meier estimates of overall survival curve for all the 58 patients who were treated with adjuvant concurrent chemoradiation after radical hysterectomy. |
 | Fig. 2(A) Comparison of Kaplan-Meier estimates of disease-free survival curve between Group A and B (88.2% vs. 68.2%, p=0.042). (B) Comparison of Kaplan-Meier estimates of overall survival curve between Group A and B (100% vs. 78.8%, p=0.034). |
References
1. Peters WA 3rd, Liu PY, Barrett RJ 2nd, Stock RJ, Monk BJ, Berek JS, et al. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000. 18:1606–1613.
2. Piver MS, Chung WS. Prognostic significance of cervical lesion size and pelvic node metastases in cervical carcinoma. Obstet Gynecol. 1975. 46:507–510.
3. Hsu CT, Cheng YS, Su SC. Prognosis of uterine cervical cancer with extensve lymph node metastases: special emphasis on the value of pelvic lymphadenectomy in the surgical treatment of uterine cervical cancer. Am J Obstet Gynecol. 1972. 114:954–962.
4. Nahhas WA, Sharkey FE, Whitney CW, Husseinzadeh N, Chung CK, Mortel R. The prognostic significance of vascular channel involvement and deep stromal penetration in early cervical carcinoma. Am J Clin Oncol. 1983. 6:259–264.
5. Martimbeau PW, Kjorstad KE, Iversen T. Stage IB carcinoma of the cervix, the Norwegian Radium hospital: II. Results when pelvic nodes are involved. Obstet Gynecol. 1982. 60:215–218.
6. Van Nagel JR Jr, Donaldson ES, Parker JC, Van Dyke AH, Wood EG. The prognostic significance of cell type and lesion size in patients with cervical cancer treated by radical surgery. Gynecol Oncol. 1977. 5:142–151.
7. Delgado G, Bundy B, Zaino R, Sevin BU, Creasman WT, Major F. Prospective surgical-pathological study of disease-free interval in patients with stage IB squamous cell carcinoma of the cervix: a Gynecologic Oncology Group study. Gynecol Oncol. 1990. 38:352–357.
8. Inoue T, Morita K. The prognostic significance of number of positive nodes in cervical carcinoma stages IB, IIA, and IIB. Cancer. 1990. 65:1923–1927.
9. Morris M, Eifel PJ, Lu J, Grigsby PW, Levenback C, Stevens RE, et al. Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high-risk cervical cancer. N Engl J Med. 1999. 340:1137–1143.
10. Ryu HS, Chun M, Chang KH, Chang HJ, Lee JP. Postoperative adjuvant concurrent chemoradiotherapy improves survival rates for high-risk, early stage cervical cancer patients. Gynecol Oncol. 2005. 96:490–495.
11. Morice P, Castaigne D, Pautier P, Rey A, Haie-Meder C, Leblanc M, et al. Interest of pelvic and paraaortic lymphadenectomy in patients with stage IB and II cervical carcinoma. Gynecol Oncol. 1999. 73:106–110.
12. Michel G, Morice P, Castaigne D, Leblanc M, Rey A, Duvillard P. Lymphatic spread in stage Ib and II cervical carcinoma: anatomy and surgical implications. Obstet Gynecol. 1998. 91:360–363.
13. Samlal RA, van der Velden J, Schilthuis MS, Gonzalez Gonzalez D, Ten Kate FJ, Hart AA, et al. Identification of high-risk Groups among node-positive patients with stage IB and IIA cervical carcinoma. Gynecol Oncol. 1997. 64:463–467.
14. Tinga DJ, Timmer PR, Bouma J, Aalders JG. Prognostic significance of single versus multiple lymph node metastases in cervical carcinoma stage IB. Gynecol Oncol. 1990. 39:175–180.
15. Stock RG, Chen AS, Flickinger JC, Kalnicki S, Seski J. Node-positive cervical cancer: impact of pelvic irradiation and patterns of failure. Int J Radiat Oncol Biol Phys. 1995. 31:31–36.
16. Lin HH, Cheng WF, Chan KW, Chang DY, Chen CK, Huang SC. Risk factors for recurrence in patients with stage IB, IIA, and IIB cervical carcinoma after radical hysterectomy and postoperative pelvic irradiation. Obstet Gynecol. 1996. 88:274–279.
17. Wertheim MS, Hakes TB, Daghestani AN, Nori D, Smith DH, Lewis JL Jr. A pilot study of adjuvant therapy in patients with cervical cancer at high risk of recurrence after radical hysterectomy and pelvic lymphadenectomy. J Clin Oncol. 1985. 3:912–916.
18. Houvenaeghel G, Lelievre L, Rigouard AL, Buttarelli M, Jacquemier J, Viens P, et al. Residual pelvic lymph node involvement after concomitant chemoradiation for locally advanced cervical cancer. Gynecol Oncol. 2006. 102:74–79.
19. Choi CH, Lee JW, Kim TJ, Kim WY, Nam HR, Kim BG, et al. Phase II study of consolidation chemotherapy after concurrent chemoradiation in cervical cancer: preliminary results. Int J Radiat Oncol Biol Phys. 2007. 68:817–822.
20. Wong LC, Choo YC, Choy D, Sham JS, Ma HK. Long-term follow-up of potentiation of radiotherapy by cis-platinum in advanced cervical cancer. Gynecol Oncol. 1989. 35:159–163.
21. Eifel PJ, Winter K, Morris M, Levenback C, Grigsby PW, Cooper J, et al. Pelvic irradiation with concurrent chemotherapy versus pelvic and para-aortic irradiation for high-risk cervical cancer: an update of radiation therapy oncology Group trial (RTOG) 90-01. J Clin Oncol. 2004. 22:872–880.
22. Whitney CW, Sause W, Bundy BN, Malfetano JH, Hannigan EV, Fowler WC Jr, et al. Randomized comparison of fluorouracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage IIB-IVA carcinoma of the cervix with negative para-aortic lymph nodes: a Gynecologic Oncology Group and Southwest Oncology Group study. J Clin Oncol. 1999. 17:1339–1348.
23. Rose PG, Bundy BN, Watkins EB, Thigpen JT, Deppe G, Maiman MA, et al. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med. 1999. 340:1144–1153.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download