Abstract
Objective
To examine the correlation among the preoperative serum levels of five biomarkers presumed to be useful for early detection of epithelial ovarian cancer and evaluate the relationships between serum levels of these five biomarkers and epithelial ovarian cancer stage.
Methods
We analyzed 56 newly diagnosed epithelial ovarian cancer patients. Preoperative serum levels of leptin, prolactin, osteopontin (OPN), insulin-like growth factor-II, and CA-125 were determined by ELISA. We also examined the correlation between the serum levels of the biomarkers and ovarian cancer stage. Significant differences in the mean serum levels of two proteins, leptin and CA-125, were observed between stage subsets.
Results
There was a significant negative correlation between prolactin and leptin and a significant positive correlation between prolactin and OPN. Of the five biomarkers, only the mean serum CA-125 level showed a significant positive correlation with cancer stage (Spearman ρ=0.24, p<0.01). OPN showed a marginally significant positive correlation with stage (Spearman ρ=0.14, p=0.07).
Conclusion
We demonstrated the relationship between five biomarkers in epithelial ovarian cancer. These tumor markers may be useful in screening for ovarian cancer, in characterizing disease states, and in developing therapeutic interventions targeting these marker proteins. Large-scale studies that include potential confounding factors and modifiers are necessary to more accurately define the value of these novel biomarkers in ovarian cancer.
Ovarian cancer is the leading cause of death from gynecological malignancy in most developed countries, although it is still relatively infrequent in developing countries. In the USA, ovarian cancer is the fifth leading cause of cancer-related death among women and is the leading cause of gynecological cancer deaths, accounting for nearly 16,000 deaths in 2008.1
The high mortality rate of ovarian cancer is attributable mainly to the lack of effective screening and the dearth of symptoms and signs in the early stages. Indeed, only about 20% of patients are diagnosed when the tumor is still confined to the pelvic cavity. In these stage I or II patients, the 5-year survival rate ranges from 70 to 95%, depending on the stage and grade of tumor differentiation.2,3 In contrast, the 5-year overall survival rate of patients diagnosed beyond stage III is less than 20%.4 Although recent advances in treatment have slightly improved survival, the overall survival rate of ovarian cancer has not increased significantly over the last 20 years. Therefore, the most reasonable strategy for improving the survival rate of ovarian cancer patients is to develop effective early detection techniques.
A recent study characterized a panel of four biomarkers, leptin, prolactin, osteopontin (OPN), and insulin-like growth factor-II (IGF-II), associated with stage I and II ovarian cancer, with 95% sensitivity and 94% specificity for ovarian cancer detection. These results are better than those obtained with other currently available tests. Leptin, prolactin, OPN, and IGF-II were selected as biomarkers because they are all related to the normal physiology of the ovaries, and show significant differences in expression between healthy individuals and ovarian cancer patients.5
The levels of expression of these biomarkers are maintained by a delicate balance between each of the cellular components of the ovary in physiologic conditions. In the process of ovarian carcinogenesis, the development of abnormal cells may alter and disrupt this intercellular communication, resulting in the abnormal expression of these biomarkers. We hypothesized that there may be interrelations between these biomarkers in the context of ovarian cancer. The aberrant expression of these biomarkers may occur not only in the process of tumorigenesis, but also during tumor progression and metastasis.
In the present study, we used enzyme-linked immunosorbent assays (ELISAs) to evaluate the correlation between the mean serum levels of the four biomarkers mentioned above and of CA-125, a well-known ovarian cancer tumor marker, in ovarian cancer patients. We also examined the correlation between these biomarkers and the ovarian cancer stage.
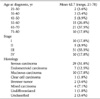
The serum samples used in this study were collected at Kangwon National University Hospital (Chuncheon, Kangwon, Korea) between 1 June 2001 and 31 May 2008. The study group included women newly diagnosed with epithelial ovarian cancer. The eligibility criteria for inclusion were as follows: untreated, newly diagnosed epithelial ovarian cancer, availability of samples prior to surgical intervention, and age 18 years or older. Patients with a previous history of ovarian or fallopian tube cancer; other cancer diagnosed within the 5 years prior to sample collection; or currently undergoing chemotherapy with evidence of ovarian, fallopian, or primary peritoneal carcinoma were excluded. Informed consent was obtained according to the guidelines of our hospital Institutional Review Board. Of the 56 patients with epithelial ovarian cancer, 15 and 41 patients were diagnosed with stage I/II and stage III/IV disease, respectively. Data regarding diagnosis, staging, and histology were acquired by reviewing the medical records. The clinical and histological characteristics of the patients are summarized in Table 1.
Peripheral blood samples were collected preoperatively from women who were scheduled for surgery due to a suspicious pelvic mass, at the Department of Obstetrics and Gynecology of Kangwon National University Hospital. The time interval between serum specimen collection and surgery ranged from 1 to 35 days. Of the 438 samples collected between June 2001 and May 2008, 56 samples were classified as newly diagnosed epithelial ovarian cancer and were included in this study (stages I-IV and patient age, 21 to 78 years). Peripheral blood samples (10 ml) were obtained from each individual. The serum was separated by centrifugation at 800×g for 10 min, divided into aliquots, and stored at -80℃ in the serum bank at Kangwon National University School of Medicine until analysis.
Serum analyses were performed using ELISA kits for each of the five analytes (Diagnostic Systems Laboratories, Webster, TX; Assay Designs, Ann Arbor, MI, USA), according to the respective manufacturer's instructions. The results were read on a Sunrise microplate absorbance reader (Tecan, Durham, NC, USA) with appropriate baseline correction for each assay. The concentrations were determined using a linear standard curve constructed by plotting the mean absorbance against known concentrations of reference standards for each marker.
The Kruskall-Wallis test was used to compare the preoperative mean serum levels of each biomarker between stage subsets. For the biomarkers that showed statistically significant differences, the Mann-Whitney U test was used for multiple comparisons among the individual stage subsets. ANOVA with post hoc analysis was not performed because the relatively small number of patients in the stage I, stage II, and stage IV subsets makes it invalid in this study.
Correlation between the five biomarkers was assessed using Pearson's correlation analysis. Biomarkers that showed significant correlation were analyzed by linear regression to determine the working relationships between the biomarkers. The Spearman correlation coefficient was used to determine the correlation between the serum levels of the biomarkers and the cancer stage, determined according to the International Federation of Gynecology and Obstetrics (FIGO) criteria. SPSS ver. 10.1.3 (SPSS Inc., Chicago, IL, USA) was used for data management and all statistical analyses. All results are given as two-tailed p-values, and p<0.05 was considered statistically significant.
We used ELISAs to analyze the concentrations of five protein biomarkers (leptin, prolactin, OPN, IGF-II, and CA-125) in serum samples from 56 untreated epithelial ovarian cancer patients. This subset of proteins was selected for the analysis because they show significant differences in expression between healthy individuals and ovarian cancer patients, and because they have been proposed as novel markers used in combination for the early detection of ovarian cancer. Fig. 1 shows the mean serum levels of the five biomarkers according to cancer stage. The serum level of CA-125 increased consistently with stage. However, the other four biomarkers (leptin, prolactin, OPN, and IGF-II) showed no consistent correlation with stage.
We compared the mean serum level of each biomarker among the four stage subsets. For the biomarkers that showed statistically significant differences, multiple comparisons among the individual stage subsets were performed. As shown in Table 2, two proteins (leptin and CA-125) showed a significant difference in mean serum level between stage subsets. The mean levels of leptin at each stage were 10.5±13.2 (stage I), 3.9±5.9 (stage II), 8.9±14.2 (stage III), and 6.5±16.2 ng/ml (stage IV); the mean level at stage III was significantly higher than that at stage II. The mean serum levels of CA-125 were 4.5±5.8 (stage I), 13.1±32.6 (stage II), 29.6±50.9 (stage III), and 37.0±65.9 IU/ml (stage IV), with the levels at stages III and IV being significantly higher than those at stages I and II. The other three biomarkers (prolactin, OPN, and IGF-II) showed no significant differences between stage subsets.
Pearson's correlation analysis was performed to determine whether there were correlations between the serum levels of biomarkers in epithelial ovarian cancer patients. There was a significant negative correlation between prolactin and leptin and a significant positive correlation between prolactin and OPN. No significant correlation was found between any of the other biomarkers (Table 3). Linear regression analysis of the biomarkers that showed statistically significant correlation revealed a low degree of correlation for each pair (prolactin and leptin, r2=0.033; prolactin and OPN, r2=0.038) (Fig. 2).
Fifty-six cases of epithelial ovarian cancer were analyzed using Spearman's correlation analysis to determine the relationships between cancer stage and the serum levels of the five biomarkers. As shown in Table 4, among the five biomarkers examined, only CA-125 showed a definite significant positive correlation with stage (Spearman ρ=0.24, p<0.01). OPN showed a marginally significant positive correlation with stage (Spearman ρ=0.14, p=0.07). Thus, the serum levels of CA-125 and OPN showed an increasing trend with higher cancer stage. The other three biomarkers (leptin, prolactin, and IGF-II) showed no significant correlation with cancer stage.
A woman's estimated risk of developing ovarian cancer in her lifetime is 1 in 70 or 1.4%.1 Unfortunately, no fully effective mass screening method for early ovarian cancer has yet been developed. The currently available methods, such as abdominal and transvaginal ultrasonography, color flow Doppler, and CA-125, are not specific enough for detecting early, treatable ovarian cancer through population screening.6 Therefore, the disease is detected at an advanced stage in most patients, being confined to the ovaries at diagnosis in fewer than 30% of cases. The lack of effective screening tools is one of the main reasons for the poor prognosis of this disease. Therefore, the development of a sensitive and specific method for early detection of ovarian cancer is a priority as a means of improving the treatment outcome of this disease.
Currently, one of the most common screening tests for epithelial ovarian cancer involves the use of biomarkers. Biomarkers have been applied in the management of epithelial ovarian cancer in several different ways, including predicting primary disease at an early stage, distinguishing malignant from benign pelvic masses, monitoring responses to treatment, and estimating prognosis. A number of proteins present in either blood or urine have been identified as specific markers for epithelial ovarian cancer.7-9 Among them, CA-125 has attracted the most attention to date. However, no single protein has provided adequate sensitivity and specificity as a screening biomarker. A recent study using four biomarkers (leptin, prolactin, OPN, and IGF-II) indicated 95% sensitivity and 94% specificity for ovarian cancer detection, which are higher than those of other currently available tests.5
In this study, we analyzed the serum levels and relationships between five biomarkers, i.e., leptin, prolactin, OPN, IGF-II, and CA-125, in epithelial ovarian cancer. These proteins were selected as early detection markers for two reasons. First, they showed significant differences in expression between healthy individuals and epithelial ovarian cancer patients.5 The serum levels of prolactin, OPN, and CA-125 were significantly higher in epithelial ovarian cancer patients, whereas the other two biomarkers (leptin and IGF-II) were the opposite. Second, most of these proteins showed anti-apoptotic or proliferative effects on ovarian cancer cells.10-14
All five biomarkers evaluated in the present study have been suggested as potential tumor markers by other research groups, although they have not been tested previously as a set. Leptin is a 16-kDa hormone secreted as a product of the ob gene. Leptin showed consistent angiogenic and proliferative potential in an in vitro study but presented a complex and paradoxical picture in a clinical study.11 Several reports have documented an association between cancer risk and higher leptin levels, as measured prospectively.15,16 Normal or elevated leptin levels have been documented in analyses of individuals performed >1.5 y before the detection of colorectal or breast cancer. However, serum leptin levels measured at the time of diagnosis in patients with gastrointestinal and other cancers were lower than the control levels.17 Thus, the levels of leptin in serum may be significantly affected by the timing of serum collection relative to disease onset. Leptin signaling is transduced mainly by the signaling pathway that involves signal transducer and activator of transcription (Jak/STAT), mitogen-activated protein kinase (MAPK), and phosphoinositide 3-kinase (PI3K).18
Prolactin was originally defined as a peptide hormone that stimulates lactogenesis; it is secreted by the anterior pituitary gland. A number of recent studies have shown that prolactin is an important hormone/growth factor in female reproductive organs, including the ovaries. In addition, it is produced in breast, prostate, and colorectal cancers, where it is involved in the progression of these cancers in an autocrine/paracrine manner.19 Prolactin receptor mRNA is found in most ovarian cancer cell lines and inhibits apoptosis of ovarian cancer cells in vitro.10 This anti-apoptotic effect is mediated by stimulation of the PI3K-Akt pathway and is also associated with Bcl-2 family proteins in human breast cancer cells.20
OPN is a 44-kDa glycophosphoprotein present in all body fluids, extracellular matrix components, and the proteinaceous matrix of mineralized tissues. OPN was shown to be over expressed in tumors and serum of women newly diagnosed with an ovarian tumor.13 OPN levels are also elevated in breast, prostate, lung, colon, pancreatic, and ovarian cancers and in multiple myelomas.21 The IGFs are polypeptides that are important in cellular proliferation, differentiation, and apoptosis. They are regulated by a family of binding proteins (IGFBPs), six of which have been identified to date, that can both attenuate and stimulate the mitogenic effects of the IGFs by controlling type I IGF receptors. The expression of the IGF-II gene is associated with the development of breast, colon, and prostate cancers. In addition, IGF-II expression is elevated in ovarian cancer in comparison with normal ovarian tissues. Accumulating evidence implicates IGFs in carcinogenesis and tumor progression.22 CA-125 is a tumor-associated antigen, identifiable by the highly specific murine monoclonal antibody IgG1 OC 125, that is present in more than 80% of ovarian cancer patients and in only 1% of healthy women. It is currently the most commonly used single ovarian cancer tumor marker.
In the present study, we reviewed the correlations between preoperative serum levels of these biomarkers in ovarian cancer. Previous reports on the relationships between tumor markers in ovarian cancer have been confined to the relationships between CA-125 and other tumor markers.23 Our study is of value because it provides information about the relationships between diverse potential biomarkers in ovarian cancer. This study showed a significant negative correlation between prolactin and leptin, and a significant positive correlation between prolactin and OPN, although neither correlation was strong (r2=0.033 and r2=0.038, respectively). At present, it is difficult to explain the biological basis for these correlations, and it is possible that they are incidental. However, because these potential biomarkers of ovarian cancer showed significant changes in serum levels during carcinogenesis, there may be an underlying pathophysiological relationship between them. Interestingly, the serum concentrations of prolactin and leptin were negatively correlated, yet they share the same signal transduction pathway, the PI3K-Akt pathway. The only other biomarker correlation was the positive correlation between prolactin and OPN levels. In contrast to our results, a previous study documented a significant relationship between serum levels of OPN and CA-125 in ovarian cancer patients (Spearman ρ=0.31, p<0.01).24
Only CA-125 showed a significant positive correlation with cancer stage (Spearman ρ=0.24, p<0.01). Our result corresponds well with those of previous studies on CA-125. Elevated overall CA-125 levels have been found in 75 to 90% of ovarian cancer patients, and elevated serum CA 125 levels were present in 51, 71, 91, and 98% of patients with FIGO stage I, II, III, and IV tumors, respectively.25-28 This suggests a positive correlation between the preoperative serum CA-125 level and the FIGO stage. In the case of OPN, there was a marginally significant correlation with cancer stage in our study (Spearman ρ=0.14, p=0.07). Serum OPN is thought be derived from the primary tumor or the ovarian stroma in ovarian cancer, because the serum level of OPN is higher before debulking surgery compared with the level during the postoperative period. In addition, a previous study indicated that the serum OPN level was significantly correlated with the bulk of diseased tissue in ovarian cancer.24 As there are significant correlations between tumor size and stage and between tumor size and OPN in ovarian cancer,29 it is likely that there is a meaningful relationship between OPN and the cancer stage. Further studies are necessary to characterize this relationship.
None of the other three biomarkers, leptin, prolactin, and IGF-II, showed a significant correlation with stage. As noted above, controversy remains regarding the association between serum leptin levels and the onset of disease, and there are no published data addressing this putative relationship. The association between the serum level of IGF-II and ovarian cancer is also complicated, because the effects of IGF-II are regulated mainly through the paracrine or autocrine system in local tissues, rather than via an endocrine function, and because the serum level of IGF-II is markedly affected by IGFBP.
Our paper has several limitations, including its retrospective nature and small sample size. Diagnostic accuracy, including sensitivity, specificity, positive predictive value (PPV), and negative predictive values (NPV) of each biomarker and in combination was not assessed. Because this study was done retrospectively, comparable normal control group necessary to evaluate the validity of biomarkers was unavailable. But, there are some previous studies validating the diagnostic accuracy of these biomarkers. According to Visintin et al., none of the above biomarkers by themselves were significant enough to differentiate healthy versus cancer cells. However, the combination of the these biomarkers provided a better differentiation than CA-125.30 In another study, the combination of 6 biomarkers (5 biomarkers mentioned above and macrophage inhibitory factor) yielded 95.3% sensitivity and 99.4% specificity.31
Within these limitations, however, our study showing the relationships between five biomarkers in epithelial ovarian cancer is meaningful. We assumed that the presence of abnormal cells may alter and disrupt the intercellular communication, which is maintained by a delicate balance between each of the cellular components of the ovary. We tried to find out whether there is consistent interrelation between biomarkers in the context of ovarian cancer. The biomarkers identified in this study may not only represent factors produced by the tumor, but also represent the organ's response to the presence of neoplastic cells. Significant levels of biomarkers could only be detected in peripheral blood at later stages of tumor development; however, the body is able to recognize and respond to early stages of the tumorigenicity. In this sense, we attempted to ascertain the correlation between the biomarkers and ovarian cancer stage. Larger scaled further studies are needed to explore these interrelations more definitely.
In summary, we demonstrated the relationships between five biomarkers in epithelial ovarian cancer. A great deal remains to be determined regarding the relationships and putative oncogenic roles of these five biomarkers in epithelial ovarian cancers. These tumor markers may be useful in screening for ovarian cancer, in characterizing disease states, and in developing therapeutic interventions targeting these marker proteins.
Figures and Tables
Fig. 1
Schematic of the mean biomarker levels by FIGO stage. Only the serum level of CA-125 showed a consistent increase with stage.

Fig. 2
Linear regression curves between the biomarkers that showed significant correlations on Pearson's correlation analysis. (A) Prolactin and leptin. (B) Prolactin and osteopontin.

References
1. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008. 58:71–96.
2. Berchuck A, Elbendary A, Havrilesky L, Rodriguez GC, Bast RC Jr. Pathogenesis of ovarian cancers. J Soc Gynecol Investig. 1994. 1:181–190.
3. Schwartz PE. Current diagnosis and treatment modalities for ovarian cancer. Cancer Treat Res. 2002. 107:99–118.
4. Rapkiewicz AV, Espina V, Petricoin EF 3rd, Liotta LA. Biomarkers of ovarian tumours. Eur J Cancer. 2004. 40:2604–2612.
5. Mor G, Visintin I, Lai Y, Zhao H, Schwartz P, Rutherford T, et al. Serum protein markers for early detection of ovarian cancer. Proc Natl Acad Sci U S A. 2005. 102:7677–7682.
6. Menon U, Jacobs IJ. Recent developments in ovarian cancer screening. Curr Opin Obstet Gynecol. 2000. 12:39–42.
7. Chambers AF, Vanderhyden BC. Ovarian cancer biomarkers in urine. Clin Cancer Res. 2006. 12:323–327.
8. Goff BA, Muntz HG. Screenig and early diagnosis of ovarian cancer. Womens Health Prim Care. 2005. 8:262–268.
9. Ye B, Skates S, Mok SC, Horick NK, Rosenberg HF, Vitonis A, et al. Proteomic-based discovery and characterization of glycosylated eosinophil-derived neurotoxin and COOH-terminal osteopontin fragments for ovarian cancer in urine. Clin Cancer Res. 2006. 12:432–441.
10. Asai-Sato M, Nagashima Y, Miyagi E, Sato K, Ohta I, Vonderhaar BK, et al. Prolactin inhibits apoptosis of ovarian carcinoma cells induced by serum starvation or cisplatin treatment. Int J Cancer. 2005. 115:539–544.
11. Choi JH, Park SH, Leung PC, Choi KC. Expression of leptin receptors and potential effects of leptin on the cell growth and activation of mitogen-activated protein kinases in ovarian cancer cells. J Clin Endocrinol Metab. 2005. 90:207–210.
12. Daughaday WH, Rotwein P. Insulin-like growth factors I and II: peptide, messenger ribonucleic acid and gene structures, serum, and tissue concentrations. Endocr Rev. 1989. 10:68–91.
13. Furger KA, Menon RK, Tuck AB, Bramwell VH, Chambers AF. The functional and clinical roles of osteopontin in cancer and metastasis. Curr Mol Med. 2001. 1:621–632.
14. Hudson JD, Shoaibi MA, Maestro R, Carnero A, Hannon GJ, Beach DH. A proinflammatory cytokine inhibits p53 tumor suppressor activity. J Exp Med. 1999. 190:1375–1382.
15. Stattin P, Palmqvist R, Soderberg S, Biessy C, Ardnor B, Hallmans G, et al. Plasma leptin and colorectal cancer risk: a prospective study in Northern Sweden. Oncol Rep. 2003. 10:2015–2021.
16. Stattin P, Soderberg S, Biessy C, Lenner P, Hallmans G, Kaaks R, et al. Plasma leptin and breast cancer risk: a prospective study in northern Sweden. Breast Cancer Res Treat. 2004. 86:191–196.
17. Mantovani G, Maccio A, Mura L, Massa E, Mudu MC, Mulas C, et al. Serum levels of leptin and proinflammatory cytokines in patients with advanced-stage cancer at different sites. J Mol Med. 2000. 78:554–561.
18. Hegyi K, Fulop K, Kovacs K, Toth S, Falus A. Leptin-induced signal transduction pathways. Cell Biol Int. 2004. 28:159–169.
19. Ruffion A, Al-Sakkaf KA, Brown BL, Eaton CL, Hamdy FC, Dobson PR. The survival effect of prolactin on PC3 prostate cancer cells. Eur Urol. 2003. 43:301–308.
20. Peirce SK, Chen WY. Human prolactin and its antagonist, hPRL-G129R, regulate bax and bcl-2 gene expression in human breast cancer cells and transgenic mice. Oncogene. 2004. 23:1248–1255.
21. Fedarko NS, Jain A, Karadag A, Van Eman MR, Fisher LW. Elevated serum bone sialoprotein and osteopontin in colon, breast, prostate, and lung cancer. Clin Cancer Res. 2001. 7:4060–4066.
22. Conover CA, Hartmann LC, Bradley S, Stalboerger P, Klee GG, Kalli KR, et al. Biological characterization of human epithelial ovarian carcinoma cells in primary culture: the insulin-like growth factor system. Exp Cell Res. 1998. 238:439–449.
23. Baron-Hay S, Boyle F, Ferrier A, Scott C. Elevated serum insulin-like growth factor binding protein-2 as a prognostic marker in patients with ovarian cancer. Clin Cancer Res. 2004. 10:1796–1806.
24. Brakora KA, Lee H, Yusuf R, Sullivan L, Harris A, Colella T, et al. Utility of osteopontin as a biomarker in recurrent epithelial ovarian cancer. Gynecol Oncol. 2004. 93:361–365.
25. But I, Gorisek B. Preoperative value of CA 125 as a reflection of tumor grade in epithelial ovarian cancer. Gynecol Oncol. 1996. 63:166–172.
26. Nagele F, Petru E, Medl M, Kainz C, Graf AH, Sevelda P. Preoperative CA 125: an independent prognostic factor in patients with stage I epithelial ovarian cancer. Obstet Gynecol. 1995. 86:259–264.
27. Rossi AC, Di Vagno G, Cormio G, Cazzolla A, Stefanelli S, D'Elia E, et al. A retrospective study of preoperative CA 125 levels in 82 patients with ovarian cancer. Arch Gynecol Obstet. 2004. 269:263–265.
28. Tuxen MK, Soletormos G, Dombernowsky P. Tumor markers in the management of patients with ovarian cancer. Cancer Treat Rev. 1995. 21:215–245.
29. Stratton JF, Pharoah P, Tidy JA, Paterson ME. An analysis of ovarian tumor diameter and survival. Int J Gynecol Cancer. 2000. 10:449–451.
30. Visintin I, Feng Z, Longton G, Ward DC, Alvero AB, Lai Y, et al. Diagnostic markers for early detection of ovarian cancer. Clin Cancer Res. 2008. 14:1065–1072.
31. Kim K, Visintin I, Alvero AB, Mor G. Development and validation of a protein-based signature for the detection of ovarian cancer. Clin Lab Med. 2009. 29:47–55.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download