Abstract
Objective
Ovarian granulosa cell tumors are rare malignancies with a relatively favorable prognosis. However, patients still suffer from disease-related mortality. Therefore, the prognostic factors should be clarified. The purpose of this study was to investigate the clinical and pathologic characteristics related with disease recurrence and mortality in adult type ovarian granulosa cell tumors.
Methods
Eighty surgically staged patients with granulosa cell ovarian tumor treated at the Hacettepe University Hospital between 1982 and 2006 were retrospectively reviewed. Clinical and pathological characteristics were analyzed.
Results
Granulosa cell ovarian tumors accounted for 4.3% of malignant ovarian neoplasms. Mean age was 47.6 years. The most common presenting symptom was abnormal uterine bleeding (53.7%). Endometrial pathology was detected in 51.2% of patients preoperatively. Seventy percent of patients were diagnosed at stage I, and 53.8% of patients received adjuvant treatment. Mean follow-up was 67.5 months. Overall 5-year and 10-year survival was 91% and 86%, respectively. Mean survival was 147.1 months. Recurrence rate was 11.2%. In univariate analysis, advanced stage, advanced age, residual disease after surgery, and need for adjuvant treatment were associated with disease-related mortality and advanced stage disease and absence of initial staging surgery were associated with disease recurrence. However, in multivariate analysis, only initial stage was found to be a significant prognostic factor.
Granulosa cell tumors (GCTs) of the ovary are uncommon, low-grade malignancies accounting for 2-3% of all ovarian cancers.1 They are characterized by prolonged natural history, tendency to late recurrences, and a favorable overall prognosis.1,2 Surgery is the primary choice of treatment which alone provides cure in cases with disease confined to the ovaries. However, platinum-based combined chemotherapy regimen is advised in cases with high-risk factor or more advanced disease.3
The prognostic factors in GCTs include the stage of disease, age of patient at the time of diagnosis, and presence or absence of residual disease after initial surgery.1,4 Nevertheless, the reproducibility of those prognostic factors has been difficult to establish due to the relatively rare occurrence of the disease and lack of standardized management.5
In this retrospective study, we aimed to review the prognostic factors related to recurrence and survival in adult type ovarian granulosa cell tumors. Several articles focusing mainly on the prognosis of ovarian GCTs have been published previously in the literature.6 However, those papers generally included limited numbers of cases and the surgical management were not uniform. The originality of the current article comes from the number of patients which represents one of the largest series published to date and the surgical management which consisted of surgical staging performed uniformly by gynecologic oncologists in a single institute.
Eighty patients with pure adult type granulosa cell tumors of the ovary were identified at Hacettepe University Hospital between 1982 and 2006. Data were retrospectively obtained from patients' charts and gynecologic oncology follow-up forms. Patients' records were reviewed regarding age, gravidity and parity, menopausal status, chief complaint, presence of endometrial pathology, surgical and adjuvant treatment modalities, presence of recurrent disease and mortality, and survival in months.
Data were analyzed using SPSS ver. 11.5 (SPSS Inc., Chicago, IL, USA). The survival curves were constructed using the Kaplan-Meier method and were compared using the log rank test. Univariate and multivariate analyses were performed using Cox's regression model. Pearson's chi-square or Fisher's exact test was used to compare the difference of proportions. A p-value of less than 0.05 was considered significant.
Eighty cases of granulosa cell tumors of the ovary were identified over a period of 25 years. Granulosa cell ovarian tumors accounted for 4.3% (80/1,850) of all malignant ovarian neoplasms during the study period.
The mean age of patients was 47.6 years (range, 17 to 87 years). The mean gravidity and parity were 3.8 and 2.8, respectively. Among the patients 51.2% were premenopausal. The most common presenting symptom was postmenopausal bleeding (27.5%) followed by heavy or irregular menstruation (26.2%). Other presenting symptoms were abdominal or pelvic pain, abdominal distention, acute abdomen, and neurologic symptom due to intracranial metastatic lesions, whereas 10 patients (12.5%) were asymptomatic and were diagnosed during investigations such as ultrasonography or computerized tomography performed for non-gynecologic reasons (Table 1). Of the abdominal masses leading to an acute abdomen, torsion was seen in two and spontaneous rupture was seen in one patient.
Preoperative endometrial evaluation was performed in 43 of 80 patients (53.8%) due to abnormal bleeding. Among them, 32 (40.0%) had simple endometrial hyperplasia without atypia, 4 (5%) had complex endometrial hyperplasia without atypia, 3 (3.8%) had simple endometrial hyperplasia with atypia, 2 (2.5%) had complex endometrial hyperplasia with atypia, while 2 endometrial biopsies showed normal endometrial tissues without hyperplasia or carcinoma. Overall, endometrial pathology was seen in 51.2% of the patients during the preoperative evaluation (Table 1). Among 37 patients without abnormal bleeding and thus without preoperative endometrial evaluation, 8 additional patients had endometrial pathology in the hysterectomy specimens including 1 (1.2%) endometrial cancer in postoperative specimens (Table 2). Endometrial cancer which was confined to the endometrium was detected in a 60-year-old woman with stage III disease who presented with abdominal distention due to peritoneal spread and ascites. Therefore, 49 patients (61.2%) overall had endometrial pathology. Among 49 patients with endometrial pathology, 41 (83.7%) presented with abnormal bleeding.
The levels of serum tumor markers were studied in 44 patients and all were within normal levels except for CA-125 which was elevated in 15 of these 44 patients. The mean CA-125 level was 32.3 IU/ml (range, 7.2 to 178 IU/ml) in the whole group, and 56.0 IU/ml (range, 37.0 to 178.0 IU/ml) in patients with elevated CA-125 levels (Table 1).
All patients were subjected to surgical staging procedures including primary staging surgery, fertility saving staging surgery or restaging surgery (Table 2). Among them, 61 (76.2%) underwent primary staging surgery including total abdominal hysterectomy + bilateral salpingo-oophorectomy + bilateral pelvic-paraaortic lymph node dissection + infracolic omentectomy with or without tumoral debulking. Eight patients (10%) underwent fertility saving staging surgery including unilateral salpingo-oophorectomy + bilateral pelvic-paraaortic lymph node dissection + infracolic omentectomy with biopsies if indicated. In the remaining 11 patients (13.8%), a restaging procedure was performed within 4 weeks after cystectomy, oophorectomy, unilateral or bilateral salpingo-oophorectomy. Fifty-six of these patients (70.0%) were diagnosed to be stage I whereas the remaining 24 patients (30.0%) were stages III/IV. Although more patients who presented with abnormal bleeding were diagnosed at stage I initially, this did not reach statistical significance (79.1% vs. 59.5%, p=0.056). CA-125 levels were similar in patients with early and advanced stage disease (30.8 IU/ml vs. 36.1 IU/ml, p=0.57).
The mean diameter of the ovarian mass was 11.8 cm (range, 2 to 25 cm). In 3.8% of the patients, bilateral ovarian tumor was detected. Ascites was seen in 23 (28.8%) patients and it was more prevalent in patients with spread of disease beyond the ovary (16.1% vs. 58.3%, p<0.001) (Table 2).
Retroperitoneal nodal, peritoneal and hepatic involvement was detected in 8.8%, 16.2% and 2.5% of patients, respectively. In 5 patients, intracranial (frontal), hepatic, supraclavicular nodal plus hepatic, pulmonary, or urinary bladder metastasis resulted in stage IV disease. A patient with frontal lobe metastasis underwent craniotomy, and a mass sized 6×4 cm was completely removed. Also, the patient with metastasis to the urinary bladder was subjected to partial cystectomy to achieve complete debulking. On the other hand, macroscopic residual tumor was left in 6 patients (7.5%) with stage III or IV disease. Two patients with hepatic metastasis, 1 with pulmonary metastasis, and 3 with diffuse intraperitoneal spread had gross residual tumor after initial staging or restaging surgery.
A group consisting of 46.2% of patients did not receive adjuvant treatment while 42.5% of all patients received adjuvant chemotherapy, 3.8% received adjuvant radiotherapy, and 7.5% received both adjuvant chemotherapy and radiotherapy. While all patients with advanced stage disease received adjuvant therapy, only 33.9% of patients with stage I disease received adjuvant therapy due to capsular involvement, tumor rupture or poorly-differentiated tumor.
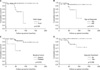
The follow-up began with the primary staging or restaging surgery and mean follow-up was 67.5 months (range, 2.0 to 162.0 months). The 5-year and 10-year overall survival was 91% and 86%, respectively. Mean survival was 147.1 months (95% CI, 136.5 to 157.7 months). In univariate analysis; advanced stage disease, advanced age at diagnosis, presence of macroscopic residual disease after surgery, and need for adjuvant treatment following surgery were associated with disease-related mortality (Table 3, Fig. 1). However, in multivariate analysis, only initial stage of disease was found to effect survival significantly.
During the follow-up period, recurrence was observed in 9 patients (11.2%) in a mean period of 45.9 months (range, 28.0 to 62.0 months). The recurrence rates were 5.4% in stage I, 21.1% in stage III, and 40.0% in stage IV. Compared with more advanced stages, recurrence was significantly lower in patients with stage I disease (5.4% vs. 25.0%, p=0.019) and in patients who were subjected to initial staging surgery (7.2% vs. 36.4%, p=0.018). The presence of gross residual disease did not affect the recurrence rates significantly. Only 2 of 9 patients (22.2%) with recurrence had gross residual disease after initial surgery. In these cases, the recurrence was detected by either examination or imaging after the patient had been disease-free during clinical or radiological evaluation performed after the completion of adjuvant treatment. Initial stages, adjuvant treatments, recurrence times, recurrence sites, and treatment after recurrences are shown in Table 4.
Granulosa cell tumors (GCT) of the ovary are considered as low grade malignancies with a relatively more favorable prognosis compared with much more commonly encountered epithelial ovarian tumors. However, patients diagnosed with GCT still suffer from recurrence or disease-related mortality necessitating surgery and/or other treatment modalities. Therefore, the prognostic factors in these relatively rare tumors need to be clarified.
In most studies, disease stage, patient's age and presence or absence of residual disease after initial surgery were shown to be important prognostic factors in GCTs.1,4 On the other hand, due to the rarity of the disease, studies on GCTs to date generally tend to consist of too few patients to detect prognostic factors clearly.
In this study, stage of disease, age of patient, presence of initial staging surgery of fertility saving surgery, presence or absence of macroscopic residual disease, and use of adjuvant treatment modalities were investigated in order to reveal their prognostic significance.
Stage is universally accepted as an important prognostic variable. Although 5-year and 10-year survival rates were reported to be 94% and 88%, respectively, these rates declined to only 44% in more advanced stages.1 Disease-related mortality rate of at least 40% was observed in patients with extra-ovarian disease spread.7 The importance of stage was also confirmed in the current study. Mean survival was significantly longer in patients with stage I disease, and mortality was significantly higher in patients with advanced stage disease. In fact, initial stage of disease was found to be the only factor associated with mortality in multivariate analysis.
Recurrence rates are also closely related with stage.8 In stage I disease, only 5% of patients recurred whereas this rate was 33% in more advanced stages.9 In our study group, recurrence rates were also significantly lower in stage I disease (5.4% vs. 25.0%, p=0.019).
Patient's age has been mentioned as a prognostic factor in some studies, but the favorable age category was highly variable.5 In this study, patients who were aged below 60 at the time of diagnosis had longer mean survival times (154.6 vs. 89.2 months, p=0.015), and experienced less mortality (4.9% vs. 21.1%, p=0.05). However, age was not found to be significant prognostic factor in multivariate analysis in terms of disease-related mortality. The recurrence rates were also similar in both age groups.
Residual disease after surgery may also affect oncologic prognosis adversely, and patients with residual tumor after surgery are recommended to receive adjuvant therapy.1,10 In the current series, the presence of macroscopic residual tumor after initial surgery resulted in a shorter survival time (55.8 vs. 157.5 months, p<0.001). Although rates of recurrence and mortality were higher in patients with residual disease, these did not reach statistical significance. In addition, all patients with macroscopic residual disease had advanced stage disease, as mentioned in another study.9 Possibly due to this fact, the presence of residual disease was not an independent prognostic factor.
Surgery is advocated as the first treatment of choice, because it provides the accurate information about the initial extent of disease, and therefore it documents the patients requiring adjuvant treatment modalities. Although the extent of the initial surgical procedure is still controversial and not standard, some authors reported higher relapse rates in cases of conservative surgery and better survival in cases with radical surgery.11 In patients of childbearing age with desire for future fertility, fertility saving surgery seems to be acceptable. However, a comprehensive staging procedure should again be performed since the pattern of spread seems to include peritoneal surfaces similar to epithelial ovarian carcinoma.12 In the current study, all 80 cases received a comprehensive surgical staging procedure. However, 11 patients had incomplete initial surgery and were subjected to a comprehensive restaging procedure within 4 weeks. Patients with initial staging surgery survived significantly longer (151.9 vs. 67.0 months, p=0.003), but both groups suffered similarly from mortality. Eight patients with a desire for fertility underwent fertility saving staging surgery with endometrial evaluation, which did not affect prognosis adversely. After fertility saving surgery, all patients were free of recurrent disease after a mean follow-up period of 81.7 months. Of these women, 5 attempted to get pregnant and 2 (40%) conceived successfully resulting in 3 healthy, term infants. One of these patients experienced a spontaneous pregnancy and another patient experienced two spontaneous pregnancies after two unsuccessful in vitro fertilization attempts. Although both of these patients received adjuvant combination chemotherapy after surgery, all three pregnancies resulted in healthy infants without any congenital malformations.
Due to the low incidence of these tumors, randomized studies assessing the value of postoperative adjuvant therapy in high-risk patients could not be possible up to date. Therefore, it is still not clear whether the use of postoperative treatment actually confers a survival advantage.5,6 Nevertheless, adjuvant treatment is considered in patients with metastatic or advanced diseases. The overall response rate to different combination chemotherapy regimens in advanced or recurrent granulosa cell tumors was reported to range from 50% to 92%.8 The overall response rate to the BEP (bleomycin, etoposide, cisplatin) combination which is considered to be an effective regimen with tolerable toxicity as a first-line chemotherapy was reported as 83% in metastatic sex-cord stromal tumors of the ovary.3,13 In this series, 53.8% of patients received adjuvant therapy due to advanced stage disease or high risk stage I disease. The adjuvant treatment modalities mainly included chemotherapy with or without radiotherapy. But use of adjuvant treatment modalities was not advantageous for recurrent disease or mortality. In fact, all mortalities were observed in cases who were given adjuvant treatment, the rate of mortality was 16.3% in this group. The adverse outcome in this group of patients should be attributed to the advanced stage of disease since use of adjuvant treatment was not found to be an important prognostic factor in multivariate analysis. Furthermore, the type of adjuvant treatment modalities, especially the types of chemotherapeutic agents given to the patients could not be included in the survival analysis as a prognostic factor because different chemotherapy regimens including melphelan, vincristine plus doxorubicin, vincristine plus doxorubicin plus cyclophosphamide, cisplatin plus vinblastine plus bleomycin, and bleomycin plus etoposide plus cisplatin were used from past to present.
This current study has weaknesses as well as strengths when compared with the existing literature. The most important weakness in our study is its retrospective nature. Nevertheless, given the rarity of GCTs of the ovary, it would not be possible to carry out prospective, well-controlled studies. Another weakness in this study is that it included patients treated for a relatively long period of 25 years. There are some factors which have changed with time and may possibly affect the outcome of the patients. These factors include the experience of the primary surgeons and the new regimens of combination chemotherapy evolved in time. But, once again, the rarity of this disease necessitates longer periods of time for the accumulation of cases. On the other hand, one of the strongest aspects of this study includes the availability of a standard initial management consisting of a comprehensive surgical staging or restaging, which was performed in a single institute with experienced gynecologic oncologists. Also, the study group which includes 80 women with ovarian GCT represents one of the largest scale studies published in the English literature so far.6
In conclusion, the single most important prognostic factor in ovarian GCT seems to be the initial stage of disease. Therefore, a comprehensive staging surgery should be attempted whenever possible to document the real extent of disease and to estimate the oncologic outcome more accurately. In cases without initial staging surgery, a restaging surgery should be performed by a gynecologic oncologist to establish the stage and to be able to estimate the prognosis more accurately unless the patient is medically unfit. In patients with desire for fertility, a fertility saving staging surgery with endometrial biopsy is safe, and chemotherapy may be used if indicated without adversely affecting the chance and outcome of future pregnancies. Also, given the rarity of GCTs of the ovary, prospective, randomized, controlled, multi-center studies with higher number of patients who are subjected to standard treatment modalities are needed to clarify other possible prognostic factors.
Figures and Tables
Fig. 1
Survival curves according to initial stage of disease (A), age at diagnosis (B), presence or absence of macroscopic residual tumor (C), and adjuvant treatment status (D).
References
1. Malmstrom H, Hogberg T, Risberg B, Simonsen E. Granulosa cell tumors of the ovary: prognostic factors and outcome. Gynecol Oncol. 1994. 52:50–55.
2. Segal R, DePetrillo AD, Thomas G. Clinical review of adult granulosa cell tumors of the ovary. Gynecol Oncol. 1995. 56:338–344.
3. Gershenson DM, Morris M, Burke TW, Levenback C, Matthews CM, Wharton JT. Treatment of poor-prognosis sex cord-stromal tumors of the ovary with the combination of bleomycin, etoposide, and cisplatin. Obstet Gynecol. 1996. 87:527–531.
4. Schwartz PE, Smith JP. Treatment of ovarian stromal tumors. Am J Obstet Gynecol. 1976. 125:402–411.
5. Schumer ST, Cannistra SA. Granulosa cell tumor of the ovary. J Clin Oncol. 2003. 21:1180–1189.
6. Cronje HS, Niemand I, Bam RH, Woodruff JD. Review of the granulosa-theca cell tumors from the emil Novak ovarian tumor registry. Am J Obstet Gynecol. 1999. 180:323–327.
7. Uygun K, Aydiner A, Saip P, Kocak Z, Basaran M, Dincer M, et al. Clinical parameters and treatment results in recurrent granulosa cell tumor of the ovary. Gynecol Oncol. 2003. 88:400–403.
8. Uygun K, Aydiner A, Saip P, Basaran M, Tas F, Kocak Z, et al. Granulosa cell tumor of the ovary: retrospective analysis of 45 cases. Am J Clin Oncol. 2003. 26:517–521.
9. Sehouli J, Drescher FS, Mustea A, Elling D, Friedmann W, Kuhn W, et al. Granulosa cell tumor of the ovary: 10 years follow-up data of 65 patients. Anticancer Res. 2004. 24:1223–1229.
10. Evans AT 3rd, Gaffey TA, Malkasian GD Jr, Annegers JF. Clinicopathologic review of 118 granulosa and 82 theca cell tumors. Obstet Gynecol. 1980. 55:231–238.
11. Pautier P, Lhomme C, Culine S, Duvillard P, Michel G, Bidart JM, et al. Adult granulosa-cell tumor of the ovary: a retrospective study of 45 cases. Int J Gynecol Cancer. 1997. 7:58–65.
12. Auranen A, Sundstrom J, Ijas J, Grenman S. Prognostic factors of ovarian granulosa cell tumor: a study of 35 patients and review of the literature. Int J Gynecol Cancer. 2007. 17:1011–1018.
13. Homesley HD, Bundy BN, Hurteau JA, Roth LM. Bleomycin, etoposide, and cisplatin combination therapy of ovarian granulosa cell tumors and other stromal malignancies: a Gynecologic Oncology Group study. Gynecol Oncol. 1999. 72:131–137.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download