Abstract
Cervical cancer can be presented as an unusual and aggressive manner in human immunodeficiency virus (HIV)-positive women. There are case reports of psoas abscess which mimick metastasis from cervical carcinoma in HIV-positive patients. However, such cases are very rare in HIV-negative women with only few case reports available in the literature. We report one case of psoas abscess mimicking metastasis in a HIV-negative woman, which was initially diagnosed as spinal tuberculosis.
There are only very few case reports of psoas abscess like metastasis from carcinoma of the cervix in human immunodeficiency virus (HIV) negative patients. We report one such case which was initially diagnosed as spinal tuberculosis.
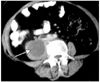
A 60-year-old multiparous female presented with complaints of low backache for the last 1 month. There was no history of fever or trauma. She had been diagnosed as a case of squamous cell carcinoma of the cervix, stage IIb and had completed radiotherapy two years previously. Clinical examination and pelvic ultrasound did not show any features of local recurrence. Laboratory investigations revealed a hemoglobin level of 10.9 g/dl, total leukocyte count of 10,200 cells/mm3 with 64% neutrophils, 30% lymphocytes, 6% eosinophils, 0% monocytes and 0% basophils. Erythrocyte sedimentation rate was 5 mm in the 1st hour. Serum creatinine and blood urea levels were within normal limits and serology for human immunodeficiency virus (HIV-1) was nonreactive. The CEA level was not elevated. Evaluation for SCC marker was not performed. The patient underwent computed tomography (CT) examination of the chest and abdomen which showed the presence of lytic lesions involving the L2 and L3 vertebrae with cortical destruction and an associated well-defined hypodense lesion in the right psoas muscle, measuring 3 × 2.8 × 3.2 cm, with peripheral enhancement (Fig. 1). No other abnormal findings were detected elsewhere in the chest and abdomen. Initially, a diagnosis of spinal tuberculosis with right psoas abscess was made due to the endemicity of tuberculosis in this part of the world. Magnetic resonance imaging (MRI) of the lumbosacral spine also revealed altered signal intensity of the L2 and L3 vertebrae with associated right psoas abscess (Fig. 2). The intervening disc space was normal. The bone scan revealed increased uptake in the involved lumbar vertebrae. However PET scanning was not performed in this case. Subsequently, ultrasound guided fine needle aspiration cytology (FNAC) of the right psoas lesion was performed to establish the diagnosis before treatment. The aspirate yielded thick pus, however cytological examination was not suggestive of tuberculosis, and the staining for acid fast bacilli (AFB) was negative. FNAC was again repeated under CT guidance of the right paravertebral region adjacent to the destroyed lumbar vertebrae, which revealed the presence of malignant squamous cells consistent with the diagnosis of metastatic squamous cell carcinoma (Fig. 3). The patient received radiotherapy for the metastatic lesion of the spine, after which significant symptomatic and radiologic improvement was noted.
Mynter first described the entity psoas abscess in 1881 and referred to it as psoitis.1 Psoas abscess may be classified as primary or secondary. Primary psoas abscess occurs probably as a result of hematogenous spread of an infectious process from an occult source in the body. The usual pathogens are Staphylococcus aureus, Streptococcus species and Escherichia coli.1 Secondary psoas abscesses result from extension of an infectious process from adjacent bone, genitourinary tract or intestines.2 Clinical presentation includes back pain with limitation of function, fever and leukocytosis. Ultrasonography, CT and MRI are the keys to definitive diagnosis.1
Invasive cervical carcinoma is well accepted as an AIDS-defining condition. Immunosuppression from the virus increases the incidence and severity of neoplasia. Hence cervical cancer can manifest itself in an unusual and aggressive manner in HIV-positive women. There are case reports of psoas abscess like metastasis from cervical carcinoma in HIV positive patients.3 However, metastases from carcinoma of the cervix presenting as a psoas abscess in HIV negative women is very rare with only a few case reports available in the literature to the best of our knowledge. The case reported by Devendra and Tay2 describes only muscle involvement without bone involvement, while the case reported by Bar-Dayan et al.4 noted associated bone involvement also. In these two case reports the primary tumor was diagnosed simultaneously. However in the case reported by George and Lai5 the primary cervical tumor had been treated previously by radiotherapy, as in our case, but the HIV status of the patient was not mentioned.
In this index case, since the patient presented with psoas abscess like lesion associated with lytic destruction of the lumbar vertebrae, the possibility of spinal tuberculosis was the initial diagnosis. But the aspirate from the right psoas did not show the presence of AFB. As we were aware of the fact that metastatic squamous cell carcinoma of cervix can present as a psoas abscess, we again repeated the FNAC from the destroyed bone under CT guidance, which finally established the diagnosis.
This case highlights the fact that metastasis from squamous cell carcinoma of the cervix can present as a psoas abscess. It has to be considered as a differential diagnosis in all cases of carcinoma of the cervix with paraspinal lesions before diagnosing them as spinal tuberculosis, even in regions endemic for tuberculosis.
Figures and Tables
Fig. 1
CT image. Well-defined hypo-dense lesion in the right psoas muscle (arrow) with peripheral enhancement (3×2.8×3.2 cm).
References
1. Bagul NB, Abeysekara AM, Jacob S. Primary psoas abscess due to Streptococcus milleri. Ann Clin Microbiol Antimicrob. 2008. 7:7.
2. Devendra K, Tay SK. Metastatic carcinoma of the cervix presenting as a psoas abscess in an HIV-negative woman. Singapore Med J. 2003. 44:302–303.
3. Singh GS, Aikins JK, Deger R, King S, Mikuta JJ. Metastatic cervical cancer and pelvic inflammatory disease in an AIDS patient. Gynecol Oncol. 1994. 54:372–376.
4. Bar-Dayan Y, Fishman A, Levi Z, Rachmani R. Squamous cell carcinoma of the cervix with psoas abscess-like metastasis in an HIV-negative patient. Isr J Med Sci. 1997. 33:674–676.
5. George J, Lai FM. Metastatic cervical carcinoma presenting as psoas abscess and osteoblastic and lytic bony metastases. Singapore Med J. 1995. 36:224–227.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download