Abstract
The preservation of fertility in female cancer survivors has become an important health issue. The different cryopreservation options available for fertility preservation are embryo, oocyte, and ovarian tissue cryopreservation. Oocyte cryopreservation is available for women without partners, but there is a limited experience with this technique and the pregnancy rate is still low. In spite of recent reports of successful birth after autotransplantation of cryopreserved-thawed human ovarian cortical tissues, clinical experience is also limited and this technique remains still experimental. Whole ovary cryopreservation itself poses several challenges. Further researches for establishing optimal cryopreservation and thawing protocols and increasing post-thawing survival, pregnancy, and delivery rates are necessary. In this article, the strategies for fertility preservation in cancer survivors are discussed. The different options and their results are discussed, as well as their indications, efficacy and ethical issues.
Cancer is not rare in younger women of reproductive age. Recent data estimate that more than 679,540 women in United States, many of reproductive age, are diagnosed with invasive cancer annually.1 The number of young women diagnosed with cancer has been increasing. According to the 2002 Annual report of the Korea Central Cancer Registry, 10,945 reproductive aged women (15-44 years old) were newly diagnosed with invasive cancer in 2002.2 Advances in the diagnosis and treatment of childhood, adolescent and adult cancer have greatly increased the life expectancy of premenopausal women who have overcome their disease. By the year 2010, as many as 1 in 250 patients will have survived malignancies.3 For the treatment of cancer, aggressive chemotherapy, especially with alkylating agents and ionizing radiotherapy, can destroy gonads and subsequently lead to a loss of fertility and premature ovarian failure.4 Even in those patients who were not sterilized by high dose chemotherapy or radiotherapy, there may be an increased risk for complications during pregnancy such as early pregnancy loss, premature labor, and low birth weight.5 It had been reported that a four-fold increased risk of premature ovarian failure (POF) in teenagers treated for cancer, and a risk increased by a factor of 27 in women between 21 and 25 years of age.6
The advent of in vitro fertilization (IVF) and its current worldwide use has resulted in the development of successful cryopreservation techniques for surplus embryos. These cryopreservation techniques have further been applied to the unfertilized mature human oocyte7 and ovarian tissue.8-10
In this brief review, we address which reproductive technologies, especially cryopreservation, are presently available for the preservation of fertility in the reproductive age women who will be treated with an anti-cancer chemoradiotherapy, and some of the challenges encountered with their clinical application.
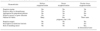
Several options are currently available to preserve fertility in cancer patients and give them the opportunity to conceive when they have overcome their disease: embryo cryopreservation, oocyte cryopreservation or ovarian tissue cryopreservation (Table 1).11-15 The choice of the most suitable method for preserving fertility depends on different parameters: the type and timing of chemotherapy, the type of cancer, the patient's age and the partner status.
If the patient has a partner or accepts donor sperm, embryo cryopreservation should be considered first, since this is a clinically well-established procedure. Embryo cryopreservation is the preferred method to preserve fertility due to reasonable delivery rates, according to the Ethics Committee of the American Society for Reproductive Medicine.16 This method requires the patient to be of pubertal age, have a partner or use donor sperm, and be able to undergo a cycle of ovarian stimulation. However, many women who are faced with a decision regarding their future fertility may not have an established partner or may not desire to use donor sperm.17 In addition, it is not possible when the chemotherapy has to be initiated immediately or when ovarian stimulation is contraindicated due to the type of cancer.
Cryopreservation of oocytes can be used in single women who can undergo a stimulation cycle, although the effectiveness of this technique is very low, with pregnancy and delivery rates ranging from 1 to 5% per frozen oocyte.18-20
Ovarian tissue cryopreservation is the ideal option for prepubertal girls, and for women who cannot delay the start of chemotherapy. Ovarian tissue can be frozen using different categories: cortical fragments, whole ovary with its vascular pedicle or isolated follicles. In humans, ovarian tissue cryopreservation and transplantation procedures have so far been almost limited to avascular cortical fragments, both in experimental and in clinical studies. Until now, ovarian cortical tissue cryopreservation is the only procedure that has resulted in live births in humans after autologous transplantation.14,21,22
Embryo cryopreservation is an established clinical procedure, and currently is the only widely available option for fertility preservation. Reported survival rates per thawed embryo range between 35 and 90%, implantation rates between 8 and 30%, and cumulative pregnancy rates can be more than 60%.23 However, there are several limitations in this approach. First, the patient needs a male partner or to use donor sperm. Second, ovarian stimulation precedes oocyte retrieval for IVF, necessitating a delay in the initiation of chemotherapy or radiotherapy that may not be acceptable in many cases. Third, exposure to the high serum estrogen concentrations during ovarian stimulation may be contraindicated in women with estrogen-sensitive malignancies such as breast cancer.24 Natural cycle IVF could avoid this high estrogen milieu, but the oocyte yield is too small to use considering the limited time for IVF treatment. Tamoxifen has been used with some success as an alternative to provide safer ovarian hyperstimulation for breast cancer patients.25 However, as tamoxifen has a stimulatory effect on the endometrium, it cannot be used for ovarian stimulation in endometrial cancer patients. Instead, the use of aromatase inhibitors has been proposed for patients with endometrial cancer. Letrozole, a potent third generation aromatase inhibitor, competitively inhibits the activity of aromatase and has a half life of approximately 48 hours.26 Recent studies showed successful ovarian stimulation with letrozole and gonadotropins with reduced estrogen exposure, compared with standard stimulation cycles in breast and endometrial cancer patients.27,28
Embryo cryopreservation may not be an option for single women unless they choose to use sperm donation. In these patients, if they have time to complete ovarian stimulation prior to cancer therapy, cryopreservation of mature or immature oocytes can be considered as another option. However, oocyte cryopreservation also delays cancer therapy because it requires ovarian stimulation before obtaining oocytes. In addition, early results have been disappointing with respect to low survival, fertilization, and pregnancy rates after IVF of thawed oocytes, due to the fragility of the meiotic spindle and the formation of ice crystals.23 Thus, it still requires further investigation for this to become a routine clinical procedure.
Since the first human live birth from cryopreserved oocytes was reported in 1986,29 more than 300 babies have been born with cryopreserved-thawed oocytes. The mature oocyte is extremely fragile during freezing-thawing due to its large size, high water content, and chromosomal arrangement. At metaphase, chromosomes are arranged in a linear fashion at the equatorial plane on meiotic spindles. Intracellular ice formation associated with the freeze-thaw process has been found to be detrimental to the spindle apparatus.30 These characteristics of mature oocyte are the reason for low survival rates after cryopreservation. Sonmezer and Oktay reviewed data from 21 studies in peer-reviewed journals and found a mean survival rate of 47%, a mean fertilization rate of 52.5%, and a mean pregnancy rate per thawed oocytes of 1.52%.23 However, recent advances in freezing and thawing technology resulted in a higher survival rate of frozen-thawed oocytes, as well as improved pregnancy rates.31 One of the factors that improved fertilization rates of cryopreserved-thawed oocytes is the use of intracytoplasmic sperm injection (ICSI) to overcome the zona hardening caused by the cryopreservation process.32 It also has been showed that ICSI results in embryos with greater cleavage rates.33
Based on different rates of freezing and thawing and cryoprotectants used, several protocols for oocyte cryopreservation have been described. The most commonly employed is the slow freeze-rapid thaw protocol. Also, newly developed techniques in oocyte cryopreservation by a slow-freezing protocol include modification of cryoprotectant solution and cryopreservation techniques, and the use of sodium-depleted media.34-37
An alternative technique aimed at preventing ice formation and improved oocyte survival is vitrification. Vitrification is the process of cryopreservation using high concentrations of cryoprotectant with a high cooling rate to solidify the cell into a glass-like state without causing ice formation.38 Vitrification is easier and less expensive and does not require a programmable freezer that is mandatory for the conventional slow freezing method.39 Recently, improved post-thaw survival and fertilization rates and live births have been reported.40 Based on a review of published reports using vitrification, mean survival rate of 68.4%, fertilization rate of 48.5% and pregnancy rate of 1.7% per vitrified-thawed oocyte were reported.23
Immature oocytes cryopreserved at the germinal vesicle (GV) stage survive better than those frozen at the metaphase II stage.41 They are more resistant to damage from cryopreservation because of lower cell volume and lack of a metaphase spindle. However, although GV oocytes have a higher post-thaw survival rate and a lower incidence of spindle damage, the inefficiency of established in vitro maturation protocols results in a final yield of mature oocytes that is similar to that obtained with cryopreserved mature oocytes.42 Recently, similar rates of maturation, fertilization, and embryo development have been achieved by vitrification of immature human oocytes, compared with control oocytes.43 However, only a few pregnancies have been reported using frozen-thawed human immature oocytes and the experience in human GV oocyte freezing is very limited.44,45 The Practice Committee of the American Society for Reproductive Medicine recommended that oocyte cryopreservation should be presently considered as an experimental technique, only to be performed under an institutional review board-approved investigational protocol.46
In 1994, Gosden et al. reported the successful restoration of fertility by autografting frozen-thawed ovarian tissue in sheep.47 Due to the recent development of more effective cryoprotectants such as ethylene glycol, dimethyl sulfoxide (DMSO), and propanediol, animal studies were repeated and successful deliveries were reported in a number of species.47,48 In ovarian tissue cryopreservation, hundreds of primordial follicles containing immature oocytes, unlike with embryo or oocyte cryopreservation, can be cryopreserved in situ. There are several advantages, such as abundant germ cells, no need for ovarian stimulation and consequent delay in initiating cancer treatment. Moreover, primordial follicles are significantly less susceptible to thermal injury than both mature and immature oocytes, because of their small size, slower metabolic rates, and the absence of a zona pellucida.24 Similar to oocyte cryopreservation, a male partner is not required. Thus, this procedure is an option for single patients and prepubertal girls. In children, ovarian tissue cryopreservation is the only fertility-sparing method because ovarian stimulation and oocyte collection cannot be considered ethical.
Three strategies, such as fragments of cortical tissue, isolated cryopreserved primordial follicles, and the transplantation of cryopreserved whole ovary, will be discussed.
Since it has been demonstrated that normal menstrual function could be restored and spontaneous pregnancies achieved after autologous orthotopic transplantation of cryopreserved ovarian cortex tissue using oophorectomized sheep,47 ovarian tissue has been successfully cryopreserved and transplanted into many species such as rodents, sheep, and marmoset monkeys.49-51 In a primate, Lee et al. reported that in the successful fertilization and pregnancy after oocyte collection from fresh transplanted ovarian tissue, the graft tissue functioned without any surgical connection to major blood vessels.52 The outer cortical layer of the ovary contains most of the primordial follicles. The ovary is removed by laparoscopy or laparotomy, and cut into strips of tissue around 1-3 mm in thickness and up to 1 cm2 in total area to allow for adequate penetration of the cryoprotectant solution.53 In cancer patients, a pathologic assessment of the ovarian tissue must be performed to exclude the presence of metastatic disease. In in vitro studies, viability can be obtained in over 70-80% of the specimens using the slow freezing and rapid thawing method.
There are, theoretically, three approaches in the development of immature follicles: autotransplantation (orthotopically or heterotopically), xenotransplantation, and in vitro culture.54
Reported cases of autotransplantation of cryopreserved ovarian tissue, either orthotopically within the pelvis of heterotopically within subcutaneous tissue, are summarized in Table 2. There are some different characteristics between orthotopic and heterotopic autotransplantation (Table 3). Orthotopic autotransplantation of cryopreserved ovarian tissue may result in a natural pregnancy if the fallopian tubes remain patent. However, this procedure requires abdominal surgery and general anesthesia. A laparoscopic surgery makes this procedure less invasive but technically more difficult. Several cases have been reported, showing spontaneous follicular maturation23,55 and presumably ovulation following stimulation with menopausal gonadotrophins.23
The first case of a successful spontaneous pregnancy from cryopreserved ovarian cortical tissue has been contended for not providing definite evidence of a pregnancy from cryopreserved and transplanted ovarian cortical tissue, because the subject patient had not undergone a bilateral oophorectomy.21 The major disadvantage of transplanting ovarian cortical strips is that revascularization of the graft needs the several days. Also, the consequent ischemia is the technical limitation of cortical tissue transplantation, whether orthotopic or heterotopic. There is a possibility of follicle atresia during the period of ischemia, before the tissue becomes revascularized. Because of that event, ovarian function might be compromise beyond several months of follow-up (mean duration; 9 months).23,55
Heterotopic autotransplantation of cryopreserved ovarian tissue has several advantages. This procedure is minimally invasive, reversible, repeatable, and it permits easy access to the graft for monitoring the follicular development or in the event of reoperation.56 Usually, heterotopic transplantation can be conducted at sites such as the forearm or abdominal subcutaneous tissue.57,58 It has been claimed that oocyte quality might be compromised by transplantation to a heterotopic site, due to differences in temperature and pressure which may interfere with follicular development in these sites.59 The comparison of the methods of autotransplantation is summarized in Table 3.
In vitro maturation and ovarian tissue xenotransplantation may someday become common applications in conjunction with ovarian cryopreservation. Xenotransplantation of human ovarian tissue was reported in 1998.60 It was revealed that human ovarian tissue xenografted into the severe combined immunodeficiency disease (SCID) mouse demonstrated estradiol production and estrogenization of tissues after follicle-stimulating hormone administration. However, possible transmission of prions and animal viruses accompanying the retrieved oocyte must be considered. Nowadays, this technique is suggested as a means of evaluating follicular reserve and function in cryopreserved human ovarian tissue.61,62 In in vitro maturation of oocytes, epigenetic abnormalities secondary to methylation defects may be of significant concern.63
Because the oocyte of the primordial follicle contains a relatively inactive metabolic status, as well as a lack of the meiotic spindle, zona pellucida and cortical granules, the primordial follicle is resistant to cryoinjury. Moreover, the small size of follicles facilitates penetration of the cryoprotectant. Despite these advantages, the technique of isolation primordial follicles remains difficult,64 and it has not been possible to culture isolated human primordial follicles to the mature oocyte stage in vitro.65 This method may exclude the possibility of reintroducing tumor cells into cancer patients by autografting of ovarian tissue.
Encouraging the clinical application of this method, further studies are clearly needed to identify factors sustaining follicular growth and maturation in in vitro culture systems.66 Follicle isolation, or partial follicle isolation, severely impairs follicular viability in cultures. After isolation procedure, primordial and primary follicles degenerate within the first 24 hours of culture.67 Therefore the isolation procedure of primordial follicles, using enzymatic digestion, should be optimized to enhance the retrieval rate and viability of the oocyte.
It has been suggested that transplanting a suspension of isolated follicles may be another option, as the follicular basal lamina encapsulating the membrana granulosa excludes capillaries, white blood cells and nerve processes from the granulosa compartment, and grafting fully isolated follicles may be safer.68 In addition, establishing faster angiogenesis and minimizing ischemic and reperfusion damage would permit the introduction of a high number of follicles into the host.
The survival of transplanted ovarian tissue is completely dependent on the establishment of neovascularization. If this process is incomplete, a large proportion of follicles are lost as a result during the initial ischemia period just after transplantation.69,70 It is necessary to maintain the follicular reserve and extend the life span and function of the ovarian tissue so that the ischemic period between transplantation and neovascularization be reduced. One of the future approaches to preserve fertility is the transplantation of an intact ovary with vascular anastomosis, allowing immediate revascularization of the ovary.
Transplantation of fresh whole ovary with vascular anastomosis has already been successfully performed in rats,71 rabbits,72 sheep,73 dogs,74 monkeys75 and humans.76 The first case of restoration of fertility after whole frozen ovary transplantation was reported by Wang et al. in 2002.71 They described that the survival rate was 57% (4/7 rats), which survived for ≥60 days, and the pregnancy rate was 25% (1/4 rats). Despite this success in rats, it remains as a technical problem to cryopreserve whole ovaries from large mammals and humans, which are larger and more fibrotic. There is a difficulty of adequate diffusion of cryoprotectants into large tissues, and vascular injury caused by intravascular ice formation. The duration of subsequent ovarian function is initially limited, mostly due to ischemia resulting from thrombosis.77 To overcome this problem, it has been suggested that the graft be perfused with heparinized Ringer's solution, followed by perfusion and immersion in a bath containing cryoprotectants immediately after oophorectomy. The ovarian vessels and excess hilar tissue is dissected, and grafts are perfused via the ovarian artery with the cryoprotectants using infusion system to maintain a flow rate at 1.3 mL/min with continuous replenishment of the reservoir.78 Recently, such attempts have been also applied in human whole ovary and a comparable survival rate (75.1%) is obtained.79,80
It should be considered in whole ovarian cryopreservation used for younger women, whose ovaries have a mean size of 3×2×2 cm, that this protocol will need a larger cryovial than conventionally used. Also, the programmed freezer system should have a larger cryochamber. Surgical technique should be trained; great care must be taken to remove the ovary, together with a larger part (≥5 cm) of the infundibulopelvic ligament, allowing dissection of the ovarian vessels, and perfusion with a cryoprotective medium. Until now, the status of whole ovary cryopreservation remains experimental. Research and development of technology to cryopreserve whole organs, as well as surgical techniques for the autotransplantation of an entire ovary with its vascular pedicle, should be encouraged.
Shaw et al. reported the transmission of lymphoma via grafts of ovarian tissue from diseased donor mice to healthy recipients.81 This study emphasized the risks of clinical application by transplantation of ovarian tissue to women recovering from cancer, especially a blood-borne cancer.81,82 However, clinical ovarian metastasis is rare in "common" cancers of young patients, such as Wilms' tumor and Hodgkin's disease. The risk of transferring cancer cells depends on the disease type, activity, stage, and mass of malignant cells transferred. Screening methods should be developed to eliminate the risk of cancer cell transmission with reimplantation. Recently, it has been suggested that preoperative imaging prevents operation and storage of tissue with cancer, and evaluation of stored ovarian tissue for minimal residual disease (MRD) using sensitive markers (e.g. Anti-CD 30, and anti-Ki 67) is essential to increase safety and to prevent reimplantation of tissue with malignant cells.83 In fact, it may be feasible to screen the harboring metastatic cancer cells in the preserved ovarian tissue before transplantation using immunohistochemistry, flow cytometry, or molecular genetic techniques such as reverse transcriptase-polymerase chain reaction and fluorescence in situ hybridization.
The lifespan of transplant ovarian tissue is dependent on the degree of ischemia. Ischemic injury after transplantation can be minimized by relief of hypoxic tissue damage by using antioxidants and facilitation angiogenesis by angiogenic factors. Ultimately, to prevent ischemic tissue injury, the strategy is whole ovary transplantation with vascular anastomosis. These studies have been conducted to establish the optimal techniques of whole ovaries.
The point that needs consideration is that the malignant transformation of transplanted ovarian tissue may occur. The major indications for ovarian tissue harvest are for cancer, and they also have the same risk of cancer in ovarian tissues as well as other tissues. In particular, patients with BRCA-1 and BRCA-2 mutations have a 60% and 10-20% lifetime risk of developing ovarian cancer, respectively.84 These patients often undergo prophylactic oophorectomy to decrease their chance of ovarian / peritoneal cancer by 90%, or as part of a treatment plan for breast cancer.85 Heterotopic transplantation can be considered in these patients, but the transplanted ovarian tissue should be removed in its entirety as soon as treatment for fertility is complete.
In vitro maturation and xenotransplantation may become an alternative plan in the future. However, recent studies have investigated the integrity of human oocytes obtained after subcutaneous xenografting of cryopreserved ovarian tissue into SCID mice and in vitro maturation of retrieved cumulus-oocyte complexes.86 Unfortunately, some oocytes showed abnormal nuclear and cytoplasmic maturation by immunocytochemical analysis of microtubules and DNA.
A completely unknown variable requiring long-term follow-up is the questionable relative risk of epithelial or germ cell malignant transformation in transplanted ovarian tissue secondary to the rapid temperature changes and exposure to cryoprotectants inherent in the cryopreservation process.
This technique has additional risks. The epigenetic abnormalities secondary to methylation defects may be of significant concern.63 Xenotransplantation may have a risk of transmission of prions and animal viruses accompanying the retrieved oocyte. in vitro maturation and ovarian xenotransplantation may one day become common applications in conjunction with ovarian cryopreservation, and the practitioner should be able to explain the risk of this techniques.
Young cancer patients are psychologically vulnerable, when they recognize the disease as well as a possibility of infertility after cancer therapy. In this situation, it is important that the physician reassure the patients suggesting several options to preserve their fertility. Moreover, clinical experience is also limited and this technique remains still experimental. Clinical application of these unproven experimental procedures can be ethically complex. The ethical issues of fertility preservation should be discussed.
The primary ethical consideration is the safety of the procedures. The procedure of fertility preservation should not harm the patient by dangerously delaying cancer treatment. For example, oocyte cryopreservation requires ovarian stimulation and oocyte retrieval, which can delay chemotherapy and increase the chance of cancer growth and metastasis. Ovarian stimulation with gonadotropin may increase the E2 levels, which might stimulate estrogen-sensitive tumors (e.g. breast cancer). It is not ethical to suggest oocyte cryopreservation to preserve fertility, because of the risk is clear and the benefit is uncertain. One of the most important ethical issues is to ensure that no remnant cells are reintroduced by subsequent transplantation.
Until now, most strategies to preserve the fertility in women are still experimental and do not guarantee the recovery of fertility. Oocyte and ovarian tissue cryopreservation before cancer therapy appear to be hopeful options for fertility preservation. However, oocyte cryopreservation is not a well-established method and the pregnancy rates are still low. The principles of beneficence and non-maleficence are paramount in the treatment of minors, especially when they are psychologically vulnerable. It should not be offered if delaying anti-cancer therapy would increase the risk of disease aggravation.
Ovarian tissue cryopreservation is also ethically challenging. This method is potentially useful, but it is too early to determine the true benefits since there are only three case reports of live birth after transplantation of cryopreserved human ovarian tissue. Therefore, it is an ethical dilemma whether we should even offer a new, unproven technology with potential benefits but with known risks. Ovarian tissue cryopreservation may increase the risks because it requires surgery under the general anesthesia to harvest ovarian tissue. There would be added risks such as bleeding, infection, and bowel injury. It may not be justified to collect ovarian tissue from infants or very young children whose ovaries are small and for whom surgery is a high risk procedure. It also may not be ethical to offer this procedure to the patients whose ovaries are already exhausted of oocytes because of age or cancer therapy.
In children suffering from cancer, patients' rights may be a concern. In the current context, her 'best interest' includes both her present interest in minimizing risk and her future interest in fertility preservation. This consent should be a reflection of the parents' respect for their child. Children should be allowed to assent to their treatment after being provided with a full explanation including risks, discomforts, benefits, and alternatives. If the medical risk is acceptable, it seems that parents have an ethical right to request fertility preservation.
Knowing that there are options for fertility preservation can be a relief for them, but they should be well informed to prevent false expectations as well as the possibility of being exploited by the commercial interests of the purveyors of unproven technologies.
In general, young female cancer patients are poorly counseled on their options for fertility preservation. Treatment of the cancer is of utmost importance, but several assisted reproductive technologies can provide relief from the uncertainty of future without compromising cancer treatments. The number of options is growing continuously, some are more established, such as embryo cryopreservation, and some are still experimental, such as ovarian tissue cryopreservation.
The different cryopreservation options available for fertility preservation in female cancer patients are embryo, oocyte, and ovarian tissue cryopreservation. Because of the variations in the type of cancer, type and dose of chemotherapy, the time available before onset of treatment, the patient's age, and the status of partners, each case should be individualized and requires a different strategy in fertility preservation (Fig. 1).
Under the ethical principle, appropriate expansion of the indication and further studies on optimizing technique must continue in anticipation that cryopreservation of the oocyte and ovarian tissue will become a useful and widely accepted option in preserving female fertility in young cancer patients.
Figures and Tables
References
1. Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, et al. Cancer statistics, 2006. CA Cancer J Clin. 2006. 56:106–130.
2. Korea Central Cancer Registry, Ministry of Health and Welfare Republic of Korea. 2002 Annual report of the Korea Central Cancer Registry. 2003. Seoul: Ministry of Health and Welfare.
3. Bleyer WA. The impact of childhood cancer on the United States and the world. CA Cancer J Clin. 1990. 40:355–367.
4. Apperley JF, Reddy N. Mechanism and management of treatment-related gonadal failure in recipients of high dose chemoradiotherapy. Blood Rev. 1995. 9:93–116.
5. Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Munson ML. Births: Final data for 2002. Natl Vital Stat Rep. 2003. 52:1–113.
6. Larsen EC, Muller J, Schmiegelow K, Rechnitzer C, Andersen AN. Reduced ovarian function in long-term survivors of radiation-and chemotherapy-treated childhood cancer. J Clin Endocrinol Metab. 2003. 88:5307–5314.
7. Porcu E, Fabbri R, Seracchioli R, Ciotti PM, Magrini O, Flamigni C. Birth of a healthy female after intracytoplasmic sperm injection of cryopreserved human oocytes. Fertil Steril. 1997. 68:724–726.
8. Bahadur G, Steele SJ. Ovarian tissue cryopreservation for patients. Hum Reprod. 1996. 11:2215–2216.
9. Oktay K, Buyuk E, Veeck L, Zaninovic N, Xu K, Takeuchi T, et al. Embryo development after heterotopic transplantation of cryopreserved ovarian tissue. Lancet. 2004. 363:837–840.
10. Poirot C, Vacher-Lavenu MC, Helardot P, Guibert J, Brugieres L, Jouannet P. Human ovarian tissue cryopreservation: Indications and feasibility. Hum Reprod. 2002. 17:1447–1452.
11. Gosden RG, Rutherford AJ, Norfolk DR. Transmission of malignant cells in ovarian grafts. Hum Reprod. 1997. 12:403.
12. Donnez J, Bassil S. Indications for cryopreservation of ovarian tissue. Hum Reprod Update. 1998. 4:248–259.
13. Oktay K, Karlikaya G. Ovarian function after transplantation of frozen, banked autologous ovarian tissue. N Engl J Med. 2000. 342:1919.
14. Meirow D, Levron J, Eldar-Geva T, Hardan I, Fridman E, Zalel Y, et al. Pregnancy after transplantation of cryopreserved ovarian tissue in a patient with ovarian failure after chemotherapy. N Engl J Med. 2005. 353:318–321.
15. Kim SS. Fertility preservation in female cancer patients: Current developments and future directions. Fertil Steril. 2006. 85:1–11.
16. Ethics Committee of the American Society for Reproductive Medicine. Fertility preservation and reproduction in cancer patients. Fertil Steril. 2005. 83:1622–1628.
17. Practice Committee of the American Society for Reproductive Medicine. Ovarian tissue and oocyte cryopreservation. Fertil Steril. 2004. 82:993–998.
18. Stachecki JJ, Cohen J. An overview of oocyte cryopreservation. Reprod Biomed Online. 2004. 9:152–163.
19. Borini A, Sciajno R, Bianchi V, Sereni E, Flamigni C, Coticchio G. Clinical outcome of oocyte cryopreservation after slow cooling with a protocol utilizing a high sucrose concentration. Hum Reprod. 2006. 21:512–517.
20. Levi Setti PE, Albani E, Novara PV, Cesana A, Morreale G. Cryopreservation of supernumerary oocytes in IVF/ICSI cycles. Hum Reprod. 2006. 21:370–375.
21. Donnez J, Dolmans MM, Demylle D, Jadoul P, Pirard C, Squifflet J, et al. Livebirth after orthotopic transplantation of cryopreserved ovarian tissue. Lancet. 2004. 364:1405–1410.
22. Demeestere I, Simon P, Emiliani S, Delbaere A, Englert Y. Fertility preservation: Successful transplantation of cryopreserved ovarian tissue in a young patient previously treated for Hodgkin's disease. Oncologist. 2007. 12:1437–1442.
23. Sonmezer M, Oktay K. Fertility preservation in female patients. Hum Reprod Update. 2004. 10:251–266.
24. Seli E, Tangir J. Fertility preservation options for female patients with malignancies. Curr Opin Obstet Gynecol. 2005. 17:299–308.
25. Oktay K, Buyuk E, Davis O, Yermakova I, Veeck L, Rosenwaks Z. Fertility preservation in breast cancer patients: IVF and embryo cryopreservation after ovarian stimulation with tamoxifen. Hum Reprod. 2003. 18:90–95.
26. Pfister CU, Martoni A, Zamagni C, Lelli G, De Braud F, Souppart C, et al. Effect of age and single versus multiple dose pharmacokinetics of letrozole (Femara) in breast cancer patients. Biopharm Drug Dispos. 2001. 22:191–197.
27. Azim A, Oktay K. Letrozole for ovulation induction and fertility preservation by embryo cryopreservation in young women with endometrial carcinoma. Fertil Steril. 2007. 88:657–664.
28. Oktay K, Hourvitz A, Sahin G, Oktem O, Safro B, Cil A, et al. Letrozole reduces estrogen and gonadotropin exposure in women with breast cancer undergoing ovarian stimulation before chemotherapy. J Clin Endocrinol Metab. 2006. 91:3885–3890.
29. Chen C. Pregnancy after human oocyte cryopreservation. Lancet. 1986. 1:884–886.
30. Baka SG, Toth TL, Veeck LL, Jones HW Jr, Muasher SJ, Lanzendorf SE. Evaluation of the spindle apparatus of in-vitro matured human oocytes following cryopreservation. Hum Reprod. 1995. 10:1816–1820.
31. Borini A, Bonu MA, Coticchio G, Bianchi V, Cattoli M, Flamigni C. Pregnancies and births after oocyte cryopreservation. Fertil Steril. 2004. 82:601–605.
32. Porcu E. Oocyte freezing. Semin Reprod Med. 2001. 19:221–230.
33. Gook DA, Schiewe MC, Osborn SM, Asch RH, Jansen RP, Johnston WI. Intracytoplasmic sperm injection and embryo development of human oocytes cryopreserved using 1,2-propanediol. Hum Reprod. 1995. 10:2637–2641.
34. Fabbri R, Porcu E, Marsella T, Rocchetta G, Venturoli S, Flamigni C. Human oocyte cryopreservation: New perspectives regarding oocyte survival. Hum Reprod. 2001. 16:411–416.
35. Boldt J, Cline D, McLaughlin D. Human oocyte cryopreservation as an adjunct to IVF-embryo transfer cycles. Hum Reprod. 2003. 18:1250–1255.
36. Trad FS, Toner M, Biggers JD. Effects of cryoprotectants and ice-seeding temperature on intracellular freezing and survival of human oocytes. Hum Reprod. 1999. 14:1569–1577.
37. Eroglu A, Toner M, Toth TL. Beneficial effect of microinjected trehalose on the cryosurvival of human oocytes. Fertil Steril. 2002. 77:152–158.
38. Rall WF, Fahy GM. Ice-free cryopreservation of mouse embryos at -196 degrees C by vitrification. Nature. 1985. 313:573–575.
39. Trounson A. Preservation of human eggs and embryos. Fertil Steril. 1986. 46:1–12.
40. Yoon TK, Chung HM, Lim JM, Han SY, Ko JJ, Cha KY. Pregnancy and delivery of healthy infants developed from vitrified oocytes in a stimulated In vitro fertilization-embryo transfer program. Fertil Steril. 2000. 74:180–181.
41. Boiso I, Marti M, Santalo J, Ponsa M, Barri PN, Veiga A. A confocal microscopy analysis of the spindle and chromosome configurations of human oocytes cryopreserved at the germinal vesicle and metaphase II stage. Hum Reprod. 2002. 17:1885–1891.
42. Marhhom E, Cohen I. Fertility preservation options for women with malignancies. Obstet Gynecol Surv. 2007. 62:58–72.
43. Wu J, Zhang L, Wang X. In vitro maturation, fertilization and embryo development after ultrarapid freezing of immature human oocytes. Reproduction. 2001. 121:389–393.
44. Tucker MJ, Wright G, Morton PC, Massey JB. Birth after cryopreservation of immature oocytes with subsequent in vitro maturation. Fertil Steril. 1998. 70:578–579.
45. Tucker MJ, Morton PC, Wright G, Sweitzer CL, Massey JB. Clinical application of human egg cryopreservation. Hum Reprod. 1998. 13:3156–3159.
46. Practice Committee of the American Society for Reproductive Medicine . Practive Committee of the Society for Assisted Reproductive Technology. Ovarian tissue and oocyte cryopreservation. Fertil Steril. 2006. 86:S142–S147.
47. Gosden RG, Baird DT, Wade JC, Webb R. Restoration of fertility to oophorectomized sheep by ovarian autografts stored at -196 degrees C. Hum Reprod. 1994. 9:597–603.
48. Bordes A, Lornage J, Demirci B, Franck M, Courbiere B, Guerin JF, et al. Normal gestations and live births after orthotopic autograft of vitrified-warmed hemi-ovaries into ewes. Hum Reprod. 2005. 20:2745–2748.
49. Candy CJ, Wood MJ, Whittingham DG. Follicular development in cryopreserved marmoset ovarian tissue after transplantation. Hum Reprod. 1995. 10:2334–2338.
50. Salle B, Demirci B, Franck M, Rudigoz RC, Guerin JF, Lornage J. Normal pregnancies and live births after autograft of frozen-thawed hemi-ovaries into ewes. Fertil Steril. 2002. 77:403–408.
51. Almodin CG, Minguetti-Câmara VC, Meister H, Ferreira JO, Franco RL, Cavalcante AA, et al. Recovery of fertility after grafting of cryopreserved germinative tissue in female rabbits following radiotherapy. Hum Reprod. 2004. 19:1287–1293.
52. Lee DM, Yeoman RR, Battaglia DE, Stouffer RL, Zelinski-Wooten MB, Fanton JW, et al. Live birth after ovarian tissue transplant. Nature. 2004. 428:137–138.
53. Oktay K, Buyuk E, Rosenwaks Z, Rucinski J. A technique for transplantation of ovarian cortical strips to the forearm. Fertil Steril. 2003. 80:193–198.
54. Kim SS, Battaglia DE, Soules MR. The future of human ovarian cryopreservation and transplantation: fertility and beyond. Fertil Steril. 2001. 75:1049–1056.
55. Radford JA, Lieberman BA, Brison DR, Smith AR, Critchlow JD, Russell , et al. Orthotopic reimplantation of cryopreserved ovarian cortical strips after high-dose chemotherapy for Hodgkin's lymphoma. Lancet. 2001. 357:1172–1175.
56. Oktay K, Economos K, Kan M, Rucinski J, Veeck L, Rosenwaks Z. Endocrine function and oocyte retrieval after autologous transplantation of ovarian cortical strips to the forearm. JAMA. 2001. 286:1490–1493.
57. Callejo J, Salvador C, Miralles A, Vilaseca S, Lailla JM, Balasch J. Long-term ovarian function evaluation after autografting by implantation with fresh and frozen-thawed human ovarian tissue. J Clin Endocrinol Metab. 2001. 86:4489–4494.
58. Kim SS, Hwang IT, Lee HC. Heterotopic autotransplantation of cryobanked human ovarian tissue as a strategy to restore ovarian function. Fertil Steril. 2004. 82:930–932.
59. Wølner-Hanssen P, Hägglund L, Ploman F, Ramirez A, Manthorpe R, Thuring A. Autotransplantation of cryopreserved ovarian tissue to the right forearm 4(1/2) years after autologous stem cell transplantation. Acta Obstet Gynecol Scand. 2005. 84:695–698.
60. Oktay K, Newton H, Mullan J, Gosden RG. Development of human primordial follicles to antral stages in SCID/hpg mice stimulated with follicle stimulating hormone. Hum Reprod. 1998. 13:1133–1138.
61. Gook DA, Edgar DH, Borg J, Archer J, Lutjen PJ, McBain JC. Oocyte maturation, follicle rupture and luteinization in human cryopreserved ovarian tissue following xenografting. Hum Reprod. 2003. 18:1772–1781.
62. Gook DA, Osborn SM, Archer J, Edgar DH, McBain J. Follicle development following cryopreservation of human ovarian tissue. Eur J Obstet Gynecol Reprod Biol. 2004. 113:Suppl 1. S60–S62.
63. Lucifero D, Mertineit C, Clarke HJ, Bestor TH, Trasler JM. Methylation dynamics of imprinted genes in mouse germ cells. Genomics. 2002. 79:530–538.
64. Martinez-Madrid B, Dolmans MM, Langendonckt AV, Defrère S, Van Eyck AS, Donnez J. Ficoll density gradient method for recovery of isolated human ovarian primordial follicles. Fertil Steril. 2004. 82:1648–1653.
65. Torrents E, Boiso I, Barri PN, Veiga A. Applications of ovarian tissue transplantation in experimental biology and medicine. Hum Reprod Update. 2003. 9:471–481.
66. Smitz JE, Cortvrindt RG. The earliest stages of folliculogenesis in vitro. Reproduction. 2002. 123:185–202.
67. Abir R, Fisch B, Nitke S, Okon E, Raz A, Ben Rafael Z. Morphological study of fully and partially isolated early human follicles. Fertil Steril. 2001. 75:141–146.
68. Laschke MW, Menger MD, Vollmar B. Ovariectomy improves neovascularization and microcirculation of freely transplanted ovarian follicles. J Endocrinol. 2002. 172:535–544.
69. Nisolle M, Casanas-Roux F, Qu J, Motta P, Donnez J. Histologic and ultrastructural evaluation of fresh and frozen-thawed human ovarian xenografts in nude mice. Fertil Steril. 2000. 74:122–129.
70. Liu J, Van der Elst J, Van den Broecke R, Dhont M. Early massive follicle loss and apoptosis in heterotopically grafted newborn mouse ovaries. Hum Reprod. 2002. 17:605–611.
71. Wang X, Chen H, Yin H, Kim SS, Lin Tan S, Gosden RG. Fertility after intact ovary transplantation. Nature. 2002. 415:385.
72. Winston RM, Browne JC. Pregnancy following autograft transplantation of Fallopian tube and ovary in the rabbit. Lancet. 1974. 2:494–495.
73. Jeremias E, Bedaiwy MA, Gurunluoglu R, Biscotti CV, Siemionow M, Falcone T. Heterotopic autotransplantation of the ovary with microvascular anastomosis: A novel surgical technique. Fertil Steril. 2002. 77:1278–1282.
74. Paldi E, Gal D, Barzilai A, Hampel N, Malberger E. Genital organs. Auto and homotransplantation in forty dogs. Int J Fertil. 1975. 20:5–12.
75. Scott JR, Keye WR, Poulson AM, Reynolds WA. Microsurgical ovarian transplantation in the primate. Fertil Steril. 1981. 36:512–515.
76. Leporrier M, von Theobald P, Roffe JL, Muller G. A new technique to protect ovarian function before pelvic irradiation. Heterotopic ovarian autotransplantation. Cancer. 1987. 60:2201–2204.
77. Yin H, Wang X, Kim SS, Chen H, Tan SL, Gosden RG. Transplantation of intact rat gonads using vascular anastomosis: Effects of cryopreservation, ischaemia and genotype. Hum Reprod. 2003. 18:1165–1172.
78. Bedaiwy MA, Jeremias E, Gurunluoglu R, Hussein MR, Siemianow M, Biscotti C, et al. Restoration of ovarian function after autotransplantation of intact frozen-thawed sheep ovaries with microvascular anastomosis. Fertil Steril. 2003. 79:594–602.
79. Martinez-Madrid B, Dolmans MM, Van Langendonckt A, Defrere S, Donnez J. Freeze-thawing intact human ovary with its vascular pedicle with a passive cooling device. Fertil Steril. 2004. 82:1390–1394.
80. Bedaiwy MA, Hussein MR, Biscotti C, Falcone T. Cryopreservation of intact human ovary with its vascular pedicle. Hum Reprod. 2006. 21:3258–3269.
81. Shaw JM, Bowles J, Koopman P, Wood EC, Trounson AO. Fresh and cryopreserved ovarian tissue samples from donors with lymphoma transmit the cancer to graft recipients. Hum Reprod. 1996. 11:1668–1673.
82. Shaw J, Trounson A. Oncological implications in the replacement of ovarian tissue. Hum Reprod. 1997. 12:403–405.
83. Meirow D, Hardan I, Dor J, Fridman E, Elizur S, Ra'anani H, et al. Searching for evidence of disease and malignant cell contamination in ovarian tissue stored from hematologic cancer patients. Hum Reprod. 2008. 23:1007–1013.
84. Liede A, Narod SA. Hereditary breast and ovarian cancer in Asia: Genetic epidemiology of BRCA1 and BRCA2. Hum Mutat. 2002. 20:413–424.
85. Kauff ND, Satagopan JM, Robson ME, Scheuer L, Hensley M, Hudis CA, et al. Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med. 2002. 346:1609–1615.
86. Kim SS, Kang HG, Kim NH, Lee HC, Lee HH. Assessment of the integrity of human oocytes retrieved from cryopreserved ovarian tissue after xenotransplantation. Hum Reprod. 2005. 20:2502–2508.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download