Abstract
Epithelioid sarcoma of vulva is extremely rare. Only 20 cases have been reported in the literature so far. Early diagnosis is difficult because of its benign appearance as a painless subcutaneous nodule. Therefore treatment can be delayed, although epithelioid sarcoma requires prompt surgery. We report a case of epithelioid sarcoma that occurred in the left vulva with a brief review of literature.
Epithelioid sarcoma is a malignant soft tissue tumor that was established as a distinct disease entity by Enzinger in 1970, and which usually arises in the hand and forearm of young adults.1 Epithelioid sarcomas of the vulva are extremely rare, and only 20 cases have been reported in the literature so far.2,3 Epithelioid sarcomas occurring in the perineum and pubic regions have a higher rate of local recurrence and distant metastasis than those occurring in the upper and lower extremities. For this reason, epithelioid sarcomas are classified into "distal type" that occurs in the upper and lower extremities, and "proximal type" that occurs in the trunk and pubic region.4 Optimal treatment for epithelioid sarcoma of the vulva is not been known due to its rarity. We report a case of epithelioid sarcoma that occurred in the left vulva of a 24 year-old female patient that was treated with wide local excision.
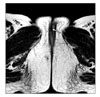
A 24-year-old nulli-gravida woman visited a private clinic due to a palpable nodule in the upper part of the left labium majus. Her gynecologist regarded the lesion as a benign condition. She visited again the same clinic 2 months after the initial visit because her symptom had not improved. Her gynecologist performed a biopsy of the lesion. Histological examination showed atypical cells and therefore she was referred to our hospital. She had negative personal and family history for other diseases. Inspection of the vulva showed a mass of 1 cm diameter in the left labium majus. Physical examination of the mass revealed a smooth surfaced, hard consistency and non-tender nodule. No other abnormalities were found by physical examination. We reviewed the biopsy specimen of the private clinic. The tentative diagnosis of epithelioid sarcoma was made. Magnetic Resonance Imaging of the pelvis showed a soft tissue tumor of 1 cm diameter in the upper portion of the left vulva, and no pelvic and inguinal lymphadenopathy (Fig. 1). Positron Emission Tomography did not reveal hypermetabolism in the vulva lesion and did not show any evidence of metastasis. We decided to treat the patient with clitoris sparing wide local excision with a 2 cm safety margin. However the safety margin of medial side of the tumor was 1.5 cm because the clitoris was close to the mass. Inguinal lymphadenectomy was not performed.
The surgical specimen was sent to our pathology department. The sections revealed a skin fragment measuring 2.0×1.5 cm with a mildly thickened epidermis. In the dermis, a well-circumscribed lobular nodule was seen. The nodule consisted of spindles or polygonal epithelioid cells. The cells had irregular vesicular nuclei with eosinophilic nucleolus. Immunohistochemistry revealed strong positive for cytokeratin and vimentin staining (Fig. 2). Finally, she was diagnosed as epithelioid sarcoma. She underwent no postoperative adjuvant therapy. Eight months after operation she is well without evidence of disease.
Epithelioid sarcoma is a rare malignant soft tissue tumor of mesenchymal origin. Most epithelioid sarcomas occur in the upper and lower extremities of the young adults (distal type), while epithelioid sarcomas occurring in the gastrointestinal tract, urogenital organs and vulva (proximal type) have poorer prognosis than the distal type epithelioid sarcoma.3,5,6 Vulvar sarcomas account for 5% of the primary malignant vulvar tumors. The most common type is leiomyosarcoma, and other types are malignant fibrous histiocytoma, malignant rhabdoid tumor, angiosarcoma, rhabdomyosarcoma and epithelioid sarcoma.7,8 Among these tumors, epithelioid sarcoma of the vulva is extremely rare, and only 20 cases have been reported so far. Epithelioid sarcoma is difficult to diagnose histologically, because histologic findings of epithelioid sarcoma are similar to squamous cell carcinomas, necrotizing granulomas, synovial sarcomas or malignant rhabdoid tumors. Useful histologic findings to differentiate epithelioid sarcoma from other tumors are nodularity, frequent necrosis, eosinophilic polygonal epithelioid cells in the nest, and tendency to form the cleft.1 Immunohistochemistry of epithelioid sarcoma reveals cytoplasmic immunoreactivity for cytokeratin and vimentin, negative for S 100 and CD31 stainings. These findings are useful to differentiate epithelioid sarcoma from other soft tissue sarcomas.4,9 Immunohistochemistry also showed positive staining for cytokeratin and vimentin in our case. Epithelioid sarcomas present usually with a painless subcutaneous nodule and mass with ulcerative surface in 10-12%.3 Because these non specific findings are also shown in benign lesions (such as infectious granuloma, Bartholin cyst, fibroma, lipoma or teratoma), epithelioid sarcoma can easily be mistaken for these benign conditions. These misdiagnoses often lead to inadequate management or treatment delay.3 In our case, because her disease was regarded as a benign condition, adequate treatment was delayed for 2 months without any treatment. She had had a biopsy of the left vulvar mass after 2 months following the visit to the private clinic and the possibility of malignancy was raised. The treatment of epithelioid sarcoma of the vulva should in principal consist of wide local excision of the lesion. However adequate safety margin is difficult to be defined. Based on vulva carcinoma, we resected the tumor with a 2 cm safety margin. Furthermore extrapolating data from the extragenital location, it is recommended to aim for a margin of at least 2 cm.10 It is controversial whether the inguinal lymph nodes should be resected. The removal of the locoregional lymph nodes should only be considered if they are suspicious or enlarged at physical or imaging examination. There is no evidence that the resection of metastatically invaded locoregional lymph nodes has any beneficial effect on the local or distant recurrence rate. Postoperative radiotherapy is commonly used in the distal type epithelioid sarcoma because it reduces the incidence of amputation through the reduction of the local recurrence, but its role in the vulvar epithelioid sarcoma is controversial.11 In a recent report regarding vulvar epithelioid sarcoma, patients who received adjuvant radiotherapy after surgical resection had a recurrence rate of 14% compared to 71% for those who did not (p=0.01). However adjuvant radiotherapy did not show statistically significant reduction in mortality from the disease.2 Other reports advocate adjuvant radiotherapy in the presence of high-grade tumors or inadequate surgical margins.6 The role of postoperative chemotherapy is questionable. Argenta et al.2 reported in a study of 31 cases of vulva epithelioid sarcoma or malignant rhabdoid tumor that adjuvant chemotherapy were applied as a front-line therapy in 7 patients, of which 3 were disease free at 8, 11, and 21 months. The other 4 died of disseminated disease within 8 months of diagnosis. We explained to our patient the results of previous adjuvant therapy and possible complications such as sexual dysfunction. She underwent only surgical resection without adjuvant therapy. The 5 year overall survival rates for "distal-type" epithelioid sarcoma range from 50% to 80%, but those for "proximal-type" appear worse. Centrally located distal lesions such as the vulva and inguinal area accompanied by 65% tumor-related mortality, and 75% local or distant metastasis.6,10,11 Factors such as tumor size, grade and surgical margin had prognostic significance for the sarcoma occurring in the urinary or gastrointestinal tract. However, these prognostic factors have not been established for vulvar epithelioid sarcoma due to its rare incidence.12,13 In conclusion, vulvar epithelioid sarcoma is extremely rare, but reveals aggressive behavior. Clinical suspicion and early diagnosis is important since this is commonly mistaken for a benign lesion. Wide local excision with adequate margins (at least 2 cm) is recommended.
Figures and Tables
References
1. Enzinger FM. Epitheloid sarcoma: A sarcoma simulating a granuloma or a carcinoma. Cancer. 1970. 26:1029–1041.
2. Argenta PA, Thomas S, Chura JC. Proximal-type epithelioid sarcoma vs malignant rhabdoid tumor of the vulva: A case report, review of the literature, and an argument for consolidation. Gynecol Oncol. 2007. 107:130–135.
3. Tjalma WA, Hauben EI, Deprez SM, Van Marck EA, van Dam PA. Epithelioid sarcoma of the vulva. Gynecol Oncol. 1999. 73:160–164.
4. Guillou L, Wadden C, Coindre JM, Krausz T, Fletcher CD. "Proximal-type" epithelioid sarcoma, a distinctive aggressive neoplasm showing rhabdoid features. Clinicopathologic, immunohistochemical, and ultrastructural study of a series. Am J Surg Pathol. 1997. 21:130–146.
5. Halling AC, Wollan PC, Pritchard DJ, Vlasak R, Nascimento AG. Epithelioid sarcoma: A clinicopathologic review of 55 cases. Mayo Clin Proc. 1996. 71:636–642.
6. Hasegawa T, Matsuno Y, Shimoda T, Umeda T, Yokoyama R, Hirohashi S. Proximal-type epithelioid sarcoma: A clinicopathologic study of 20 cases. Mod Pathol. 2001. 14:655–663.
7. Audet-Lapointe P, Paquin F, Guerard MJ, Charbonneau A, Methot F, Morand G. Leiomyosarcoma of the vulva. Gynecol Oncol. 1980. 10:350–355.
8. DiSaia PJ, Rutledge F, Smith JP. Sarcoma of the vulva: Report of 12 patients. Obstet Gynecol. 1971. 38:180–184.
9. Kasamatsu T, Hasegawa T, Tsuda H, Okada S, Sawada M, Yamada T, et al. Primary epithelioid sarcoma of the vulva. Int J Gynecol Cancer. 2001. 11:316–320.
10. Bos GD, Pritchard DJ, Reiman HM, Dobyns JH, Ilstrup DM, Landon GC. Epithelioid sarcoma: An analysis of fifty-one cases. J Bone Joint Surg Am. 1988. 70:862–870.
11. Evans HL, Baer SC. Epithelioid sarcoma: A clinicopathologic and prognostic study of 26 cases. Semin Diagn Pathol. 1993. 10:286–291.
12. Conlon KC, Casper ES, Brennan MF. Primary gastrointestinal sarcomas: Analysis of prognostic variables. Ann Surg Oncol. 1995. 2:26–31.
13. Russo P, Brady MS, Conlon K, Hajdu SI, Fair WR, Herr HW, et al. Adult urological sarcoma. J Urol. 1992. 147:1032–1036.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download