Abstract
Objective
The purpose of this study was to compare the accuracy of pelvic examination versus imaging modality such as computed tomography (CT) or magnetic resonance imaging (MRI) in the measurement of the tumor size of invasive cervical carcinoma based on pathologic findings.
Methods
Patients with stage Ib-II cervical cancer who underwent primary surgical treatment between January 2003 and December 2005 were evaluated retrospectively. One hundred three consecutive patients aged 24 to 81 years (mean age, 50.6 years), who had not received any treatment previously were included in this study. Accuracy of preoperative CT or MRI versus pelvic examination in the measurement of tumor size was compared based on pathologic findings. All patients were examined and staged clinically by the gynecologic oncologist. Surgery was performed within 2 weeks after imaging studies. The data were analyzed using descriptive statistics.
Results
The largest diameter of the tumor measured by pathologic findings was 2.76±1.76 cm. Based on pathologic findings, accuracy was estimated by the degree of agreement with a difference of <0.5 or 1.0 cm between the measurements of tumor size obtained by pelvic examination and imaging modality. Pelvic examination and imaging modality had an accuracy of 46.6% and 39.8%, respectively, with a difference of <0.5 cm, and an accuracy of 72.8% and 55.3%, respectively, with a difference of <1.0 cm. Correlation with pathologic findings was higher for pelvic examination (rs=0.680) than for imaging modality (rs=0.410). In determining the size of tumor mass differentiating >4.0 cm from ≤4.0 cm, imaging modality showed higher accuracy than pelvic examination.
Cervical cancer is the most common gynecologic malignancy in Korea.1 Cervical cancer is one of the malignancies whose stage can be clinically decided. The management of cervical cancer, particularly its surgical treatment, differs largely depending on the stage of the disease. Early cervical cancer can be cured with surgery. However, postoperative adjuvant therapy should be considered if pathologic findings demonstrate risk factors including lymph node metastases, deep cervical invasion, positive resection margin, parametrial invasion and bulkiness of tumor.2-4 Among them, parametrial invasion and tumor size are evaluated by preoperative pelvic examination.
If clinicians perform an exact pelvic examination, patients can avoid unnecessary surgery. Thus, pelvic examination is important for the decision of further management because pelvic examination is the major diagnostic tool for cervical cancer. Despite the importance of pelvic examination, pelvic examination is often ignored due to the development of imaging studies such as computed tomography (CT) or magnetic resonance imaging (MRI).
The objective of this study was to determine whether pelvic examination by a gynecologic oncologist could yield reliable diagnostic results as a diagnostic tool compared to imaging modality for cervical cancer.
Between January 2003 and December 2005, 453 patients were diagnosed with cervical cancer. The patients' medical records were retrospectively reviewed, and the women were included if they satisfied the following criteria.
Inclusion criteria included clinically visible cervical cancer, pelvic examination prior to imaging studies, preoperative imaging studies with CT or MRI, surgical treatment as the primary therapy, and a time interval from pelvic examination to surgery of <3 weeks.
Exclusion criteria included diagnostic workups including pelvic examination or imaging at other hospitals, surgery at other hospitals, and other treatments before surgery.
All patients were evaluated by a gynecologic oncologist who had worked at the gynecologic oncology clinic for more than 6 years. The examiner determined the maximum tumor diameter, the site of the tumor, the growth pattern of the tumor and the presence of vaginal or parametrial involvement. Evaluation was aided by colposcopy.
After pelvic examination, CT imaging was performed on 58 patients, and MRI was performed on 70 patients. Both CT and MRI studies were performed on 25 patients. CT imaging was performed by using 16-slice CT equipment (SOMATOM Sensation 16, Siemens, Forchheim, Germany) through the entire abdomen and pelvis after intravenous administration of contrast. CT images were obtained in the transverse plane in 1 cm slice-thickness. MRI was performed using the Signa 1.5-T system (General Electric Medical Systems, Milwaukee, WI) through the pelvis. High-resolution sagittal, axial, transverse T1- and T2-weighted images were obtained in 3 mm slice-thickness. CT and MR images were read by 2 experienced radiologists.
The fresh radical hysterectomy pathologic specimen was examined by the same experienced pathologist (P.I.A.) and the maximum tumor diameter was recorded as the "true" value.
Measurements of the tumor by pelvic examination and imaging modalities were compared based on the maximum diameter measured by pathologic findings. We categorized the maximum tumor diameter as ≤1 cm, 1.1-2 cm, 2.1-3 cm, 3.1-4 cm, and >4 cm. Differences in accuracy were tested for statistical significance using the McNemar χ2 tests at p=0.05. The linear correlation between the categorized diameters as determined by pathologic findings and the diameters determined by pelvic examination and imaging modality was evaluated using the Spearman correlation coefficient, and agreement was estimated using simple κ statistics. All statistical analyses were performed using SPSS 12.0 (SPSS Inc, Chicago, IL).
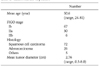
Among 453 patients, 103 met the criteria for this study. Table 1 indicates the characteristics of the patients. Most of the patients belonged to stage Ib or IIa, however, 6 women had findings consistent with stage IIb. Since the patients with advanced cervical cancer (stage IIb) were less than 50 years of age, the clinicians tried to perform surgical treatment combined with postoperative adjuvant therapy for these patients. Tumor size was 2.76±1.76 cm (mean of the maximum diameter±standard deviation), and ranged from 0.5 cm to 8.0 cm at pathologic evaluation. Histologic examination of the majority of patients revealed squamous cell carcinoma.
Experience of gynecologic oncologists was as follows: 6 to 10 years in 2 oncologists; 11 to 15 years in 1 oncologist; and ≥16 years in 2 oncologists. Tumor size measured by pelvic examination ranged from 0.5 to 6.0 cm. Tumor size measured by imaging modality ranged from 0 cm to 7.0 cm. We defined no definite mass as 0 cm.
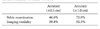
Table 2 depicts the accuracy of pelvic examination and imaging modality including CT and MRI in the measurement of tumor size compared with the "true" value. Based on pathologic findings, accuracy was estimated by the degree of agreement with a difference of 0.5 or 1.0 cm. Pelvic examination was more accurate in the evaluation of tumor size than imaging modality with a difference of both 0.5 and 1.0 cm, and the accuracy rate of pelvic examination was significantly higher than that of imaging modality (72.8% vs. 55.3%, p=0.004). Descriptive statistics for tumor size measurement categorized at 1.0-cm intervals are shown in Table 3. The correlation with pathologic findings was higher for pelvic examination than for imaging modality (rs=0.680 vs. rs=0.410, p<0.0001) (Fig. 1).
The accuracy of each method in the measurement of tumor size is shown in Table 4. The accuracy of both pelvic examination and imaging modality for the evaluation of tumor size become lower as tumor size decreased. However, the accuracy of pelvic examination for the evaluation of tumor size declined more than that of imaging modality. Moreover, imaging modality was accurate especially in the evaluation of bulky tumor.
Apart from other gynecologic malignancies such as ovarian cancer and endometrial cancer whose stages are surgically determined, the stage of cervical cancer is clinically determined. Thus, there are numerous prognostic factors which are not determinants of stage in cervical cancer. Since some pathologic parameters are related to patients' prognosis, these parameters affect the plan of further treatment.4-6 This means that pathologic findings of surgical specimens are important for the management of patients with cervical cancer. However, clinicians should consider preoperative diagnosis, because the stage of cervical cancer is clinically determined and clinicians can get much information related with prognosis from preoperative diagnosis. Tumor size has been suggested as an important prognostic factor in patients with cervical cancer.7-11 Although there are several diagnostic methods including pelvic examination, intravenous pyelogram, cystoscopy, proctoscopy and others, pelvic examination is the only single method for evaluating the size, location and parametrial invasion of the cervical mass. Thus, exact pelvic examination is important for the management of patients with cervical cancer.
Recent development of imaging techniques has made it possible to evaluate not only the characteristics of cervical mass but also the status of lymph nodes.12,13 Imaging diagnosis using CT or MRI plays an important role for cancer patients in Korea because these imaging machineries are popular and also because National Health Insurance covers a large portion of medical fee for CT or MRI in Korea. Thus, CT or MRI has progressively replaced standard diagnostic methods of cervical cancer. Moreover, some clinicians make a decision for the management of cervical cancer using imaging tools such as CT or MRI instead of the standard pelvic examination.
Could these imaging tools replace pelvic examination? The current study demonstrates the accuracy of pelvic examination and the imaging modality including CT or MRI for the evaluation of cervical mass in 103 cervical cancer patients. The real size of cervical mass ranged from 0.5 to 8.0 cm in pathologic findings. Compared with the size of the cervical mass evaluated by pathologic findings, pelvic examination estimated the size of the cervical mass more accurately than imaging modality. Many previous studies have focused on the value of imaging modality as new diagnostic method for evaluating tumor size, parametrial invasion and lymph node involvement.14-16 Although quite a few studies have reported the value of pelvic examination in cervical cancer, it has been demonstrated that the accuracy of pelvic examination is 50% with a difference of <1.0 cm from the actual values and that it is 52% with a 25% difference between clinical and pathologic measurements of tumor diameter.17,18 On the contrary, some other investigators have reported the accuracy of pelvic examination ranged from 64% to 68%.19,20 Our results showed similar accuracy rates compared with these latter reports. However, the accuracy of pelvic examination with a difference of <0.5 cm was 46.6%, and the accuracy of pelvic examination with a difference of 1.0 cm was 57.9% in the patients with the cervical mass >2.0 cm. These results were similar to findings of the former previous studies.
The accuracy of imaging modality was about 55% in agreement within 1.0 cm for tumor diameter. Many investigators have reported the value of CT or MRI in patients with cervical cancer. Nonetheless, most of them focused on the lymph node status and parametrial invasion. However, some investigators have found the accuracy of MRI ranged about from 30% to 70% according to the tumor size.21,22 Some reports have demonstrated the accuracy of MRI in the evaluation of the stage of cervical cancer ranged from 70% to 85%.23-25 These results indicate higher accuracy rate of imaging modality than those of our study. However, a comparative study has reported the accuracy of CT and MRI to be 51% and 75%, respectively in the evaluation of cervical cancer.24 Above all, a prospective study with a large sample size has demonstrated that the accuracy of CT and MRI is overestimated in the diagnosis of cervical cancer, with the accuracy of CT and MRI being 42% and 53%, respectively.26 This result was in accord with that of our study.
However, imaging modality was more accurate than pelvic examination in cases where the size of the cervical mass exceeds 4.0 cm. In addition, if a cervical tumor existed at the endocervix, the discordance between tumor diameters measured by pelvic examination and pathologic findings appears to become larger. Thus, imaging studies could be good methods for evaluating bulky masses which are >4.0 cm and are difficult to find at the exocervix. Mayr et al. also has reported MRI was more useful in tumors larger than 4.0 cm in cervical cancer patients.22
In conclusion, pelvic examination is an accurate and reliable method for evaluating the tumor size of cervical cancer. However, this study has some limitations because it was not a prospective study with a standardized examination method, and the difference between CT and MRI was not considered. Further prospective studies for evaluating pelvic examination with the standard technique are needed to confirm these findings.
Figures and Tables
Fig. 1
Correlation between the measurements estimated by pelvic examination and imaging modality based on pathologic findings. (A) Scattergram between the measurements estimated by pelvic examination and pathologic findings in patients with cervical cancer. (B) Scattergram between the measurements estimated by imaging modality and pathologic findings in patients with cervical cancer.

References
1. Korean Society of Obstetrics and Gynecology, Committee of Gynecologic Oncology. Annual report of gynecologic cancer registry program in Korea for 2004 (2004.1.1-2004.12.31). Korean J Obstet Gynecol. 2007. 50:28–78.
2. Lai CH, Hong JH, Hsueh S, Ng KK, Chang TC, Tseng CJ, et al. Preoperative prognostic variables and the impact of postoperative adjuvant therapy on the outcomes of Stage IB or II cervical carcinoma patients with or without pelvic lymph node metastases: An analysis of 891 cases. Cancer. 1999. 85:1537–1546.
3. Sedlis A, Bundy BN, Rotman MZ, Lentz SS, Muderspach LI, Zaino RJ. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: A Gynecologic Oncology Group Study. Gynecol Oncol. 1999. 73:177–183.
4. Zaino RJ, Ward S, Delgado G, Bundy B, Gore H, Fetter G, et al. Histopathologic predictors of the behavior of surgically treated stage IB squamous cell carcinoma of the cervix. A Gynecologic Oncology Group study. Cancer. 1992. 69:1750–1758.
5. Vinh-Hung V, Bourgain C, Vlastos G, Cserni G, De Ridder M, Storme G, et al. Prognostic value of histopathology and trends in cervical cancer: A SEER population study. BMC Cancer. 2007. 7:164.
6. Metindir J, Bilir G. Prognostic factors affecting disease-free survival in early-stage cervical cancer patients undergoing radical hysterectomy and pelvic-paraaortic lymphadenectomy. Eur J Gynaecol Oncol. 2007. 28:28–32.
7. Chung CK, Nahhas WA, Stryker JA, Curry SL, Abt AB, Mortel R. Analysis of factors contributing to treatment failures in stages IB and IIA carcinoma of the cervix. Am J Obstet Gynecol. 1980. 138:550–556.
8. Homesley HD, Raben M, Blake DD, Ferree CR, Bullock MS, Linton EB, et al. Relationship of lesion size to survival in patients with stage IB squamous cell carcinoma of the cervix uteri treated by radiation therapy. Surg Gynecol Obstet. 1980. 150:529–531.
9. Kristensen GB, Abeler VM, Risberg B, Trop C, Bryne M. Tumor size, depth of invasion, and grading of the invasive tumor front are the main prognostic factors in early squamous cell cervical carcinoma. Gynecol Oncol. 1999. 74:245–251.
10. Trattner M, Graf AH, Lax S, Forstner R, Dandachi N, Haas J, et al. Prognostic factors in surgically treated stage ib-iib cervical carcinomas with special emphasis on the importance of tumor volume. Gynecol Oncol. 2001. 82:11–16.
11. Horn LC, Fischer U, Raptis G, Bilek K, Hentschel B. Tumor size is of prognostic value in surgically treated FIGO stage II cervical cancer. Gynecol Oncol. 2007. 107:310–315.
12. Choi HJ, Kim SH, Seo SS, Kang S, Lee S, Kim JY, et al. MRI for pretreatment lymph node staging in uterine cervical cancer. AJR Am J Roentgenol. 2006. 187:W538–W543.
13. Soutter WP, Hanoch J, D'Arcy T, Dina R, McIndoe GA, DeSouza NM. Pretreatment tumour volume measurement on high-resolution magnetic resonance imaging as a predictor of survival in cervical cancer. BJOG. 2004. 111:741–747.
14. Arimoto T. Significance of computed tomography-measured volume in the prognosis of cervical carcinoma. Cancer. 1993. 72:2383–2388.
15. Botsis D, Gregoriou O, Kalovidouris A, Tsarouchis K, Zourlas PA. The value of computed tomography in staging cervical carcinoma. Int J Gynaecol Obstet. 1988. 27:213–218.
16. Camilien L, Gordon D, Fruchter RG, Maiman M, Boyce JG. Predictive value of computerized tomography in the presurgical evaluation of primary carcinoma of the cervix. Gynecol Oncol. 1988. 30:209–215.
17. Hoffman MS, Cardosi RJ, Roberts WS, Fiorica JV, Grendys EC Jr, Griffin D. Accuracy of pelvic examination in the assessment of patients with operable cervical cancer. Am J Obstet Gynecol. 2004. 190:986–993.
18. Alvarez RD, Potter ME, Soong SJ, Gay FL, Hatch KD, Partridge EE, et al. Rationale for using pathologic tumor dimensions and nodal status to subclassify surgically treated stage IB cervical cancer patients. Gynecol Oncol. 1991. 43:108–112.
19. Averette HE, Ford JH Jr, Dudan RC, Girtanner RE, Hoskins WJ, Lutz MH. Staging of cervical cancer. Clin Obstet Gynecol. 1975. 18:215–232.
20. Van Nagell JR Jr, Roddick JW Jr, Lowin DM. The staging of cervical cancer: Inevitable discrepancies between clinical staging and pathologic findinges. Am J Obstet Gynecol. 1971. 110:973–978.
21. Hricak H, Lacey CG, Sandles LG, Chang YC, Winkler ML, Stern JL. Invasive cervical carcinoma: Comparison of MR imaging and surgical findings. Radiology. 1988. 166:623–631.
22. Mayr NA, Yuh WT, Zheng J, Ehrhardt JC, Sorosky JI, Magnotta VA, et al. Tumor size evaluated by pelvic examination compared with 3-D quantitative analysis in the prediction of outcome for cervical cancer. Int J Radiat Oncol Biol Phys. 1997. 39:395–404.
23. Sironi S, De Cobelli F, Scarfone G, Colombo E, Bolis G, Ferrari A, et al. Carcinoma of the cervix: Value of plain and gadolinium-enhanced MR imaging in assessing degree of invasiveness. Radiology. 1993. 188:797–801.
24. Kim SH, Choi BI, Han JK, Kim HD, Lee HP, Kang SB, et al. Preoperative staging of uterine cervical carcinoma: Comparison of CT and MRI in 99 patients. J Comput Assist Tomogr. 1993. 17:633–640.
25. Togashi K, Nishimura K, Sagoh T, Minami S, Noma S, Fujisawa I, et al. Carcinoma of the cervix: Staging with MR imaging. Radiology. 1989. 171:245–251.
26. Hricak H, Gatsonis C, Chi DS, Amendola MA, Brandt K, Schwartz LH, et al. Role of imaging in pretreatment evaluation of early invasive cervical cancer: Results of the intergroup study American College of Radiology Imaging Network 6651-Gynecologic Oncology Group 183. J Clin Oncol. 2005. 23:9329–9337.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download