INTRODUCTION
Plexiform angiomyxoid myofibroblastic tumor (PAMT) is a very rare mesenchymal tumor of the gastrointestinal (GI) tract. Miettinen et al. [
1] reported that the incidence of gastric PAMT is less than 1/150 of the incidence of gastric gastrointestinal stromal tumor (GIST). PAMT has emerged as a new gastric tumor entity since Takahashi et al. [
2] first described it in 2007. In Korea, only 3 cases of PAMT have been reported thus far [
34].
PAMT is also called plexiform angiomyxoma [
5] or plexiform angiomyxoid tumor [
1]. The term plexiform fibromyxoma was added as the diagnostic term instead of PAMT in the 2010 World Health Organization (WHO) Classification of Tumors of the Digestive System. The name of the tumor represents its unique histopathological features, which are cytologically bland plexiform-arranged spindle cells, and a myxoid stroma that is positive for Alcian blue staining and shows a marked proliferation of small vessels [
2]. Gastric PAMT can be distinguished from other mesenchymal tumors by these pathologic features. Here, we present a case of asymptomatic gastric PAMT that was pathologically confirmed after surgical resection.
CASE REPORT
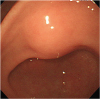
A 51-year-old man visited the Samsung Medical Center for further evaluation of the lesion suspected as submucosal tumor of the stomach, which was detected by esophagogastroduodenoscopy during a regular check-up. The patient did not have any abdominal complaints or abnormal laboratory findings. No enlargement of lymph nodes was observed at the peritoneum or retroperitoneum. Endoscopy revealed a round, elevated, subepithelial, and 3 cm tumor-like lesion without mucosal ulceration, at the antrum and lesser curvature of the stomach (
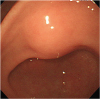
Fig. 1). Computed tomography demonstrated a 1.5 cm mass with prominent contrast enhancement, which was suspected to be a GIST (
Fig. 2). Endoscopic biopsy showed chronic gastritis. Subsequently, the patient underwent laparoscopic gastric wedge resection. A 2.0×1.5 cm cystic mass was identified in the submucosal layer. The resection margin was clear. The cut section of the mass showed a well-defined firm and whitish mass (
Fig. 3A). Histopathological findings of the resected mass revealed a submucosal multinodular cyst measuring 1.9×1.4 cm. The tumor showed microscopically infiltrative growth into the smooth muscle bundles of the muscularis propria (
Fig. 3B). There were loose myxoid and cellular areas of the tumor admixed with smooth muscle cells on high-powered microscopic fields (
Fig. 3C). Immunohistochemical staining showed that the tumor cells were positive for smooth muscle actin (SMA) (
Fig. 3D) and negative for c-kit (
Fig. 3E). The myxoid matrix was positive for Alcian blue staining. These immunohistopathological findings were in accordance with PAMT. At the 3-year follow-up, the patient was alive, without any tumor recurrence.
Fig. 1
Esophagogastroduodenoscopy shows a smooth, normal mucosa-covered elevated lesion at the gastric antrum.
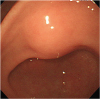
Fig. 2
Computed tomography shows a well-marginated cystic lesion, suspected to be a GIST, glomus tumor, or neuroendocrine tumor.
GIST = gastrointestinal stromal tumor.

Fig. 3
(A) Tumor surgically removed by laparoscopic wedge resection. Cut section shows a well-defined whitish and firm mass. (B) Tumor demonstrates infiltrative growth of cellular areas into smooth muscle bundles in the muscularis propria. (C) Tumor shows loose myxoid areas (left part) and cellular areas (right part) admixed with smooth muscle cells. (D) Smooth muscle fibers and tumor cells positive for smooth muscle actin (×200). (E) Tumor cells negative for c-kit. Mast cells were positively stained as an internal positive control (arrows).

DISCUSSION
PAMT is a very rare mesenchymal tumor along the GI tract. To date, more than 60 cases have been reported worldwide as PAMT or plexiform fibromyxoma. The tumor shows a similar incidence in both genders, and it occurs over a wide age range (7–75 years) [
46]. The majority of PAMTs were found in the stomach, with only one case reported in the duodenum [
7]. Most gastric PAMTs occurred in the gastric antrum, but they could be located anywhere in the stomach [
46].
Gastric PAMT can cause abdominal symptoms such as palpable abdominal mass, pain, vomiting, and weight loss, or can be an asymptomatic, incidental finding [
12]. Some patients also presented with GI bleeding, gastric outlet obstruction, ulcer, anemia, or fistulating abscess formation [
8]. Malignant transformation of gastric PAMT has not yet been reported in the literature, and it has been considered as a benign tumor. Histological features such as bland nuclear morphology, low proliferative index, and lack of necrosis imply that a PAMT is a benign tumor [
3].
However, it is not evident whether a gastric PAMT will be permanently benign or whether it could undergo malignant transformation. As PAMT is a rare disease, the limited number of reported cases are insufficient to draw any conclusion. In addition, results on long-term studies on PAMT are lacking. Moreover, PAMT may be diagnosed as one of the other submucosal tumors such as GIST, leiomyoma, neurofibroma, etc. Our findings of this rare condition will promote further studies on the determination of PAMT and its characteristics. Further long-term studies on PAMT are warranted in the future.
Endoscopic ultrasonography (EUS) is a valuable method for differential diagnosis of submucosal tumors such as PAMT and GIST [
9]. The phenotype of tumors and the tumor cell type can be evaluated using EUS-guided fine needle aspiration and immunohistochemical analysis. PAMTs can be diagnosed if endoscopic biopsy provides sufficient specimen [
10].
The diagnosis of PAMT is based on histological features, plexiform architecture, an abundant myxoid stroma rich in small blood vessels, and immunohistochemical findings [
12]. Takahashi et al. [
2] described PAMT by designating a peculiar histology (plexiform growth pattern, a myxoid stroma rich in small vessels) and cell nature (myofibroblastic origin). The histological characteristics of PAMT are a multinodular plexiform growth pattern, bland-looking spindle cells, and an Alcian blue-positive myxoid stromal matrix rich in small vessels. On immunohistochemistry, the tumor cells of PAMT are positive for SMA and negative for c-kit, CD34, S-100 protein, epithelial membrane antigen (EMA), and desmin [
4]. SMA is useful for the diagnosis of leiomyosarcoma. A strong and diffuse c-kit expression is considered a key diagnostic feature of GISTs. CD34 is normally expressed in endothelial cells, embryonic cells of the hematopoietic system, and solitary fibrous tumors; however, it is not usually expressed in leiomyomas or desmoid-type fibromatoses. The S100 protein expression in spindle cell neoplasms of the GI tract is a characteristic of schwannomas. Desmin is a sensitive marker for myogenic differentiation, and it is also expressed in desmoid-type fibromatosis. These antibodies are useful in combination for differential diagnosis of spindle cell tumors in the GI tract.
The pathological differential diagnosis of PAMT includes specific types of GIST (myxoid and succinate dehydrogenase-deficient, which lacks mutations in c-kit and platelet-derived growth factor receptor alpha [PDGFRA] genes), inflammatory fibroid polyp, leiomyoma, neurofibroma, schwannoma, extracardiac myxoma, desmoid-type fibromatosis, and low-grade fibromyxoid sarcoma [
48]. For the diagnosis of PAMT, the tumor cells should be positive for SMA and caldesmon, and negative for at least CD34, S-100, EMA, and c-kit. GISTs do not show the distinctive plexiform intramural growth pattern and are typically positive for CD117 or DOG1. Leiomyoma is detected by the fascicular arrangement of tumor cells with spindle-shaped nuclei and an eosinophilic cytoplasm, and is diffusely positive for SMA, desmin, and H-caldesmon. Plexiform neurofibroma is positive for S-100 protein, and myxoid leiomyoma is positive for SMA, desmin, and caldesmon. Solitary fibrous tumors consist of altered hypercellular and hypocellular areas, deposits of dense keloid-type collagen, and hemangiopericytoma-like areas, and are positive for CD34. Inflammatory fibroid polyp shows epithelioid to spindled fibroblasts and inflammatory cells.
The majority of patients with gastric PAMT undergo resection for accurate pathologic diagnosis and treatment. Surgeons prefer minimally invasive laparoscopic approaches and decide the surgical extent (wedge resection or partial gastrectomy) according to the location and size of the tumors. Several physicians have reported endoscopic treatment for gastric PAMT [
410]. Considering the benign features of this tumor, observation without resection may be suggested; our report, in addition to the already existing reports on PAMT, will help to better understand the pathologic features and prognosis of this condition for future studies.
In conclusion, a gastric PAMT is an extremely rare benign mesenchymal tumor, and its definitive diagnosis is difficult. Although this tumor has distinct histological and immunohistochemical features, awareness is important for its diagnosis. Gastric PAMT should, thus, be considered in the differential diagnosis of gastric benign tumors.