Abstract
Purpose
This study aimed to identify time-dependent prognostic factors and demonstrate the time-dependent effects of important prognostic factors in patients with advanced gastric cancer (AGC).
Materials and Methods
We retrospectively evaluated 3,653 patients with AGC who underwent curative standard gastrectomy between 1991 and 2005 at the Korea Cancer Center Hospital. Multivariate survival analysis with Cox proportional hazards regression was used in the analysis. A non-proportionality test based on the Schoenfeld residuals (also known as partial residuals) was performed, and scaled Schoenfeld residuals were plotted over time for each covariate.
Results
The multivariate analysis revealed that sex, depth of invasion, metastatic lymph node (LN) ratio, tumor size, and chemotherapy were time-dependent covariates violating the proportional hazards assumption. The prognostic effects (i.e., log of hazard ratio [LHR]) of the time-dependent covariates changed over time during follow-up, and the effects generally diminished with low slope (e.g., depth of invasion and tumor size), with gentle slope (e.g., metastatic LN ratio), or with steep slope (e.g., chemotherapy). Meanwhile, the LHR functions of some covariates (e.g., sex) crossed the zero reference line from positive (i.e., bad prognosis) to negative (i.e., good prognosis).
A comprehensive knowledge of the prognosis of patients with cancer is highly important in the development of a treatment strategy and management plan. The TNM classification of malignant tumors based only on the anatomical extent of the disease is a simple and practical staging system for predicting prognosis in patients with cancer.1 In contrast, multivariate survival studies can distinguish more independent prognostic factros among the many tumor-, host-, environment-, and treatmentrelated factors, and thus can provide a more accurate and detailed analysis of the prognosis of cancer patients.2
The Cox proportional hazards (PH) regression model has been most widely used in multivariate survival analyses in cancer studies.3 The Cox model examines the relationship between a potential prognostic factor and survival time distribution while assuming the proportionality of the hazards. This implies that the measured relative hazard ratio of each potential prognostic factor is constant over the entire observation time. However, whether the PH assumption remains valid over a long period of time is controversial. If some variables violate the PH assumption, a multivariate study using the Cox model may provide inaccurate or distorted analytical results.45 As a result, some significant prognostic factors could be missed and the relative hazard ratio of a time-dependent prognostic factor might be overestimated or underestimated at some point over the entire observation time.
In several studies of long-term survival in breast cancer patients, the time-dependent effects of hormone receptor status, tumor size, histologic grade, and other prognostic factors have been demonstrated.67 For example, the hormone receptor status of breast cancer showed a dramatic time-dependent effect on the prognosis. Negative hormone receptor status had an adverse effect on prognosis in the early period but demonstrated a protective effect in the late period. On the other hand, the effects of the other time-dependent prognostic factors have been found to decrease or disappear over time.8 Therefore, prognostic factors violating the PH assumption should not be regarded as extraordinary cases or special phenomena limited to breast cancer studies.
The pathological variables of depth of invasion, lymph node metastasis, tumor size, gross type, histological type, and lymphovascular invasion have been well established as significant prognostic factors after curative resection in patients with gastric cancer.191011 More recently, the prognostic effects of adjuvant chemotherapy, the extent of lymph node dissection, postoperative complications, and biomarkers have been discovered.12131415 However, at present, little is known about the time-dependent effects of prognostic factors in advanced gastric cancer (AGC).16 Therefore, the aim of the current study was to identify time-dependent prognostic factors and demonstrate the time-dependent effects of important prognostic factors in patients with AGC.
We retrospectively evaluated patients with AGC who underwent curative gastrectomy between 1991 and 2005 at the Department of Surgery, Korea Cancer Center Hospital, Seoul, Republic of Korea.17 The exclusion criteria included early gastric cancer (T1), distant metastasis (M1), residual tumor (R1 or R2), remnant gastric cancer, and previous or concurrent malignancies at the time of surgery. Finally included for analysis were a total of 3,653 patients among 6,918 patients who underwent surgery for gastric cancer during the study period.
All of the patients had received distal or total gastrectomy. Adjuvant chemotherapy was considered for patients with pathological stage II or III disease (sixth edition of the American Joint Committee on Cancer staging manual) and started generally within four weeks after surgery.18 Several chemotherapy regimens were used during the study period, including the MF regimen (mitomycin-C and 5-fluorouracil or tegafur plus uracil), the FAM regimen (5-fluorouracil, adriamycin, and mitomycin-C), the FP regimen (5-fluorouracil and cisplatin), oral 5-fluorouracil alone, and oral tegafur plus uracil alone.1219 The patients were examined regularly every three months for the initial two years after surgery, then every six months for three years, and then yearly thereafter. Routine follow-up examinations included physical examinations, tumor marker studies, chest radiographs, abdominal pelvic computed tomography, upper gastrointestinal series, and gastroscopy. The overall survival time after surgery was determined based on data from the institutional database or from the National Statistical Office for patients who were lost to follow-up. The median follow-up time was 39.9 months (range, 0.0 to 168.0 months) at the time of data analysis.
The tumor-related variables examined were depth of invasion, rate of lymph node metastasis, distant metastasis, tumor size, gross type, longitudinal location, circular location, World Health Organization (WHO) histological type, Lauren classification, Ming classification, lymphatic invasion, and venous invasion. The host- and treatment-related variables examined were sex, age, surgical type, postoperative complications, and adjuvant chemotherapy. All of the variables except gross type were converted into binary variables in order to evaluate the prognostic significance of each variable in a more similar condition and to demonstrate the time-dependent effect of prognostic factors more clearly.20
Four categories of depth of invasion, namely muscularis propria (MP, T2), subserosa (SS, T3) group, serosa exposure (SE, T3a), and serosa invasion (SI, T4b), were converted into two groups, namely MP/SS and SE/SI. Gross types were categorized into types 1 to 3, type 4, and type 5. The WHO histological types were also categorized into two groups. Well and moderately differentiated tubular adenocarcinomas and papillary adenocarcinoma were categorized as the differentiated type, whereas poorly differentiated tubular adenocarcinoma, signet ring cell carcinoma, and mucinous adenocarcinoma were classified as the undifferentiated type. The upper, middle, and lower longitudinal locations of the tumors were categorized as one group and compared with the general location. The lesser curvature, greater curvature, anterior, and posterior circular locations of the tumors were categorized as one group and compared with the encircling location.
The maximally selected chi-square method was used to determine the optimal cutoff points of numeric variables.21 The optimal cutoff points obtained were as follows: age of 55 years, metastatic lymph node ratio of 0.3, and tumor size of 5.7 cm. The patients were divided into two groups based on each cutoff point of the numeric variables.
Ten-year overall survival analyses were conducted for the patients who underwent curative gastrectomy for AGC. Kaplan-Meier curves and the log-rank test were used for univariate survival analysis. Cox PH regression with backward stepwise selection was used for the multivariate survival analysis.
A non-proportionality test based on the Schoenfeld residuals (also known as partial residuals) was performed to test the proportionality of all the significant prognostic factors in the multivariate survival analysis and to identify time-dependent prognostic factors in patients with AGC. The Schoenfeld residuals for all the covariates (significant prognostic factors in the multivariate survival analysis) were obtained by running a Cox PH regression model and saved as new variables in the working dataset. After deleting censored observations, a variable containing the ranked order of overall survival time was created. Then, new variables with the Schoenfeld residuals were correlated on the survival ranked order by using the Pearson correlation test. The P-value used for the non-proportionality test was the P-value used in the Pearson correlation. A P-value <0.05 indicated a violation of the proportionality assumption.
The Statistical Package for Social Sciences (SPSS) software ver. 13.0 for Windows (SPSS Inc., Chicago, IL, USA) was used. A P-value <0.05 was considered statistically significant.
Scaled Schoenfeld residuals were plotted over time for each covariate, and a dashed red line representing the null effect (null log hazard ratio) was added.7 A non-zero slope of the plot indicates a violation of the PH assumption. The plots demonstrate the log hazard ratio (beta) over time for each covariate; hence, they illustrate the time-dependence of the prognostic factors in patients with AGC. The R version 2.1 statistical package (R Fno-u dation for Statistical Computing, Vienna, Austria) was used.22
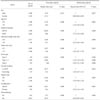
Table 1 shows 10 statistically significant factors in the AGC patients who underwent curative gastrectomy based on the results of the univariate log-rank test and Cox PH regression (estimated hazard ratio and 95% confidence intervals) from the analysis of 10-year overall survival following curative gastrectomy. Among the tumor-, host-, and treatment-related variables in patients with AGC, age, depth of invasion, metastatic lymph node ratio, tumor size, gross type, circular location, surgery type, and complications were found to have hazardous prognostic effects, with particularly intense hazards noted for patients with a high metastatic lymph node ratio and those with gross type 4 disease (Borrmann type IV) at the time of gastrectomy. On the other hand, female sex and adjuvant chemotherapy had good prognostic effects.
However, the estimated hazard ratios for each prognostic factor shown in Table 1 are valid only if the underlying PH assumption is true.23 Table 2 shows the results of the non-proportionality test based on the Schoenfeld (partial) residuals. Five variables, namely sex, depth of invasion, metastatic lymph node ratio, tumor size, and chemotherapy, showed statistical significance, indicating a violation of the PH assumption over time. Thus, time-dependent effects, which are not uncommon, have been demonstrated by the prognostic factors in the AGC patients.
For each prognostic factor, scaled Schoenfeld residuals were plotted over time. Fig. 1 is the Schoenfeld residual plot for age. The Y axis of the plot represents the beta point, that is, the log of hazard ratio, for the older patient group compared to the younger patient group. Thus, the beta (t) line (the curved solid line) with the 95% confidence interval (the two curved dotted lines) shows the log hazard ratio as a function of time in the post-gastrectomy period. Beta (t) zero (the horizontal dotted line) is equal to a hazard ratio of 1. The beta (t) line for the older patient group lies above the zero reference line and maintains parallel to the zero line during the entire study period. This plot for age is a typical example of the PH, the key assumption of the Cox model.
By contrast, the beta (t) lines of the Schoenfeld residual plots for sex, depth of invasion, metastatic lymph node ratio, tumor size, and chemotherapy cannot be maintained completely parallel to the zero line during the entire study period and represent the time-dependent effects of the prognostic factors of AGC. In Fig. 2, the beta (t) line for female sex starts above the zero line. However, it descends and crosses the zero line by around 10 months and then remains beneath the zero line for a long period. The plot for sex suggests that female sex has a good prognostic effect on survival overall. However, it shows an adverse effect in the early post-gastrectomy period. In Fig. 3, 4, 5, the beta (t) lines for depth of invasion, metastatic lymph node ratio, and tumor size start at high beta points but decline gradually over time. The beta (t) line for depth of invasion meets and crosses the zero line in the late period, while the beta (t) line for metastatic lymph node ratio remains at the high beta point until the late period. In Fig. 6, the beta (t) line for adjuvant chemotherapy begins at the negative 1.5 beta point and approaches the zero line at aroun4d0 months without crossing the zero line, which suggests that the protective effect of adjuvant chemotherapy on survival is very strong in the early period but rapidly diminishes within three or four years.
The time-dependent effects of the prognostic factors of AGC are clearly demonstrated in this study. Host-related factors maintain their prognostic effects over time. Although female sex shows a hazardous effect in the early period, which was influenced by the very poor prognosis of the young women with AGC, it has a protective effect on overall survival.11 Tumor-related factors such as depth of invasion, metastatic lymph node ratio, and tumor size show significant time-dependent effects and usually lose their hazardous prognostic effects over time. It is interesting that metastatic lymph node ratio shows a time-dependent effect, decreasing its hazardous effect over time. However, it maintains a substantial hazardous effect until the late period.7 Adjuvant chemotherapy, a treatment-related factor, also shows a time-dependent effect, and its protective effect was minimized within a couple of years but sustained for a long time.
In our results, five of the 10 independent factors in the Cox PH regression analysis showed time-dependent effects. Thus, we can suggest that time-dependent effects are not an uncommon phenomenon among prognostic factors of AGC and that the PH assumption of Cox regression could easily be violated in a long-term study. The plots of scaled Schoenfeld residuals for the time-dependent prognostic factors intuitively show the change in the log hazard ratio over time, and provide detailed and practical information on the prognosis of patients with a certain prognostic factor. For example, the unfavorable prognostic effect of a high metastatic lymph node ratio can last for 10 years or longer after curative gastrectomy in patients with AGC, indicating that all routine follow-up examinations should be undertaken for a long period by patients with a high metastatic lymph node ratio. On the other hand, some routine examinations such as abdominal pelvic computed tomography can be discontinued after several years in patients with other tumor-related unfavorable factors.
In the 15-year follow-up results of the randomized nationwide Dutch D1D2 trial, D2 lymphadenectomy showed a dramatic time-dependent effect on the survival of gastric cancer patients treated with curative gastrectomy.13 The D2 procedure was also associated with significantly higher postoperative mortality, morbidity, and reoperation rates. After a median follow-up of 15 years, D2 lymphadenectomy was associated with lower locoregional recurrence and gastric cancer-related death rates than the D1 procedure. Thus, the D2 procedure had an adverse effect on survival in the early period but showed a protectiveef - fect in the late period. The time-dependent effect in the Dutch D1D2 trial also accords with the long-lasting hazard of lymph node metastasis demonstrated in this study.
In several studies of long-term survival of breast cancer patients, the time-dependent effects of tumor-related prognostic factors were determined.67 Hormone receptor status showed a remarkable time-dependent effect on prognosis. Negative hormone receptor status was an adverse prognostic factor in the early period but became a protective prognostic factor in the late period. However, the other tumor-related prognostic factors such as tumor size and histologic grade simply weakened or lost their prognostic effects over time.8 Therefore, a time-dependent prognostic factor showing time-dependent effects should not be regarded as an extraordinary case or a special phenomenon limited to breast cancer studies. As a result, some significant prognostic factors could be missed in multivariate studies using the Cox PH regression model, and the relative hazard ratio of time-dependent prognostic factors may be overestimated or underestimated at some point in the entire observation period.7
In the Cox PH model, the hazard ratio is generally averaged over the event times, and the same weight is given to a very early hazard ratio that affects almost all individuals and to a very late hazard ratio that affects only very few individuals still at risk.7 Although Cox PH has been widely used for survival analysis in medicine,3 time-dependent effects have been assessed in only a few oncology publications, such as in breast or colon cancer studies.782425 In gastric cancer, Berger et al.26 reported time-related variations in gastric cancer prognosis in a study of Cox modeling based on fractional polynomials.
Several methods can be used for testing non-proportionality. Statistical tests for time-dependent effects have different powers to detect non-proportionality. Tests requiring partitioning of the failure time have been shown to have less power than other tests. By contrast, tests based on time-dependent covariates or on the Schoenfeld residuals have equally good power to detect non-proportionality in various non-PH and are practically equivalent.27 Schoenfeld residuals are calculated and reported at every failure time under the PH assumption and as such are not defined for censored subjects.2829 A smooth plot of the Schoenfeld residuals can then be used to directly visualize the log hazard ratio.29 Graphically, this method is reliable and easy to interpret.
The results of the current study suggest that the time-dependent effects of the prognostic factors of AGC are demonstrated in this study and are not an uncommon phenomenon among prognostic factors of AGC.
Figures and Tables
 | Fig. 3A scaled Schoenfeld residual plot for depth of invasion. PH = proportional hazard; SE = serosa exposure; SI = serosa invasion; MP = muscularis propria; SS = subserosa group. |
References
1. Sobin LH, Gospodarowicz MK, Wittekind C, editors. TNM classification of malignant tumours. New York: John Wiley & Sons;2011.
2. Gospodarowicz M, O'Sullivan B. Prognostic factors in cancer. Semin Surg Oncol. 2003; 21:13–18.
3. Cox DR. Regression models and life-tables. J R Stat Soc Series B Stat Methodol. 1972; 34:187–220.
4. Bradburn MJ, Clark TG, Love SB, Altman DG. Survival analysis part II: multivariate data analysis: an introduction to concepts and methods. Br J Cancer. 2003; 89:431–436.
5. Ahmed FE, Vos PW, Holbert D. Modeling survival in colon cancer: a methodological review. Mol Cancer. 2007; 6:15.
6. Hilsenbeck SG, Ravdin PM, de Moor CA, Chamness GC, Osborne CK, Clark GM. Time-dependence of hazard ratios for prognostic factors in primary breast cancer. In : Gasparini G, editor. Prognostic variables in node-negative and node-positive breast cancer. Boston, MA: Springer;1998. p. 317–327.
7. Bellera CA, MacGrogan G, Debled M, de Lara CT, Brouste V, Mathoulin-Pélissier S. Variables with time-varying effects and the Cox model: some statistical concepts illustrated with a prognostic factor study in breast cancer. BMC Med Res Methodol. 2010; 10:20.
8. Warwick J, Tabàr L, Vitak B, Duffy SW. Time-dependent effects on survival in breast carcinoma: results of 20 years of follow-up from the Swedish two-county study. Cancer. 2004; 100:1331–1336.
9. Kattan MW, Karpeh MS, Mazumdar M, Brennan MF. Postoperative nomogram for disease-specific survival after an R0 resection for gastric carcinoma. J Clin Oncol. 2003; 21:3647–3650.
10. Eom BW, Ryu KW, Nam BH, Park Y, Lee HJ, Kim MC, et al. Survival nomogram for curatively resected Korean gastric cancer patients: multicenter retrospective analysis with external validation. PLoS One. 2015; 10:e0119671.
11. Park JI, Jin SH, Bang HY, Paik NS, Moon NM, Lee JI. Survival rates after operation for gastric cancer: fifteen-year experience at a Korea Cancer Center Hospital. J Korean Gastric Cancer Assoc. 2008; 8:9–19.
12. Sakuramoto S, Sasako M, Yamaguchi T, Kinoshita T, Fujii M, Nashimoto A, et al. ACTS-GC Group. Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med. 2007; 357:1810–1820.
13. Songun I, Putter H, Kranenbarg EM, Sasako M, van de Velde CJ. Surgical treatment of gastric cancer: 15-year follow-up results of the randomised nationwide Dutch D1D2 trial. Lancet Oncol. 2010; 11:439–449.
14. Tsujimoto H, Ichikura T, Ono S, Sugasawa H, Hiraki S, Sakamoto N, et al. Impact of postoperative infection on long-term survival after potentially curative resection for gastric cancer. Ann Surg Oncol. 2009; 16:311–318.
15. Pietrantonio F, De Braud F, Da Prat V, Perrone F, Pierotti MA, Gariboldi M, et al. A review on biomarkers for prediction of treatment outcome in gastric cancer. Anticancer Res. 2013; 33:1257–1266.
16. Takeuchi H, Kakeji Y, Maehara Y. Time-dependent relevance of prognostic factors in patients with gastric cancer. Hepatogastroenterology. 2008; 55:779–781.
17. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 2nd English Edition. Gastric Cancer. 1998; 1:10–24.
18. Sobin LH, Wittekind C, editors. TNM Classification of Malignant Tumors. 6th ed. New York: Wiley-Liss;2002.
19. Hermans J, Bonenkamp JJ, Boon MC, Bunt AM, Ohyama S, Sasako M, et al. Adjuvant therapy after curative resection for gastric cancer: meta-analysis of randomized trials. J Clin Oncol. 1993; 11:1441–1447.
20. Harrell FE Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996; 15:361–387.
21. Miller R, Siegmund D. Maximally selected chi square statistics. Biometrics. 1982; 38:1011–1016.
22. R Development CORE TEAM. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing;2010.
23. Platt RW, Joseph KS, Ananth CV, Grondines J, Abrahamowicz M, Kramer MS. A proportional hazards model with timedependent covariates and time-varying effects for analysis of fetal and infant death. Am J Epidemiol. 2004; 160:199–206.
24. Gilchrist KW, Gray R, Fowble B, Tormey DC, Taylor SG 4th. Tumor necrosis is a prognostic predictor for early recurrence and death in lymph node-positive breast cancer: a 10-year follow-up study of 728 Eastern Cooperative Oncology Group patients. J Clin Oncol. 1993; 11:1929–1935.
25. Bolard P, Quantin C, Esteve J, Faivre J, Abrahamowicz M. Modelling time-dependent hazard ratios in relative survival: application to colon cancer. J Clin Epidemiol. 2001; 54:986–996.
26. Berger U, Schäfer J, Ulm K. Dynamic Cox modelling based on fractional polynomials: time-variations in gastric cancer prognosis. Stat Med. 2003; 22:1163–1180.
27. Ng'andu NH. An empirical comparison of statistical tests for assessing the proportional hazards assumption of Cox's model. Stat Med. 1997; 16:611–626.
28. Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994; 81:515–526.
29. Schoenfeld D. Chi-squared goodness-of-fit tests for the proportional hazards regression model. Biometrika. 1980; 67:145–153.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download