Abstract
Purpose
The Lauren classification system is a very commonly used pathological classification system of gastric adenocarcinoma. A recent study proposed that the Lauren classification should be modified to include the anatomical location of the tumor. The resulting three types were found to differ significantly in terms of genomic expression profiles. This retrospective cohort study aimed to evaluate the clinical significance of the modified Lauren classification (MLC).
Materials and Methods
A total of 677 consecutive patients who underwent curative gastrectomy from January 2005 to December 2007 for histologically confirmed gastric cancer were included. The patients were divided according to the MLC into proximal non-diffuse (PND), diffuse (D), and distal non-diffuse (DND) type. The groups were compared in terms of clinical features and overall survival. Multivariate analysis served to assess the association between MLC and prognosis.
Results
Of the 677 patients, 48, 358, and 271 had PND, D, and DND, respectively. Their 5-year overall survival rates were 77.1%, 77.7%, and 90.4%. Compared to D and PND, DND was associated with significantly better overall survival (both P<0.01). Multivariate analysis showed that age, differentiation, lympho-vascular invasion, T and N stage, but not MLC, were independent prognostic factors for overall survival. Multivariate analysis of early gastric cancer patients showed that MLC was an independent prognostic factor for overall survival (odds ratio, 5.946; 95% confidence intervals, 1.524~23.197; P=0.010).
Gastric cancer is the fourth most common cancer in the world and one of the most prevalent cancers in East Asian countries like Korea and Japan.1 Although the mortality and incidence of gastric cancer has decreased, the prognosis of patients with gastric cancer remains poor and our understanding of this cancer is still limited.2 There are numerous systems that aim to classify gastric cancer according to pathological findings. One of these is the Lauren classification system. Although it dates back to 1965, it is still one of the most commonly used pathological classification systems of gastric adenocarcinoma. This system classifies gastric adenocarcinoma into the intestinal, diffuse, or mixed types on the basis of histology. Each type has a distinct pathology, epidemiology, and prognosis.3 At the epidemiological level, the intestinal type, particularly that in the antrum, associates strongly with chronic inflammation.45 Conversely, inflammation is absent in the diffuse type.6 At the clinical level, the diffuse type appears to have a different pattern of spread and behavior than the intestinal type.7 The anatomical location of gastric cancer also influences prognosis; a recent study showed that gastric cancers in the cardia or proximal-third gastric cancer are associated with a worse prognosis than middle- or distal-third gastric cancers.8 However, at present, these histopathological, anatomic, and epidemiological distinctions are not taken into account in the clinical management of gastric cancer.
Shah et al.9 recently hypothesized that the Lauren classification system should be modified to include both the Lauren pathological classification and the anatomical location of gastric cancer, thus yielding at least three entirely distinct types termed the proximal non-diffuse type (PND), Lauren's diffuse type (D), and distal non-diffuse type (DND). Their molecular biological analyses then showed that there were marked differences between these three types in terms of mRNA expression profiles.
In the present retrospective cohort study, we aimed to evaluate the clinical significance of this modified Lauren classification (MLC) system. The specific aims of our study were to compare the clinicopathological characteristics of Korean patients with resectable gastric adenocarcinoma who were divided according to the MLC system and to assess the prognostic value of MLC in gastric adenocarcinoma.
All consecutive patients who underwent curative gastrectomy between January 2005 and December 2007 for histologically confirmed gastric cancer in Seoul National University Bundang Hospital in Seongnam, South Korea were included in this retrospective analysis. The curative gastrectomy was performed by two experienced surgeons who used the laparoscopic or open method. All patients underwent D1+ or D2 lymphatic dissection in accordance with the Japanese Gastric Cancer Association guidelines.10 None of the patients had residual tumor at either the macroscopic or microscopic level after surgery. Date regarding the characteristics of the patients, tumor, and treatment were collected from our electronic medical records.
This study was approved by the institutional review board of the Seoul National University Bundang Hospital (IRB No. B-1502/286-112).
PND tumors were those whose bulk (>80%) was located in the gastric cardia. These tumors extended up to the gastroesophageal junction and a small portion of the distal esophagus. They had Lauren intestinal type histopathology. The D tumors could be located anywhere in the stomach but had Lauren diffuse and mixed type histopathology. DND tumors were those whose bulk was usually in the distal stomach, although they could extend up to the mid body of the stomach or down to the pylorus. They had Lauren intestinal type histopathology. The patients were classified according to the tumor location and Lauren classification based on the final pathological report.
All statistical analyses were performed by PASW ver. 18.0 (IBM Co., Armonk, NY, USA) software. P-values <0.05 were considered to be statistically significant. The overall survival period was defined as the time from the diagnosis of cancer to death or the last out-patient department visit day. The disease free survival period was defined as the time from diagnosis of cancer to the identified date of recurrence. The MLC patient groups were compared in terms of clinical characteristics by chi-squared test. The survival curves of the three groups were generated by Kaplan-Meier analysis and were compared by using the log-rank test. Univariate analyses were performed by Kaplan-Meier analysis with log-rank test, and multivariate analyses were performed with the variables that were significant on univariate analysis and by using the Cox proportional hazard model.
In total, 677 patients were eligible to enroll in our study. Their median age was 58.3 years (range, 26~89 years), there were 460 males and 217 females, and the median follow-up period was 55.64 months (range, 0~101 months). There were 48 patients in the PND group, 358 patients in the D group, and 271 patients in the DND group (Table 1). The male:female ratios within each group were 41:7, 204:154, and 215:56, respectively. The D group had a significantly higher proportion of females than the other two groups (both P<0.001). The mean age of the PND, D, and DND groups was 62.4±9.6, 55.1±13.1, and 61.9±9.4 years. The D group patients were significantly younger than the patients in the other groups (both P<0.001). The mean body mass indices of the PND, D, and DND groups did not differ significantly (23.8±3.3, 23.2±3.1, and 24.0±3.0 kg/m2, respectively).
Of the 677 patients, 541 patients (79.9%) underwent subtotal gastrectomy and 136 (20.1%) underwent total gastrectomy. The PND patients were significantly more likely to undergo total gastrectomy (27/48, 56.3%) than the D (99/358, 27.7%) or DND (14/271, 5.2%) patients (both P<0.01). The D patients were also significantly more likely to undergo total gastrectomy than the DND patients (P<0.01). The three groups did not differ significantly in terms of other surgical factors (Table 1).
In the PND, D, and DND groups, the mean tumor size was 3.6±2.2, 5.1±3.2, and 3.1±2.0 cm, respectively. The D group had a significantly larger tumor size on average than the other two groups (both P<0.01) and more positive lymph-vascular invasion than DND group (P<0.01). The DND group showed a pathologically differentiated pattern compared to PND and D groups (both P<0.01). Of the PND, D, and DND groups, 31.3% (15/48), 52.0% (186/358), and 24.4% (66/271) had positive lymph nodes and the mean number of positive lymph nodes was 2.7±6.0, 5.5±10.3, and 1.7±5.1, respectively. The D group had significantly more positive lymph nodes than the DND group (P<0.01). Moreover, 35.4% (17/48), 56.4% (202/358), and 29.9% (81/271) of the PND, D, and DND patients had advanced gastric cancer, respectively. Moreover, the D group was significantly more likely to have advanced T-stage and N-stage cancer than the other two groups (all P<0.01) (Table 2).
The follow-up durations of the PND, D, and DND groups were 52.8±19.0, 53.7±18.3, and 58.5±12.2 months, respectively (Table 1). The DND group had a significantly longer follow-up duration than the other two groups (P<0.01). The disease-free survival rates of the PND, D, and DND groups were 89.6%, 83.0%, and 93.0%, respectively. DND was associated with a more favorable 5-year disease-free survival rate than D (P<0.01), but did not differ significantly from PND (P=0.36). The PND and D groups did not differ significantly in terms of 5-year disease-free survival rate (P=0.28). The 5-year overall survival rates of the PND, D, and DND groups were 77.1%, 77.7%, and 90.4%, respectively. DND was associated with more favorable overall survival compared to D and PND groups (both P<0.01) (Fig. 1). The PND and D groups did not differ significantly in terms of 5-year overall survival (P=0.89).
Univariate analysis showed that the following variables were associated with improved overall survival: younger age (<60 years, P=0.001), smaller tumor size (<3 cm, P<0.001), the use of subtotal gastrectomy as opposed to total gastrectomy (P<0.001), distal location (P<0.001), differentiated pathologic classification (P=0.001), no lymphatic invasion (P<0.001), no vascular invasion (P<0.001), T1 stage (P<0.001), N0 stage (P<0.001), intestinal Lauren classification type (P<0.001), and DND MLC type (P<0.001) (Table 3). Multivariate analysis with these variables revealed that a younger age, no vascular invasion, T1 stage, and N0 stage were the only independent prognostic factors for better overall survival (Table 4).
To further assess the clinical relevance of MLC, the patients in the cohort who had early gastric cancer (EGC) were identified.
In this cohort, the 5-year overall survival rates of the PND, D, and DND groups were 90.3%, 96.2%, and 97.4%, respectively. DND was associated with more favorable overall survival compared
to PND (P=0.047). However, the D and DND groups did not differ significantly in terms of 5-year overall survival rates (P=0.14), and the 5-years survival rates of the PND group and D group were not significantly different (P=0.54) (Fig. 2). Of the seven variables that were included in the multivariate analysis, MLC (odds ratio, 5.946; 95% confidence intervals, 1.524~23.197; P=0.010) and age (odds ratio, 4.340; 95% confidence intervals, 1.144~16.466; P=0.031) were the only independent prognostic factors for 5-year overall survival rates. Specifically, DND and younger age (<60 years) were predictors for improved 5-year overall survival rates (Table 5).
The present study on the clinical relevance of the MLC system revealed that patients with PND, D, and DND type gastric cancer differed markedly in terms of clinical and surgical characteristics. Moreover, in univariate analysis, DND type associated with a significantly better 5-year overall survival, although this was not observed on multivariate analysis. However, in EGC cases, DND was associated significantly with a better 5-year overall survival compared to the other MLC types on multivariate analysis.
In 1965, Lauren proposed a pathological classification of gastric cancer that became one of the most commonly used classification systems for gastric adenocarcinoma worldwide. Studies of the Lauren classification system show that the diffuse and intestinal Lauren types account for approximately 85% of gastric carcinomas. The intestinal type is more frequently seen in men and older patients, while the D type occurs more frequently in women and younger patients.1112131415 The diffuse type also associated with more advanced pT and pN stages and has a worse prognosis than the intestinal type; this was also observed in a Chinese study.16 Similarly, in our study, we found that compared to patients with intestinal Lauren type gastric cancer, patients with the diffuse Lauren type were more likely to be female, younger, and to have advanced pT and pN stage disease. Thus, our analysis showed that the diffuse and intestinal Lauren types in a Korean population were similar to these types in other populations in terms of clinicopathological characteristics.111213 However, we failed to find that the diffuse type was associated independently with poor prognosis in multivariate analysis. Similarly, a recent study from Germany that reported similar clinicopathological profiles for the diffuse and intestinal Lauren types showed that Lauren classification was only associated significantly with prognosis in univariate analysis; this association was no longer detected on multivariate analysis.17 This may reflect the fact that the diffuse Lauren type is associated with more advanced pT and pN stage disease, which may have contributed to the association of diffuse Lauren type with poor prognosis in univariate analysis. Thus, Lauren type is not an independent prognostic factor in gastric adenocarcinoma.
Shah et al.9 proposed that gastric adenocarcinoma is a heterogeneous disease with subtypes that differ in terms of epidemiology and histopathology. This is supported by other studies that showed that the anatomical location of gastric cancer has clinical relevance: gastric cardia or proximal-third gastric adenocarcinoma is associated with a worse prognosis than middle- or distal-third gastric cancer.181920 As a result, Shah et al.9 hypothesized that a modification of the Lauren classification that takes into account the anatomical location of the tumor may be even more useful than the existing Lauren classification. The proposed MLC system allows gastric adenocarcinoma to be classified into three types, namely, PND, D, and DND.21 Shah et al.9 then showed that these types differed significantly in their gene expression profiles. Our study showed that these three types also varied in terms of their clinical characteristics; compared to patients with PND or DND type gastric cancer, patients with D type gastric cancer were more likely to be female, younger, to have higher numbers of positive lymph nodes, and to have ≥T1 and N+ stage cancer. The patients with PND type gastric cancer were more likely to undergo total gastrectomy than the patients with DND or D. Finally, DND was associated with a favorable 5-year overall survival rate compared to PND and D in univariate, but not multivariate, analysis
Closer analysis of the 5-year overall survival rates showed that the PND group had a poor prognosis compared to the DND group, but a similar 5-year overall survival rate compared to the D group. However, the PND group did not differ from the DND group in terms of pT and pN stages. This is consistent with the findings of Shah et al.9 However, in our multivariate analysis, age and pT and pN stages, but not MLC, were associated with 5-year overall survival. Further studies assessing the clinical relevance of MLC in gastric cancer are warranted.
The implementation of nationwide screening programs with endoscopy in Japan and Korea has led to a recent surge in the detection of EGC. As a result, EGC currently accounts for approximately 50% of all curative gastrectomies that are performed for gastric cancer in Korea.222324 This led us to assess whether MLC influences the prognosis of the EGC patients in our cohort. Additionally, multivariate analysis within this subgroup revealed that MLC and age <60 years are independent prognostic factors in these patients. Specifically, DND was associated with a more favorable prognosis than the other two types. Pathologic differentiation, lymphatic invasion and venous invasion were not prognostic factors in this multivariate analysis. The EGC group consisted of T1a and T1b tumors. This may make overall survival in the EGC group dependent on depth of tumor. Furthermore, patients with positive lymph nodes accounted for only 14.1% of the EGC group. These results may increase the effect of the MLC on overall survival only in the EGC group. This multivariate analysis result suggests that patients with PND or D type disease should be carefully treated and required short-term follow up, even at an early stage of disease.
This study has some limitations. First, it is a retrospective study from a single center. However, the fact that it is a single center study has some advantages; our institute follows the Japanese Gastric Cancer treatment guidelines,10 which means that all patients were treated with the same surgical method. Moreover, all procedures were performed by the same two experienced surgeons. This may have reduced the impact of surgeon experience and surgical method on survival. Second, the sample size of the PND group was rather small, especially in the EGC subgroup analysis. This reflects the fact that EGC has a good prognosis and thus patients with such early stage disease are less willing than patients with advanced gastric cancer to continue having regular checkups after curative resection. As a result, many patients with EGC are lost to follow-up. Further studies with multiple centers that enroll more patients are needed to confirm our results.
In conclusion, DND type gastric cancer was associated with a favorable 5-year overall survival rate compared to PND and D type disease. MLC was an independent prognostic factor in multivariate analysis of patients with EGC, although this was not observed in the multivariate analysis of the entire cohort. Further studies on the clinical relevance of MLC in EGC are needed.
Figures and Tables
Fig. 1
Five-year overall survival rates of patients with different modified Lauren classification types of gastric cancer. PND = proximal non-diffuse modified Lauren type; D = diffuse modified Lauren type; DND = distal non-diffuse modified Lauren type.
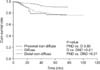
Fig. 2
Five-year overall survival rates of patients with different modified Lauren classification types of early gastric cancer. PND = proximal non-diffuse modified Lauren type; D = diffuse modified Lauren type; DND = distal non-diffuse modified Lauren type.

Table 2
Pathological comparison of modified Lauren classification

Values are presented as mean±standard deviation, number (%), or number only. PND = proximal non-diffuse modified Lauren type; D = diffuse modified Lauren type; DND = distal non-diffuse modified Lauren type; LN = lymph node. *Classification according to the standard of American Joint Committee on Cancer 7th edition of the staging system.
References
1. Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol. 2006; 24:2137–2150.
2. Moore MA, Eser S, Igisinov N, Igisinov S, Mohagheghi MA, Mousavi-Jarrahi A, et al. Cancer epidemiology and control in North-Western and Central Asia: past, present and future. Asian Pac J Cancer Prev. 2010; 11:Suppl 2. 17–32.
3. Lauren P. The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand. 1965; 64:31–49.
4. You WC, Blot WJ, Li JY, Chang YS, Jin ML, Kneller R, et al. Precancerous gastric lesions in a population at high risk of stomach cancer. Cancer Res. 1993; 53:1317–1321.
5. Correa P, Haenszel W, Cuello C, Zavala D, Fontham E, Zarama G, et al. Gastric precancerous process in a high risk population: cross-sectional studies. Cancer Res. 1990; 50:4731–4736.
6. Carneiro F, Huntsman DG, Smyrk TC, Owen DA, Seruca R, Pharoah P, et al. Model of the early development of diffuse gastric cancer in E-cadherin mutation carriers and its implications for patient screening. J Pathol. 2004; 203:681–687.
7. Marrelli D, Roviello F, de Manzoni G, Morgagni P, Di Leo A, Saragoni L, et al. Italian Research Group for Gastric Cancer. Different patterns of recurrence in gastric cancer depending on Lauren's histological type: longitudinal study. World J Surg. 2002; 26:1160–1165.
8. Sakaguchi T, Watanabe A, Sawada H, Yamada Y, Tatsumi M, Fujimoto H, et al. Characteristics and clinical outcome of proximal-third gastric cancer. J Am Coll Surg. 1998; 187:352–357.
9. Shah MA, Khanin R, Tang L, Janjigian YY, Klimstra DS, Gerdes H, et al. Molecular classification of gastric cancer: a new paradigm. Clin Cancer Res. 2011; 17:2693–2701.
10. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011; 14:113–123.
11. Muñoz N, Correa P, Cuello C, Duque E. Histologic types of gastric carcinoma in high- and low-risk areas. Int J Cancer. 1968; 3:809–818.
12. Stalsberg H. Histological typing of gastric carcinoma. A comparison of surgical and autopsy materials, and of primary tumours and metastases. Acta Pathol Microbiol Scand A. 1972; 80:509–514.
13. Kim KH, Chi CH, Lee SK, Lee D, Kubo T. Histologic types of gastric carcinoma among Koreans. Cancer. 1972; 29:1261–1263.
14. Stemmermann GN, Brown C. A survival study of intestinal and diffuse types of gastric carcinoma. Cancer. 1974; 33:1190–1195.
15. Correa P, Cuello C, Duque E. Carcinoma and intestinal metaplasia of the stomach in Colombian migrants. J Natl Cancer Inst. 1970; 44:297–306.
16. Qiu MZ, Cai MY, Zhang DS, Wang ZQ, Wang DS, Li YH, et al. Clinicopathological characteristics and prognostic analysis of Lauren classification in gastric adenocarcinoma in China. J Transl Med. 2013; 11:58.
17. Dittmar Y, Rauchfuss F, Dondorf F, Ardelt M, Scheuerlein H, Settmacher U. Extended pathohistological criteria for assessment of the long-term prognosis of gastric cancer. Zentralbl Chir. 2015; DOI: 10.1055/s-0034-1383080. [In print].
18. Kajiyama Y, Tsurumaru M, Udagawa H, Tsutsumi K, Kinoshita Y, Ueno M, et al. Prognostic factors in adenocarcinoma of the gastric cardia: pathologic stage analysis and multivariate regression analysis. J Clin Oncol. 1997; 15:2015–2021.
19. Hansson LE, Sparén P, Nyrén O. Increasing incidence of carcinoma of the gastric cardia in Sweden from 1970 to 1985. Br J Surg. 1993; 80:374–377.
20. Ohno S, Tomisaki S, Oiwa H, Sakaguchi Y, Ichiyoshi Y, Maehara Y, et al. Clinicopathologic characteristics and outcome of adenocarcinoma of the human gastric cardia in comparison with carcinoma of other regions of the stomach. J Am Coll Surg. 1995; 180:577–582.
21. Shah MA, Kelsen DP. Gastric cancer: a primer on the epidemiology and biology of the disease and an overview of the medical management of advanced disease. J Natl Compr Canc Netw. 2010; 8:437–447.
22. Kim JW, Hwang I, Kim MJ, Jang SJ. Clinicopathological characteristics and predictive markers of early gastric cancer with recurrence. J Korean Med Sci. 2009; 24:1158–1164.
23. Jeong O, Park YK. Clinicopathological features and surgical treatment of gastric cancer in South Korea: the results of 2009 nationwide survey on surgically treated gastric cancer patients. J Gastric Cancer. 2011; 11:69–77.
24. Park JM, Kim YH. Current approaches to gastric cancer in Korea. Gastrointest Cancer Res. 2008; 2:137–144.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download