Abstract
Gastric volvulus is an uncommon clinical entity. There are three types of gastric volvulus; organoaxial, mesenteroaxial and combined type. This condition can lead to a closed-loop obstruction or strangulation. Traditional surgical therapy for gastric volvulus is based on an open approach. Here we report a successful case of a patient with chronic gastric volvulus with a laparoscopic treatment. A 79-year-old woman came to the emergency department with epigastric pain accompanied by nausea for 2 weeks. Abdominal computed tomography revealed markedly distended stomach with transposition of gastroesophageal Junction and gastric antrum. Barium meal study revealed presence of the antrum was folded over 180 degrees that was located above gastroesophageal junction. We attempted an endoscopic reduction, but it was unsuccessful. The patient got laparoscopic anterior gastropexy. Based on our result, laparoscopic gastropexy can be considered as a good choice of the treatment for gastric volvulus.
Gastric volvulus was first described by Berti in 1866 based on the autopsy of a 61-year-old woman.1 There are three types of gastric volvulus: organoaxial (most common), where abnormal torsion occurs on a stomach's longitudinal axis (line connecting the cardia and the pylorus along the luminal axis of stomach); mesenteroaxial, where torsion occurs along a vertical axis (from lesser curvature to greater curvature); and a combination both the above types.2
The incidence is rare, approximately 20% of gastric volvulus cases occur in infants under 1 year old, and the other 80% in adults, among which 80% to 90% cases occur in the fifth decade of life.3 There is no reported association with sex or race. The symptoms of gastric volvulus vary depending on the degree of twisting and the rapidity of onset. Rotation of the stomach more than 180° causes complete gastric outlet obstruction. A closed loop can cause strangulation of the stomach, which can lead to ischemia, necrosis, perforation, and abdominal sepsis.
We report a case of a 79-year-old woman with chronic gastric volvulus treated with endoscopic decompression and laparoscopic gastropexy.
A 79-year-old woman reported to the emergency center with a history of recurrent epigastric pain and nausea for 2 weeks. She had no underlying diseases other than hypertension. However, she had visited the emergency room previously with recurrent epigastric pain and nausea. There was no history of trauma. When reviewed, she denied any of the following: diaphoresis, shortness of breath, constipation, diarrhea, previous surgery, and use of non-steroidal anti-inflammatory drugs and alcohols. On physical examination, her vital signs were stable. Abdominal examination revealed upper abdominal distension without rebound tenderness or signs of peritoneal irritation. Normoactive bowel sounds were noted. Laboratory testing revealed a moderately elevated white cell count of 14,500/ml with 91% segmented neutrophils.
A plain abdominal radiograph revealed a large air bubble sign in the left upper abdomen (Fig. 1A). A contrast-enhanced abdominal computed tomography revealed a markedly distended stomach; the transposition of the gastroesophageal junction and gastric antrum confirmed a recurrent or chronic state of mesenteroaxial gastric volvulus (Fig. 1B). A barium meal study revealed the presence of the antrum folded over 180° located above gastroesophageal junction (single study). After the patient consumed a foaming agent for a double study, the gastric antrum and gastroesophageal junction returned to their normal position, the gastric antrum returning to its position above the gastroesophageal junction within 2 to 3 minutes. There was no duodenal passage disturbance (Fig. 2A).
After insertion of an endoscope and gentle air insufflations on entering into the gastric lumen of the endoscope shaft, abnormal rotation of the gastric axis was observed. While removing the previously inserted endoscope, the axis recovered to the normal direction (Fig. 2B). After endoscopic reduction, the patient felt an improvement in her symptoms for about 24 hours. However, the symptoms recurred after that, due to which surgical treatment was planned.
Laparoscopic surgery was performed under general anesthesia. The surgeon stood on the right side of the patient. The umbilical port for the camera was prepared with the open technique. Pneumoperitoneum was created with carbon dioxide and intracorporeal pressure was maintained at 12 mmHg. Three 5-mm trocars were placed.
There was no proof of a hiatal hernia. The spleen had no redundancy, but the 1st and 2nd duodenal portions showed redundancy. Reduction of the gastric volvulus was performed with two laparoscopic graspers through traction of the greater curvature of the stomach. The greater curvature of the stomach was sutured to the abdominal wall by using laparoscopic suture techniques. The stomach was lifted up to the abdominal wall to check the optimal point of the gastropexy. Four prolene 2-0 sutures were placed along the greater curvature of the stomach from 5 cm above the pylorus to the lower body. The gap between sutures was about 3 cm. Four 3-mm skin incisions were made with a no. 11 blade to insert an endo-closure to bring out the prolene suture (Fig. 3A). The pneumoperitoneum was slightly released to 5 mmHg, and the prolene sutures were tied and firmly held in their positions without any excessive traction (Fig. 3B).
On postoperative day 5, an upper gastointestinal study confirmed reduction of the patient's stomach (Fig. 4). The patient did well in the postoperative period and was discharged at postoperative day 7. She was followed up for 6 months and showed no evidence of recurrence, either radiological or symptomatic.
Gastric volvulus is defined as an abnormal rotation of the stomach of more than 180°, creating a closed-loop obstruction and resulting in incarceration and strangulation.4 Congenital diaphragmatic hernia, paraesophageal hernia, and wandering spleen are the main secondary causes of this condition.4 More commonly, secondary volvulus occurs due to diaphragmatic defects or other intraabdominal factors such as left diaphragmatic eventration, adhesions, gastric ulceration, and gastric or duodenal carcinoma.5 In our case, there was no predisposing factor accompanying gastric volvulus, which is very rare. Chronic gastric volvulus is typically characterized by intermittent epigastric pain and abdominal fullness after meals.6 The Borchardt triad (severe epigastric pain and distention, vomiting followed by violent retching without the ability to vomit, and difficulty or inability to pass a nasogastric tube) is the key diagnostic feature of acute volvulus which occurs in 70% of cases.7
The basic surgical dictum for the treatment of gastric volvulus includes decompression of the stomach with reduction of the volvulus, gastropexy, and correction of the intra-abdominal factors predisposing to volvulus.5 Tanner8 described the various methods of surgical repair for gastric volvulus. These include gastrojejunostomy, fundo-antral gastrogastrostomy (Opolzer's operation), partial gastrectomy, division of bands, repair of diaphragmatic hernia, simple gastropexy, gastropexy with division of the gastrocolic omentum (Tanner's operation), and repair of eventration of the diaphragm.
Endoscopic gastropexy with a gastrostomy tube can be used to decrease the incidence of recurrent volvulus. However, Eckhause and Ferron9 reported that a solitary percutaneous endoscopic gastrostomy (PEG) tube can create a new point of fixation for the recurrent volvulus. Laparoscopic and endoscopic techniques can be combined in acute cases. Koger and Stone10 reported an acute organoaxial gastric volvulus with paraesophageal hernia treated with laparoscopic reduction followed by broad gastropexy using three pull-type PEG tubes. Naim et al.11 reviewed previously reported laparoscopic interventions for the treatment of gastric volvulus. They concluded that the laparoscopic procedure may be the safer and less morbid approach. Laparoscopic treatment can be used in many cases, including acute and chronic situations. Gastric volvulus with large paraesophageal hernias can be managed laparoscopically as well.12
In conclusion, after endoscopic maneuvering to reduce acute symptoms, laparoscopic gastropexy represents a safe and feasible approach to treating gastric volvulus. Evaluation of the optimal point of the gastropexy is very important during surgery. Elderly patients may have potential benefits such as minimal morbidity and shorter hospital stay after undergoing laparoscopic gastropexy. Long-term studies are needed to document whether laparoscopic gastropexy alone would be a gold standard for treating chronic gastric volvulus without hiatal hernia.
Figures and Tables
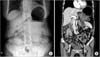 | Fig. 1(A) A simple abdominal radiograph showing a double bubble sign in the left upper abdomen. (B) A markedly distended stomach with transposition of the gastroesophageal junction and gastric antrum. |
 | Fig. 2(A) An upper gastrointestinal study revealed the presence of mesenteroaxial gastric volvulus with the finding that the antrum was located above the gastroesophageal junction (red arrow). (B) Gastroscopic finding: abnormal rotation of the axis can be seen. EG = esophagogastric. |
References
1. Berti A. Singolare attorcigliamento dell'esofago col duodeno sequito da rapida morte. Gazz Med Ital. 1866; 9:139–141.
2. Wasselle JA, Norman J. Acute gastric volvulus: pathogenesis, diagnosis, and treatment. Am J Gastroenterol. 1993; 88:1780–1784.
3. Cardile AP, Heppner DS. Gastric volvulus, Borchardt's triad, and endoscopy: a rare twist. Hawaii Med J. 2011; 70:80–82.
4. Morelli U, Bravetti M, Ronca P, Cirocchi R, De Sol A, Spizzirri A, et al. Laparoscopic anterior gastropexy for chronic recurrent gastric volvulus: a case report. J Med Case Rep. 2008; 2:244.
5. Channer LT, Squires GT, Price PD. Laparoscopic repair of gastric volvulus. JSLS. 2000; 4:225–230.
6. Palanivelu C, Rangarajan M, Shetty AR, Senthilkumar R. Laparoscopic suture gastropexy for gastric volvulus: a report of 14 cases. Surg Endosc. 2007; 21:863–866.
7. Kuwano H, Hashizume M, Ohta M, Sumiyoshi K, Sugimachi K, Haraguchi Y. Laparoscopic repair of a paraesophageal hiatal hernia with gastric volvulus. Hepatogastroenterology. 1998; 45:303–306.
8. Tanner NC. Chronic and recurrent volvulus of the stomach with late results of "colonic displacement". Am J Surg. 1968; 115:505–515.
9. Eckhauser ML, Ferron JP. The use of dual percutaneous endoscopic gastrostomy (DPEG) in the management of chronic intermittent gastric volvulus. Gastrointest Endosc. 1985; 31:340–342.
10. Koger KE, Stone JM. Laparoscopic reduction of acute gastric volvulus. Am Surg. 1993; 59:325–328.
11. Naim HJ, Smith R, Gorecki PJ. Emergent laparoscopic reduction of acute gastric volvulus with anterior gastropexy. Surg Laparosc Endosc Percutan Tech. 2003; 13:389–391.
12. Jeong SH, Ha CY, Lee YJ, Choi SK, Hong SC, Jung EJ, et al. Acute gastric volvulus treated with laparoscopic reduction and percutaneous endoscopic gastrostomy. J Korean Surg Soc. 2013; 85:47–50.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download