Abstract
The surgical indications for the treatment of gastroesophageal reflux disease (GERD) in patients with esophageal motility disorders have been debated. We report a case of antireflux surgery performed in a patient with absent esophageal motility as categorized by the Chicago classification (2011). A 54-year-old man underwent laparoscopic Toupet fundoplication due to apparent GERD and desire to discontinue all medications. After surgery, his subjective symptoms improved. Furthermore, objective findings including manometry and 24-hour pH-metry also improved. In our experience, antireflux surgery can improve GERD symptoms patients, even with absent esophageal motility.
Gastroesophageal reflux disease (GERD) affects 10% to 20% of the Western population and 4.3% to 15.7% of patients in Eastern Asia.1 Proton pump inhibitors (PPIs) are the preferred medical treatment for GERD. However, a considerable proportion of patients experience recurrence of symptoms despite of optimal medical treatment. Thus, antireflux surgery could be an alternative treatment option for long-term therapy.
The Nissen fundoplication appeared to be the more successful procedure for reflux control in several studies, and has been adopted in general practice. However, dysphagia was frequently observed after the Nissen procedure. Hence, patients who could be possible to have a risk of dysphagia when underwent antireflux surgery among patients with motility disorder, a partial wrap was recommended in this situation.
In Korea, antireflux surgery has not been widely adopted as a treatment for GERD and there are few reports on this operation compared to reports from Western countries, where the procedure is frequently used.23
Here we report a case of successful laparoscopic partial fundoplication in a patient lacking esophageal motility.
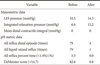
A 54-year-old man with a 10-year history of GERD and both typical and atypical symptoms was referred to the surgical clinic for antireflux surgery because of his desire to stop medications. His typical symptoms were epigastric soreness and regurgitation, while atypical symptoms included a globus sensation. He had been successfully treated with PPIs for 10 years. The patient underwent several studies to investigate the cause of his symptoms. A barium swallow study showed retention of contrast flow at the distal esophagus with minimal esophageal dilatation. It also demonstrated decreased peristaltic movement in the entire esophagus (Fig. 1). In addition, esophagogastroduodenoscopy (EGD) revealed that the gastric cardia did not tightly surround a retroflexed endoscope (Fig. 2A). Esophageal high resolution manometry (HRM) showed absent peristalsis of the distal esophagus (Fig. 3) with decreased basal lower esophageal sphincter (LES) pressure (10.5 mmHg) and zero of mean distal contractile integral (DCI). However, integrated relaxation pressure (IRP) was within normal levels of 6.6 mmHg (Table 1). Next, 24-hour impedance pH monitoring showed that all reflux distal episode, symptom index, and the DeMeester score were 79, 50%, and 82.6, respectively. We also observed an all reflux percent time of 5.3% (Table 1). Based on these findings, the final diagnosis according to the 2011 revised Chicago classification criteria was PPI-responsive GERD without dysphagia and absent peristalsis, and with low resting pressure. Therefore, surgeons and gastroenterologists planned a laparoscopic Toupet (posterior 270°) fundoplication to avoid postoperative dysphagia.
Under general anesthesia, the patient was placed in a supine position, and the surgeon stood on the right side of the patient. Pneumoperitoneum was induced and maintained at 12 mmHg using a Veress needle. Four trocars (two 10 mm and two 5 mm) were inserted. Using the reverse Trendelenburg position, the procedure started by dividing short gastric vessels from the low pole of the spleen to the angle of His. The procedure continued to the lesser omentum high enough to not cut the vagal branch to the liver. After identification of the anterior vagal nerve, the gastrophrenic ligament was divided. The dissection was then continued from right to left behind the esophagus until the crura was exposed and the angle of His was detached. At this point, a posterior window was created large enough to easily wrap using umbilical tape. After ensuring sufficient wrap placement, cruroplasty was accomplished with three simple intracorporeal nonabsorbable sutures using 3-0 Ethibond. The 2-cm-long partial Toupet wrap was completed using the anterior wall of the gastric fundus. After the leading edge of the fundus was pulled posteriorly, the fundus was sutured to the right side of the esophagus over a length of 2 cm. The anterior fundus was sutured to the left side of the esophagus over the same spacing length with 90° distance between both wraps. The right side of the wrap was anchored to the hiatus to prevent intrathoracic migration of the wrap. After confirming hemostasis and the absence of other immediate complications, the operation was completed (Fig. 4).
The patient recovered uneventfully and was able to tolerate a regular diet. The patient was discharged on postoperative day 4. His medication (PPIs and motility drugs) were stopped after surgery. When present, he controlled his symptoms with medications on demand and he was able to completely stop all medications 6 months postoperatively.
After 6 months, the patient was subjected to EGD, 24-hour impedance pH monitoring, and esophageal HRM. EGD demonstrated absence of hiatal relaxation on the retroflexed view (Fig. 2B). Esophageal HRM still showed absent peristalsis of the distal esophagus. Mean DCI after operation was also remained at zero. However, LES pressure increased from 10.5 to 14.3 mmHg and IRP also increased from 6.6 to 12.2 mmHg (Table 1). The 24-hour pH monitoring revealed increased esophageal acidity during the resting period. All reflux distal episode was observed less frequently (4 times compared to 79 times). All reflux percent times normalized to 0.0% from 5.3% and the DeMeester score reduced to 0.8 from 82.6 (Table 1, Fig. 5). Manometric and pH-metric differences before and after surgery are summarized in Table 1. At 14 months after the operation, the typical symptoms were improved compared to those prior to surgery and the patient remained off all medications. He felt symptoms only 3 or 4 times per week. He did not report dysphagia and had no difficulties with belching but did occasionally complain of mild symptoms of bloating and flatulence.
The incidence of GERD is increasing and is now about twice that of 10 years ago. GERD has recently been recognized as a significant health concern in Korea and PPI medication use is also increasing. 4 GERD was defined as 'a condition which develops when the reflux of stomach contents causes troublesome symptoms and/or complications' by the Montreal consensus. A diagnosis of GERD can be confirmed by abnormal endoscopic findings such as a mucosal break at the gastroesophageal junction, Barrett's esophagus on biopsy, a peptic stricture in the absence of malignancy, or positive findings on 24-hour pH monitoring. The treatment of GERD is based on medical therapy including PPIs. However, surgery is indicated in patients who have failed medical management, opt for surgery despite successful medical management, have complications of GERD or extra-esophageal manifestations defined by the Society of American Gastrointestinal and Endoscopic Surgeons guideline. The LOTUS trial5 demonstrated similar results at 5 year outcomes using drug-induced acid suppression with esomeprazole or antireflux surgery. Korean expert consensus declared antireflux surgery is especially useful for patients who require long-term use of PPIs or who have refractory GERD in updated 2012 guidelines for the treatment of GERD.6
Laparoscopic Nissen (total 360°) fundoplication is the preferred surgical procedure among several options. Although antireflux surgery induces excellent symptom control, it may be associated with some adverse effects including dysphagia, bloating, and flatulence. For this reason, modified procedures such as Rosetti-Nissen (the procedure of Nissen without ligation of the short gastric vessels) or Toupet (a partial posterior 270° wrap) have been developed to address these adverse effects. Partial fundoplication is associated with less postoperative dysphagia, fewer reoperations, similar patient satisfaction, and similar effectiveness for controlling GERD compared with total fundoplication. Specifically, a total fundoplication appears particularly unwarranted in cases of esophageal motility disorder from a viewpoint of the tailored approach. With this knowledge, we decided to perform partial fundoplication in our case to diminish the possibility of postoperative dysphagia.
The surgical indications for cases of GERD with associated esophageal motility disorders are debated. In the guidelines for the treatment of GERD, it is strongly recommended that all patients should undergo preoperative manometry to rule out achalasia or scleroderma-like esophagus.7
However, there is a great deal of evidences indicates that severely disordered esophageal peristalsis does not impact the outcome of antireflux surgery.
Munitiz et al.8 reported that significant increases in contractile wave pressure and a decrease in the percentage of non-propagated waves were found in dysmotility patients after fundoplication. Herbella et al.9 observed a significant increase in the amplitude of peristalsis in patients with abnormal peristalsis that had undergone partial or total fundoplication. They also observed normalization of peristalsis in 31% of patients who underwent partial fundoplication and 86% of patients who underwent total fundoplication.
Novitsky et al.10 stated that a 360° fundoplication should not be contraindicated for patients with severe esophageal dysmotility because effective fundoplication improved esophageal motility for most patients in their multicenter retrospective review. In addition, partial fundoplication is not as reliable or durable as total fundoplication. The authors defined severe dysmotility as manometry findings showing an esophageal amplitude of 30 mmHg or less and/or 70% or more nonperistaltic esophageal body contractions. By this definition, the patient in the present report had severe dysmotility. Novitsky et al.10 concluded that GERD patients with dysmotility can undergo a well-constructed total fundoplication without risk of dysphagia since multiple reports showed that elimination of acid exposure improves esophageal motility and esophageal clearance. The authors also explain that esophageal dysmotility is a known sequela of chronic esophageal acid exposure rather than a preexisting condition.
Our patient still has GERD symptoms 3 to 4 times a week at 6 months after surgery. In general, symptomatic diagnosis of GERD is usually made when the patient has symptoms occurring more than 2 times a week. Therefore, it can be said that our patient still has GERD after surgery, even though the detected pH returned to normal. Moreover, regarding the fact that the this patient's esophageal motility did not improve after surgery, a total wrap might be more beneficial for this patient.
In Korea, anti-reflux surgery has not been widely adopted as a treatment for GERD and there are few reports on this operation compared to reports from Western countries, where the procedure is frequently used. To our knowledge, there have been only two reports involving 46 patients treated with antireflux surgery in Korea.23 All patients received Nissen fundoplication after preoperative manometry, but no postoperative manometry was reported.
Here, we report symptom control and increased LES pressure after laparoscopic Toupet fundoplication in a GERD patient with absent peristalsis.
Figures and Tables
 | Fig. 1Preoperative barium swallow showing retention of contrast flow at the distal esophagus with esophageal dilatation. |
 | Fig. 2(A) Preoperative endoscopic findings reveal that the gastric cardia is not tightly surrounding a retroflexed endoscope. (B) Postoperative endoscopic findings reveal lack of hiatal relaxation in the retroflexion view. |
References
1. Jung HK. Epidemiology of gastroesophageal reflux disease in Asia: a systematic review. J Neurogastroenterol Motil. 2011; 17:14–27.
2. Lee SB, Jeon KM, Kim BS, Kim KC, Jung HY, Choi YB. Early experiences of minimally invasive surgery to treat gastroesophageal reflux disease. J Korean Surg Soc. 2013; 84:330–337.
3. Lee SK, Kim EK. Laparoscopic Nissen fundoplication in Korean patients with gastroesophageal reflux disease. Yonsei Med J. 2009; 50:89–94.
4. Kim KM, Cho YK, Bae SJ, Kim DS, Shim KN, Kim JH, et al. Prevalence of gastroesophageal reflux disease in Korea and associated health-care utilization: a national population-based study. J Gastroenterol Hepatol. 2012; 27:741–745.
5. Galmiche JP, Hatlebakk J, Attwood S, Ell C, Fiocca R, Eklund S, et al. LOTUS Trial Collaborators. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. JAMA. 2011; 305:1969–1977.
6. Jung HK, Hong SJ, Jo YJ, Jeon SW, Cho YK, Lee KJ, et al. Korean Society of Neurogastroenterology and Motility. Updated guidelines 2012 for gastroesophageal reflux disease. Korean J Gastroenterol. 2012; 60:195–218.
7. Katz PO, Gerson LB, Vela MF. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2013; 108:308–328. quiz 329
8. Munitiz V, Ortiz A, Martinez de Haro LF, Molina J, Parrilla P. Ineffective oesophageal motility does not affect the clinical outcome of open Nissen fundoplication. Br J Surg. 2004; 91:1010–1014.
9. Herbella FA, Tedesco P, Nipomnick I, Fisichella PM, Patti MG. Effect of partial and total laparoscopic fundoplication on esophageal body motility. Surg Endosc. 2007; 21:285–288.
10. Novitsky YW, Wong J, Kercher KW, Litwin DE, Swanstrom LL, Heniford BT. Severely disordered esophageal peristalsis is not a contraindication to laparoscopic Nissen fundoplication. Surg Endosc. 2007; 21:950–954.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download