Abstract
Purpose
Although several clinical trials have proven the efficacy of adjuvant S-1 treatment in gastric cancers, it is still unclear which patients receive the most benefit. In this study, we prospectively recruited patients with locally advanced gastric cancer who had undergone curative resection followed by adjuvant S-1 administration to investigate which factors affect the outcomes.
Materials and Methods
Between July 2010 and October 2011, we enrolled 49 patients who underwent curative resection for stage II or III gastric cancer and who subsequently received adjuvant S-1 treatment for 1 year.
Results
Twenty-nine patients (59.2%) continued S-1 treatment for 1 year, and 12 patients (24.5%) experienced recurrent disease during the follow-up period. Patients with continuation of S-1 for 1 year had significantly increased rates of disease-free survival (P<0.001) and overall survival (P=0.001) relative to the patients who discontinued S-1 during year 1. Multivariate analysis indicated poor outcomes for patients with stage III disease and those who discontinued S-1 treatment. Excluding patients who discontinued S-1 due to cancer progression (n=7), adjuvant treatment with S-1 still demonstrated a significant difference in the disease-free survival rate between the patients who continued treatment and those who discontinued it (P=0.020).
Gastric cancer is one of the most common malignancies and the third leading cause of cancer-related mortality worldwide.1 Resection of the stomach and proper dissection of the lymph nodes are the only management options that have been shown to improve the survival of gastric cancer patients.2 However, the majority of patients with locally advanced gastric cancer often present with recurrent disease after surgery. As a result, several studies have attempted to demonstrate the survival benefit of perioperative treatments to increase the rate of curative resection and to reduce the rate of recurrence after surgery. Prior to the last decade, most of the adjuvant treatment strategies have been investigated in Western countries such as the USA and the UK.345 The variability of surgical quality for extended lymphadenectomy in these clinical trials has been pointed out.6 Novel clinical trials should be conducted for Eastern patients who have undergone a standard D2 lymphadenectomy for locally advanced gastric cancer to examine the proper role of adjuvant treatment in this patient population. Previously, two representative multi-institutional studies in Asian populations have reported a survival benefit with adjuvant chemotherapy following curative D2 lymphadenectomy.78 However, despite undergoing adjuvant treatment for 6 months to 1 year after surgery, approximately one-fourth of patients in the chemotherapy group demonstrated recurrence in both studies.78 In order to examine a potential improvement in survival for gastric cancer patients, it is necessary to identify a subgroup of patients who are expected to show a poor response to adjuvant treatments.
S-1 (previously known as TS-1) is an oral formulation of 5-fluorouracil (5-FU) consisting of 1-(2-tetrahydrofuryl)-5-fluorouracil (tegafur), 5-chloro-2,4-dihydroxypyridine, and potassium oxonate (Oxo) in a molar ratio of 1.0:0.4:1.0.9 The aim of the Adjuvant Chemotherapy Trial of TS-1 for Gastric Cancer (ACTS-GC) was to evaluate the efficacy of TS-1 in relation to long-term survival compared with surgery alone in stage II or III gastric cancer.8 The aim of the CLASSIC study was to evaluate the effect on longterm survival of adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy. Given that neither partial nor total gastrectomy was found to affect the pharmacokinetics of 5-FU derived from S-1, its use appears to be suitable in the postoperative adjuvant setting for advanced stage gastric cancer patients. Despite that fact, in the ACTS-GC study, 34.2% of patients treated with S-1 withdrew from treatment and 27.8% showed recurrence after treatment with S-1.8
To date, several reports have described how to modify the schedule of adjuvant S-1 in order to maintain a full year of treatment, as well as to predict patient compliance with S-1 treatment. 101112 Aoyama et al.13 reported that the level of creatinine clearance was a significant risk factor for the continued use of S-1 adjuvant treatment. To our knowledge, there is no previous report that clarifies whether the continued use of S-1 has an effect on patient prognosis. Moreover, there are a few reports that describe the safety and feasibility of adjuvant S-1 chemotherapy in a Korean population.14 Therefore, further investigation of adjuvant S-1 treatment for gastric cancer in Korean patients is warranted. Here, we report the results of a prospective single center study in a Korean population in order to demonstrate the compliance with S-1 adjuvant treatment after standard gastric cancer surgery and to elucidate the correlation between continuation of S-1 and the survival rates of gastric cancer patients with stage II and III disease.
This study was a prospective observational study of a single center in Korea. Three surgeons with a collective experience of over 200 cases of gastric cancer surgery performed all surgical procedures and administered all adjuvant chemotherapy regimens. Forty-nine patients who underwent curative resection including D2 lymphadenectomy for gastric cancer were enrolled in this study. All patients were diagnosed with stage II or III gastric adenocarcinoma according to the American Joint Committee on Cancer Staging Manual 7th edition. Patients with evidence of metastatic disease were excluded from the study. Other criteria for enrollment included lack of any other existing malignancy, no history of previous chemoradiotherapy, and a performance status score of 0 to 2 on the Eastern Cooperative Oncology Group scale. The study protocol was approved by the Institutional Review Board of Ajou University Hospital (MED-OBS-10-138).
S-1 was administered according to the schedule suggested in the ACTS-GC study. Patients were enrolled within 6 weeks after surgery and confirmation of final pathology and performance status. Patients recruited into this study received S-1 at a dose of 40 mg (body surface area [BSA] <1.25 m2), 50 mg (BSA 1.25~1.50 m2), or 60 mg (BSA >1.50 m2) twice daily for 4 weeks, then rested during the following 2 weeks. The period of adjuvant S-1 treatment was 1 year, and we observed patients until death or until 5 years after surgery. Dose reductions or interruptions were allowed at the physician's discretion when patients experienced potentially serious or life-threatening adverse events including poor general health, myelosuppression, or gastrointestinal symptoms. For example, if patients had hematologic toxic effects of grade 3 or grade 4 or non-hematologic toxic effects of grade 2, grade 3, or grade 4, their daily dose was reduced, from 120 to 100 mg, 100 to 80 mg, or 80 to 50 mg. If patients could not complete TS-1 during the first postoperative year for various reasons, they were simply observed without any other treatment. However, if patients were diagnosed with recurrence, we recommended that they receive secondary chemotherapeutic regimens.
Adverse events were assessed according to the Common Terminology Criteria for Adverse Events of the National Cancer Institute (NCI-CTCAE). These events were documented while patients were receiving chemotherapy and for 28 days after the last dose of study medication. Patients underwent hematologic tests and assessments of clinical symptoms every 2 weeks. The presence of a relapse was determined by means of imaging studies, including ultrasonography, computed tomography (CT), and endoscopy. Patients underwent at least one type of imaging study, usually CT, at 3 or 6 month intervals during the first 2 years after surgery and at 6 month intervals thereafter until year 5 after surgery.
The primary endpoint was overall survival, defined as the time from date of surgery to date of death from any cause. The secondary endpoint was 5-year disease-free survival, defined as the time from date of surgery to date of recurrence of the original gastric cancer, development of a new gastric cancer, or death from any cause.
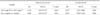
A total of 49 patients were enrolled between July 2010 and October 2011. The median age was 56 years, and patient age ranged from 32 to 79 years. Twenty-nine patients (59.2%) were men and 20 patients (40.8%) were women. Eight patients (16.3%) received total gastrectomy, 41 patients (83.7%) underwent subtotal gastrectomy, and 2 patients (4.1%) received combined resection (splenectomy and distal pancreatectomy) due to tumor invasion into the spleen or lymph node metastasis to the splenic hilum. The primary tumors of 2 patients (4.1%) involved the whole stomach, 6 tumors (12.2%) were located in the upper third, 22 tumors (44.9%) in the middle, and 19 (38.8%) in the lower third of the stomach. Of the 49 patients evaluated, 20 (40.8%) were finally diagnosed with stage II, and 29 (59.2%) were diagnosed with stage III (Table 1).
The median time until the initiation of the adjuvant chemotherapy after surgery was 31.9 days (range: 16~52 days).
Data regarding adverse events on the 49 patients who received adjuvant S-1 were prospectively collected for analysis. Adverse events of grade 1, 2, 3, or 4 were defined according to the NCICTCAE, including, gastrointestinal, hematologic, neurologic, and dermatologic symptoms.15 Grade 3 and 4 toxicities occurred in 1.9% and 5.7% of patients, respectively. Common side effects are outlined in Table 2 and included grade 3 and 4 diarrhea, oral ulcers, and skin rash.
Twenty-nine patients completed S-1 dosing and 20 patients discontinued S-1 treatment. Twenty patients (40.8%) completed the 1-year schedule with full-dose administration and 9 patients required dose reduction. The causes of incomplete S-1 dosing are outlined in Table 3 and include disease progression (n=7), side effects (n=9), and others (n=4).
During the follow-up period, recurrent disease was diagnosed in 12 patients (24.5%). The most common types of recurrence were spread to distant lymph nodes and hematogenous spread to the liver. Ultimately, 7 patients died due to cancer recurrence (Table 4).
We analyzed the correlation between various clinicopathologic factors and oncologic outcomes. In the univariate analysis, stage III disease and non-completion of S-1 treatment were significantly correlated with worse disease-free survival and overall survival rates, and the differentiation of the primary tumor was related to the overall survival rate (Table 5, 6). In the multivariate analysis, stage III disease and non-completion of S-1 were factors that predicted early recurrence (stage III: relative risk [RR] 0.155, P=0.018; non-completion: RR 0.068, P=0.001) and a poor overall survival rate (stage III: RR 0.107, P=0.036; non-completion: RR 0.054, P=0.006) (Table 7).
Additionally, we analyzed the disease-free or overall survival rates of 42 patients after the exclusion of 7 patients who received incomplete S-1 treatment due to recurrence, in order to remove bias. Of the 42 patients, 13 patients with non-completion of S-1 still demonstrated a worsening of the disease-free survival rate when compared to patients with completion of S-1 treatment (Fig. 1).
Our study demonstrates that 1 year of adjuvant S-1 treatment after gastric cancer surgery in a Korean patient population with stage II and III gastric cancer disease is well tolerated. In addition, our study emphasizes that non-continuation of adjuvant S-1 treatment during the 1-year period after surgery is significantly associated with a high risk of recurrence and poor survival of patients with stage II and III gastric cancer.
Postoperative oral administration of S-1 has become the best option for patients with stage II and III gastric cancer based on the reported survival benefit in recent multicenter randomized controlled clinical trials.816 Prior to these results, the only proven evidence for adjuvant treatment in gastric cancer came from the results of the Medical Research Council Adjuvant Gastric Infusional Chemotherapy (MAGIC) trial and the Intergroup 0116 (INT-0116) trial, both conducted in Western countries.35 In these Western studies, highly toxic intravenous agents or radiation in the perioperative period resulted in higher survival rates compared to surgery alone. However, most surgeons in Eastern countries such as Korea and Japan have not tended to base their practices on those results because of the differences in procedures for D2 lymphadenectomy. There were no standard surgical procedures in those reported clinical trials. However, surgeons in Eastern countries typically perform D2 lymphadenectomy and most believe that the procedure would be sufficient to cure patients with stage I gastric cancers. Meanwhile, there was also a consensus among these physicians that additional treatment modalities were needed to improve the survival rate for patients with more advanced disease even after curative gastrectomy with D2 lymphadenectomy. In particular, as patients treated with gastrectomy generally have a poor tolerance for chemotherapeutic agents, compliance with adjuvant treatment should be considered. From this point of view, orally available S-1 treatment is very suitable for patients who have undergone partial or total gastrectomy for advanced gastric cancers.
Adjuvant S-1 treatment in stage II and III gastric cancer has been approved by the National Health Insurance Corporation (NHIC) of Korea since 2011 based on the results of the ACTS-GC trial from Japan.16 This trial was the first large-scale clinical trial to show the efficacy of 5-FU in gastric cancers as adjuvant treatment. In particular, as S-1 was developed as an orally available 5-FU agent combined with other ingredients to reduce various toxicities,17 surgeons also have the ability to prescribe it without consultation with an oncologist. In our study, only surgeons performed follow-up on all enrolled patients and managed the side effects from S-1 administration. Our results showed that the percentage of patients who did not complete a full schedule of S-1 treatment was 40.8%. Although this figure was 5.7% higher than the results reported by oncologists in another Korean retrospective study,14 the difference was not statistically significant (data not shown, chi-square test, P=0.428). Of the patients enrolled in the current study, 7 ceased S-1 treatment due to cancer progression. Another 13 patients terminated S-1 treatment due to side effects (n=9) or patient refusal (n=4). In our study, 28 patients experienced one or more toxicities during their treatment, but most were properly managed, and the number of patients who stopped the medication due to toxicities could be minimized. However, our results suggested that non-completion of S-1 treatment could be an important factor to predict recurrence after surgery.
In our study, the most common side effect that resulted in a dose reduction was diarrhea (5.7%). In the ACTS-GC study, diarrhea was also one of the common side effects (grade 3 or greater, 3.1%).8 Chemotherapy-induced diarrhea also occurs in 50% to 80% of patients who are administered a chemotherapy regimen.1819 Treatment with 5-FU commonly results in diarrhea.1920 Chemotherapy-induced diarrhea can result in an imbalance of serum electrolytes, depletion of fluids, dehydration requiring hospitalization, and even chemotherapy-related death. The cause of chemotherapy-induced diarrhea involves many factors including the loss of intestinal epithelium, superficial necrosis, and inflammation of the bowel wall, which can create an imbalance between absorption and secretion in the bowel.192122 Regarding treatment with 5-FU, other clinical factors such as female sex and Caucasian ethnicity predict the severity of the chemotherapy-induced diarrhea.2324 The differences in severity are presumably influenced by the enzymatic activity of dihydropyrimidine-dehydrogenase.25 Partial deficiency of this enzyme due to polymorphisms results in decreased drug clearance and can increase toxicities. Although S-1 was developed as an oral 5-FU agent, which is expected to demonstrate lower toxicity compared to intravenous 5-FU, the potential for lower gastrointestinal toxicity would be one of the crucial side effects of 5-FU. The American Society of Clinical Oncology has suggested guidelines for the evaluation and management of patients with chemotherapyinduced diarrhea.18 Patients with uncomplicated diarrhea can be managed with medications such as loperamide in the outpatient setting, and chemotherapy should be stopped for grade 2 or greater diarrhea until symptoms resolve. However, patients with severe and complicated diarrhea (e.g., fever, sepsis, neutropenia, and bleeding) should be admitted to the hospital and treated with intravenous fluids, antibiotics, and octreotide.
Our study, along with the subgroup analysis of ACTS-GC, shows an unfavorable oncologic outcome in gastric cancer patients with stage III or worse disease in spite of adjuvant S-1 treatment after surgery.16 The long-term results of the ACTS-GC study demonstrate that adjuvant S-1 monotherapy significantly improves overall survival and the relapse-free survival rate in stage II and IIIA disease. However, in patients with stage IIIB disease, the 5-year overall survival rate was 50.2% in the patients treated with adjuvant S-1 compared to a rate of 44.1% in the surgery only group. The narrow difference between the two groups suggests that future studies should investigate the effectiveness of neoadjuvant or adjuvant treatments with multiple regimens in patients at high risk for recurrence. The previously mentioned CLASSIC trial also showed the effectiveness of oxaliplatin and capecitabine on the overall and relapse-free survival.7 The authors state that these combined regimens also showed a favorable superiority even in patients with stage III disease compared to surgery alone. However, further studies directly comparing the effectiveness of S-1 alone and these combined regimens are required. In addition, a recent randomized clinical trial (SPIRITS) demonstrated the effectiveness of S-1 plus cisplatin in patients with unresectable or recurrent gastric cancer, and other studies have shown the tolerability of these regimens in patients who have undergone gastrectomy.26 Further studies would be needed to examine whether S-1 plus cisplatin is superior to S-1 alone.
In conclusion, our results showed that completion of S-1 treatment for 1 year after surgery was the most important factor to predict the outcome of patients with advanced gastric cancer. Even when we excluded the patients who terminated S-1 treatment due to tumor recurrence from the analysis, completion of S-1 treatment was significantly related to a good outcome. Therefore, efforts are needed to control toxicities during S-1 administration, and patients should attempt to complete administration for 1 year if possible. In addition, patients with stage III disease still demonstrate poor outcomes. As a result, it is important to consider other novel regimens for patients at high risk.
Figures and Tables
Acknowledgments
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2014R1A1A2057390). Special thanks to Mr. Yoon Hwa Cho, who collected the clinicopathologic data of recruited patients in this study.
References
1. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015; 136:E359–E386.
2. Hochwald SN, Brennan MF, Klimstra DS, Kim S, Karpeh MS. Is lymphadenectomy necessary for early gastric cancer? Ann Surg Oncol. 1999; 6:664–670.
3. Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006; 355:11–20.
4. Earle CC, Maroun JA. Adjuvant chemotherapy after curative resection for gastric cancer in non-Asian patients: revisiting a meta-analysis of randomised trials. Eur J Cancer. 1999; 35:1059–1064.
5. Macdonald JS, Smalley SR, Benedetti J, Hundahl SA, Estes NC, Stemmermann GN, et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med. 2001; 345:725–730.
6. Markar SR, Wiggins T, Ni M, Steyerberg EW, Van Lanschot JJ, Sasako M, et al. Assessment of the quality of surgery within randomised controlled trials for the treatment of gastrooesophageal cancer: a systematic review. Lancet Oncol. 2015; 16:e23–e31.
7. Bang YJ, Kim YW, Yang HK, Chung HC, Park YK, Lee KH, et al. Adjuvant capecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): a phase 3 open-label, randomised controlled trial. Lancet. 2012; 379:315–321.
8. Sakuramoto S, Sasako M, Yamaguchi T, Kinoshita T, Fujii M, Nashimoto A, et al. Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med. 2007; 357:1810–1820.
9. Shirasaka T, Shimamato Y, Ohshimo H, Yamaguchi M, Kato T, Yonekura K, et al. Development of a novel form of an oral 5-fluorouracil derivative (S-1) directed to the potentiation of the tumor selective cytotoxicity of 5-fluorouracil by two biochemical modulators. Anticancer Drugs. 1996; 7:548–557.
10. Aoyama T, Yoshikawa T, Shirai J, Hayashi T, Yamada T, Tsuchida K, et al. Body weight loss after surgery is an independent risk factor for continuation of S-1 adjuvant chemotherapy for gastric cancer. Ann Surg Oncol. 2013; 20:2000–2006.
11. Iwasa S, Yamada Y, Fukagawa T, Eguchi Nakajima T, Kato K, Hamaguchi T, et al. Management of adjuvant S-1 therapy after curative resection of gastric cancer: dose reduction and treatment schedule modification. Gastric Cancer. 2011; 14:28–34.
12. Kim SJ, Kim K, Park Y, Kim BS, Huh J, Ko YH, et al. Dose modification of alemtuzumab in combination with dexamethasone, cytarabine, and cisplatin in patients with relapsed or refractory peripheral T-cell lymphoma: analysis of efficacy and toxicity. Invest New Drugs. 2012; 30:368–375.
13. Aoyama T, Yoshikawa T, Hayashi T, Kuwabara H, Mikayama Y, Ogata T, et al. Risk factors for 6-month continuation of S-1 adjuvant chemotherapy for gastric cancer. Gastric Cancer. 2013; 16:133–139.
14. Jeong JH, Ryu MH, Ryoo BY, Lee SS, Park I, Lee SH, et al. Safety and feasibility of adjuvant chemotherapy with S-1 for Korean patients with curatively resected advanced gastric cancer. Cancer Chemother Pharmacol. 2012; 70:523–529.
15. Trotti A, Colevas AD, Setser A, Rusch V, Jaques D, Budach V, et al. CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol. 2003; 13:176–181.
16. Sasako M, Sakuramoto S, Katai H, Kinoshita T, Furukawa H, Yamaguchi T, et al. Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J Clin Oncol. 2011; 29:4387–4393.
17. Kochi M, Fujii M, Kanamori N, Kaiga T, Aizaki K, Takahashi T, et al. Effect of gastrectomy on the pharmacokinetics of S-1, an oral fluoropyrimidine, in resectable gastric cancer patients. Cancer Chemother Pharmacol. 2007; 60:693–701.
18. Benson AB 3rd, Ajani JA, Catalano RB, Engelking C, Kornblau SM, Martenson JA Jr, et al. Recommended guidelines for the treatment of cancer treatment-induced diarrhea. J Clin Oncol. 2004; 22:2918–2926.
19. Gibson RJ, Stringer AM. Chemotherapy-induced diarrhoea. Curr Opin Support Palliat Care. 2009; 3:31–35.
20. Keefe DM, Gibson RJ, Hauer-Jensen M. Gastrointestinal mucositis. Semin Oncol Nurs. 2004; 20:38–47.
21. Keefe DM. Intestinal mucositis: mechanisms and management. Curr Opin Oncol. 2007; 19:323–327.
22. Keefe DM, Brealey J, Goland GJ, Cummins AG. Chemotherapy for cancer causes apoptosis that precedes hypoplasia in crypts of the small intestine in humans. Gut. 2000; 47:632–637.
23. McCollum AD, Catalano PJ, Haller DG, Mayer RJ, Macdonald JS, Benson AB 3rd, et al. Outcomes and toxicity in africanamerican and caucasian patients in a randomized adjuvant chemotherapy trial for colon cancer. J Natl Cancer Inst. 2002; 94:1160–1167.
24. Zalcberg J, Kerr D, Seymour L, Palmer M. Haematological and non-haematological toxicity after 5-fluorouracil and leucovorin in patients with advanced colorectal cancer is significantly associated with gender, increasing age and cycle number. Tomudex International Study Group. Eur J Cancer. 1998; 34:1871–1875.
25. Mattison LK, Fourie J, Hirao Y, Koga T, Desmond RA, King JR, et al. The uracil breath test in the assessment of dihydropyrimidine dehydrogenase activity: pharmacokinetic relationship between expired 13CO2 and plasma [2-13C]dihydrouracil. Clin Cancer Res. 2006; 12:549–555.
26. Koizumi W, Narahara H, Hara T, Takagane A, Akiya T, Takagi M, et al. S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol. 2008; 9:215–221.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download