Abstract
Purpose
The prevalence of gastric cancer in the elderly is increasing. The purpose of this study was to clarify factors related to morbidity following gastric cancer surgery in elderly patients.
Materials and Methods
For this study, data from 411 patients who underwent curative gastrectomies with lymph node dissections between March 2010 and January 2013 were retrospectively studied using a prospectively designed database. Patients were divided into 2 groups (<70 years vs. ≥70 years). For each group, perioperative factors were analyzed to determine if they were associated with postoperative morbidity and mortality.
Results
Comorbidities were more prevalent in the elderly group (≥70 years). Intraoperative and postoperative transfusions were also more frequently required in the elderly group. There was no significant difference in the number of retrieved lymph nodes between the 2 groups (44.3 vs. 46.6 nodes). In a comparison of the elderly versus non-elderly groups, the postoperative morbidity rates were 22.7% versus 8.9% (P<0.001) and the postoperative mortality rates were 4.2% versus 0% (P=0.002), respectively. Of the possible non-surgical complications, pulmonary problems were predominately found in the elderly group (P<0.001). Surgical complications were evenly distributed between the 2 groups (P=0.463). Postoperative morbidity was significantly associated with older age and postoperative transfusion. Multivariate analysis showed that higher body mass index (BMI) and postoperative transfusion were important factors associated with postoperative complications in the elderly group.
As the population has aged, life expectancy has increased to 77.9 years for males and 84.6 years for females in Korea.1 Although the overall incidence of gastric cancer has decreased, the incidence in the elderly is increasing. The morbidity and mortality rates after gastric cancer surgery are reportedly 43% to 46% and 10% to 13%, respectively, in Western countries.2,3 In contrast, large-scale studies in Korea have reported morbidity and mortality rates of 12.5% to 17.4% and 0.3% to 0.6%, respectively, after gastric cancer surgery.4,5
The only effective and proven method for management of patients with clinically resectable gastric cancer is curative resection of the primary tumor and proper lymph node dissection. However, this is not an easy process for elderly patients, as they commonly have various comorbidities such as hypertension, diabetes mellitus, cardiovascular disease, pulmonary disease, and cerebrovascular disease, all of which extend the postsurgery recovery period. Furthermore, studies have reported that comorbidities are significantly related to morbidity after gastric cancer surgery.6,7 Surgeons cannot avoid all postoperative complications, and these issues must be effectively managed when they occur.
The rate of postoperative complications has decreased over time due to improvements in anesthesiology, surgical instruments, operating techniques, perioperative nutritional support, and careful preoperative evaluations. The current study evaluated clinicopathological characteristics and operation risk factors related to older age and management of postoperative complications following gastric cancer surgery in elderly patients.
A total of 420 patients with gastric adenocarcinoma underwent gastric resection in the Department of Surgery at our institution between March 2010 and January 2013. Of the 420 patients, 411 patients met the following study criteria: curative resection with D1+ or ≥D2 lymph node dissection, no history of other organ malignancies, and >15 retrieved lymph nodes.
Patients with stage IV gastric cancer were excluded. Two surgeons verified the levels of the dissected lymph nodes, and pathologists examined all retrieved lymph nodes for metastasis. Subtotal or total gastrectomies were performed, and the negativity of resection margins for tumor invasion was confirmed. Laparoscopic or robotic surgery was performed for patients with gastric cancer in early clinical stages. Combined resection was considered for patients with visualized local invasion into the adjacent organs including the spleen, distal pancreas, transverse colon, or gallbladder. The extent of lymph node dissection was defined according to Japanese Research Society for Gastric Carcinoma recommendations. Cancers were staged according to the tumor-node-metastasis classification system from the Union for International Cancer Control (UICC).8 Potentially curative resection was defined as R0 resection according to the UICC residual tumor classification system. The elderly group in this study included patients who were ≥70 years of age. Postoperative morbidities were assessed by physical examinations, routine laboratory tests, and radiological examinations during hospitalization. Hospital mortality was defined as postoperative death within 30 days or death during hospitalization. Body mass index (BMI) was calculated as weight (kg) divided by height squared (m2). Patients were categorized as either non-overweight (BMI<25 kg/m2) or overweight (BMI≥25 kg/m2).
We compared clinicopathological variables and perioperative factors (operation time, time to first flatus, time to initiation of a soft diet, number of metastatic and retrieved lymph nodes, and postoperative hospital stay length), postoperative morbidities, and the hospital mortality rate for each age group.
Statistical analyses were performed using Statistical Package for the Social Sciences software, version 15.0 for Windows (SPSS Inc., Chicago, IL, USA). Clinicopathological variables were analyzed using chi-squared tests for discrete variables or Student's t-tests for continuous variables. The risk factors that influenced postoperative complications were determined using logistic regression analysis. P-values <0.05 were considered statistically significant.
The clinicopathological characteristics of the 411 patients are summarized in Table 1. The mean patient age was 61.3 years (range, 23~90 years). There were 119 patients (29.0%) in the elderly group. The 2 groups were evenly distributed and did not differ in terms of gender, BMI, tumor size, invasion depth, lymph node involvement, extent of lymph node dissection, or extent of gastrectomy. However, the elderly group had a higher prevalence of comorbidities than the non-elderly group. The most common comorbidity was hypertension (125 patients, 30.4%), followed by pulmonary diseases (20 patients, 4.9%), diabetes mellitus (19 patients, 4.6%), heart diseases (13 patients, 3.2%), and liver diseases (12 patients, 2.9%). The elderly group more frequently had tumors located in the upper third of the stomach (24.4%) compared to the non-elderly group (13.4%). Intestinal-type tumors were also more prevalent in the elderly group (63.0%) compared to the non-elderly group (54.5%). In the elderly group, combined resection and conventional operations were performed more commonly, and intraoperative and postoperative transfusions were required more frequently. Although the mean operation time was significantly shorter in the elderly group (216.3 vs. 239.6 minutes), the time to first flatus (3.5 vs. 3.2 days) and the time to initiation of a soft diet (7.2 vs. 6.7 days) were longer in the elderly group, as was the length of postoperative hospital stay. There were no significant differences between the age groups in the number of lymph nodes that were metastatic (3.6 vs. 4.0 nodes) or retrieved (44.3 vs. 46.6 nodes) (Table 2).
Postoperative complications occurred in 53 patients (12.8%) and were significantly more common in the elderly group. Hospital mortality (5/411 patients, 1.2%) only occurred in the elderly group. The 5 mortalities were attributable to sepsis due to bile peritonitis, sepsis due to intra-abdominal fluid collection with abscess, sepsis due to anastomotic leakage, myocardial infarction, and pneumonia with cerebral infarction, respectively. Non-surgical complications such as atelectasis, pneumonia, pleural effusion, or myocardial and cerebral infarction were predominantly found in the elderly group (P<0.001). Other surgical complications such as wound infection, fluid collection, intraluminal bleeding, intestinal obstruction, ileus, anastomosis leakage, duodenal stump leakage, pancreatic fistula, and hepatic complication were evenly distributed between the 2 groups (P=0.463). Four patients in the non-elderly group had stenosis of the anastomotic area, while 1 patient in the elderly group had a remnant stomach perforation (Table 3). The numbers of grade I, II, IIIa, IIIb, and V complications according to the Clavien-Dindo classification system were 11 (2.7%), 31 (7.5%), 4 (1.0%), 2 (0.5%), and 5 (1.2%), respectively.
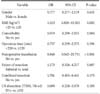
The complication rates were similar in patients with differences in gender, BMI, comorbidities, operation time, preoperative and intraoperative transfusion, extent of resection, combined resection, extent of lymph node dissection, tumor size, invasion depth, lymph node metastasis, and surgeon. Logistic regression analysis showed that postoperative morbidity was significantly associated with old age and postoperative transfusion (Table 4). High BMI and postoperative transfusion were important factors for postoperative complications in the elderly group (Table 5).
In the past, the resection rate of elderly patients with gastric cancer was very low in Europe (25%~50%) compared to Japan (56%~83%).9,10 More recently, resection rates have increased due to the widespread availability of endoscopy technology,11 which leads to earlier gastric cancer diagnosis combined with improved surgical skills, anesthesia, and postoperative intensive care.
In most countries, a person >65 years old with decreased socioeconomic function, functional loss of major organs, or decreased ability to recover from stress such as trauma is defined as 'elderly.' However, there are no clear criteria for defining this group. Elders are sometimes divided into subgroups: young-old (65~74 years), old-old (75~84 years), and oldest-old (≥85 years).12 Some papers have reported that >30% of patients with gastric cancer are >70 years old.13,14 Furthermore, a study found that pulmonary dysfunction was significantly associated with patients ≥70 years old compared to patients <70 years old.15 Therefore, we defined elderly gastric cancer patients as those >70 years old, because they accounted for approximately 30% of gastric cancer patients, which allowed us to obtain a sufficient sample size to achieve statistical significance. Moreover, raising the age criteria in the elderly group did not yield significant results due to the small sample size.
Most surgeons are reluctant to operate on elderly patients due to high morbidity and mortality rates. Improvements in surgical techniques and anesthesia have made gastrectomies safer for elderly patients with gastric cancer, but postoperative morbidity and mortality rates remain high.15,16 In this study, we also found that the postoperative morbidity rate was higher in elderly compared to non-elderly patients (22.7% vs. 8.9%). Moreover, the recovery period of elderly gastric cancer patients who underwent gastrectomies was longer in terms of bowel movement, start of soft diet, and hospital stay. However, some studies have shown no differences in postoperative outcomes between elderly and young patients.17,18,19 Furthermore, minimally invasive surgery has been widely adopted for elderly patients with gastric cancer, and it has a shorter recovery period than conventional surgery as well as similar postoperative morbidity rates as those experienced by young gastric cancer patients.20 In this study, most elderly patients had more than 1 comorbidity including hypertension (30.4%), pulmonary disease (4.9%), diabetes mellitus (4.6%), and coronary and heart disease (3.2%). Moreover, when our department first started performing laparoscopic gastrectomies for elderly patients, we had to exercise caution because the lack of an experienced laparoscopist and assistant could lead to prolonged operation times. Prolonged carbon dioxide insufflation into the intra-abdominal cavity can damage the cardiopulmonary physiology in elderly patients with comorbidities.21
Some reports have indicated that total gastrectomies and extended lymph node dissections were associated with high surgical morbidity and mortality rates in gastric cancer patients.22,23 Limited lymph node dissection is frequently performed in elderly patients but does not seem to affect their disease-specific survival rate.24 Careful preoperative assessments of organ function and limited lymph node dissection may explain why there are fewer postoperative complications in elderly patients.24 However, we performed extended lymph node dissections in patients with advanced disease for curative surgery, regardless of age, because D2 dissection is the standard at our institute and our 2 surgeons are very experienced with this procedure. The mean number of retrieved lymph nodes in the elderly group was >40, which was not significantly different from the non-elderly group. Moreover, our study showed acceptable complication rates with regard to the extent of resection and lymph node dissection. The connective tissue and lymph nodes of elderly patients are susceptible to easy bleeding during surgery. Therefore, elderly patients are likely to lose a significant amount blood and require transfusions. Transfusions are associated with risks including transfusion-related acute lung injury, multiple organ failure, graft-versus-host disease, and infectious disease transmission.25 Several reports have shown that perioperative transfusions increase postoperative complications,26,27 whereas other studies have shown the opposite to be true.28
In the present study, although there was no significant difference in major surgical complications between the 2 groups, the frequency of intraoperative and postoperative transfusions was significantly higher in the elderly group, as was the incidence of non-surgical complications including atelectasis, pneumonia, and pleural effusion. We also found that old age, comorbidities, and advanced gastric cancer were risk factors for perioperative transfusion (data not shown). The prevalence of obesity in the elderly is growing gradually in our aging society. However, the relationship between obesity and surgical outcomes remains debatable. Some studies in Western countries have reported that obesity is only a simple predictor of wound infection and not a risk factor for major postoperative complications.29 However, evidence in Asian populations suggests that high BMI correlates with increased postoperative complications.30 We found that higher BMI was not a risk factor for postoperative complications. However, subgroup analysis of the elderly group revealed that higher BMI was a risk factor for postoperative complications.
Based on our results, it is difficult to conclude that abnormal pulmonary function or surgical complications are the causes of pulmonary complications in elderly patents. However, postoperative pulmonary problems are more common in elderly patients, as they tend to have chronic obstructive pulmonary disease, have smoked long-term, and have a poor general health status. Therefore, it is necessary to minimize postoperative pulmonary complications by optimizing perioperative lung function using methods such as deep breathing exercises, incentive spirometry, and epidural anesthesia.31
Limitations of this study include the retrospective nature of the study and an inaccurate amount of intraoperative blood loss. Despite these drawbacks, this study demonstrated that perioperative transfusion was an important risk factor for surgical complications in elderly patients with gastric cancer. Another limitation is that we were not able to show long-term surgical outcomes of elderly patients with gastric cancer because our institution is relatively new. Long-term follow-up data will be collected for future analysis.
In conclusion, pulmonary complications were frequent problems in elderly patients after gastric cancer surgery. Higher BMI and perioperative transfusion, particularly postoperative transfusion, were significant risk factors for postoperative complications in elderly patients with gastric cancer.
Figures and Tables
Table 1
Clinicopathological characteristics of elderly patients with gastric cancer undergoing gastrectomies

Table 2
Influence of old age on surgical outcomes of elderly patients with gastric cancer undergoing gastrectomies

Table 3
Postoperative morbidity rates of elderly patients with gastric cancer undergoing gastrectomies

References
1. Statistics Korea. Korean statistical information service [Internet]. Daejeon: Statistics Korea;cited 2012 may 1. Available from: http://Kosis.kr.
2. Bonenkamp JJ, Songun I, Hermans J, Sasako M, Welvaart K, Plukker JT, et al. Randomised comparison of morbidity after D1 and D2 dissection for gastric cancer in 996 Dutch patients. Lancet. 1995; 345:745–748.

3. Cuschieri A, Fayers P, Fielding J, Craven J, Bancewicz J, Joypaul V, et al. The Surgical Cooperative Group. Postoperative morbidity and mortality after D1 and D2 resections for gastric cancer: preliminary results of the MRC randomised controlled surgical trial. Lancet. 1996; 347:995–999.

4. Park DJ, Lee HJ, Kim HH, Yang HK, Lee KU, Choe KJ. Predictors of operative morbidity and mortality in gastric cancer surgery. Br J Surg. 2005; 92:1099–1102.

5. Kim HH, Han SU, Kim MC, Hyung WJ, Kim W, Lee HJ, et al. Long-term results of laparoscopic gastrectomy for gastric cancer: a large-scale case-control and case-matched Korean multicenter study. J Clin Oncol. 2014; 32:627–633.

6. Jeong SH, Ahn HS, Yoo MW, Cho JJ, Lee HJ, Kim HH, et al. Increased morbidity rates in patients with heart disease or chronic liver disease following radical gastric surgery. J Surg Oncol. 2010; 101:200–204.

7. Kim W, Song KY, Lee HJ, Han SU, Hyung WJ, Cho GS. The impact of comorbidity on surgical outcomes in laparoscopy-assisted distal gastrectomy: a retrospective analysis of multicenter results. Ann Surg. 2008; 248:793–799.

8. Sobin LH, Gospodarowicz MK, Wittekind C, editors. International Union against Cancer. TNM Classification of Malignant Tumours. 7th ed. Oxford: Wiley-Blackwell;2009.
9. Winslet MC, Mohsen YM, Powell J, Allum WH, Fielding JW. The influence of age on the surgical management of carcinoma of the stomach. Eur J Surg Oncol. 1996; 22:220–224.

10. Maehara Y, Emi Y, Tomisaki S, Oshiro T, Kakeji Y, Ichiyoshi Y, et al. Age-related characteristics of gastric carcinoma in young and elderly patients. Cancer. 1996; 77:1774–1780.

11. Benhamiche AM, Faivre J, Tazi AM, Couillault C, Villing AL, Rat P. Time trends in diagnostic strategy, treatment, and prognosis of gastric cancer in the elderly: a population based study. Eur J Cancer Prev. 1997; 6:71–77.

12. Crews DE, Zavotka S. Aging, disability, and frailty: implications for universal design. J Physiol Anthropol. 2006; 25:113–118.

13. Oohara T, Johjima Y, Yamamoto O, Tohma H, Kondo Y. Gastric cancer in patients above 70 years of age. World J Surg. 1984; 8:315–320.

14. Takeda J, Tanaka T, Koufuji K, Kodama I, Tsuji Y, Kakegawa T. Gastric cancer surgery in patients aged at least 80 years old. Hepatogastroenterology. 1994; 41:516–520.
15. Otsuji E, Fujiyama J, Takagi T, Ito T, Kuriu Y, Toma A, et al. Results of total gastrectomy with extended lymphadenectomy for gastric cancer in elderly patients. J Surg Oncol. 2005; 91:232–236.

16. Wu CW, Lo SS, Shen KH, Hsieh MC, Lui WY, P'eng FK. Surgical mortality, survival, and quality of life after resection for gastric cancer in the elderly. World J Surg. 2000; 24:465–472.

17. Kunisaki C, Makino H, Takagawa R, Oshima T, Nagano Y, Ono HA, et al. Efficacy of laparoscopy-assisted distal gastrectomy for gastric cancer in the elderly. Surg Endosc. 2009; 23:377–383.

18. Coniglio A, Tiberio GA, Busti M, Gaverini G, Baiocchi L, Piardi T, et al. Surgical treatment for gastric carcinoma in the elderly. J Surg Oncol. 2004; 88:201–205.

19. Lee SR, Kim HO, Yoo CH. Impact of chronologic age in the elderly with gastric cancer. J Korean Surg Soc. 2012; 82:211–218.

20. Kim EJ, Seo KW, Yoon KY. Laparoscopy-assisted distal gastrectomy for early gastric cancer in the elderly. J Gastric Cancer. 2012; 12:232–236.

21. Sharma KC, Brandstetter RD, Brensilver JM, Jung LD. Cardiopulmonary physiology and pathophysiology as a consequence of laparoscopic surgery. Chest. 1996; 110:810–815.

22. Katai H, Sasako M, Sano T, Fukagawa T. Gastric cancer surgery in the elderly without operative mortality. Surg Oncol. 2004; 13:235–238.

23. Endo S, Yoshikawa Y, Hatanaka N, Tominaga H, Shimizu Y, Hiraoka K, et al. Treatment for gastric carcinoma in the oldest old patients. Gastric Cancer. 2011; 14:139–143.

24. Takeshita H, Ichikawa D, Komatsu S, Kubota T, Okamoto K, Shiozaki A, et al. Surgical outcomes of gastrectomy for elderly patients with gastric cancer. World J Surg. 2013; 37:2891–2898.

25. Raghavan M, Marik PE. Anemia, allogenic blood transfusion, and immunomodulation in the critically ill. Chest. 2005; 127:295–307.

26. Bernard AC, Davenport DL, Chang PK, Vaughan TB, Zwischenberger JB. Intraoperative transfusion of 1 U to 2 U packed red blood cells is associated with increased 30-day mortality, surgical-site infection, pneumonia, and sepsis in general surgery patients. J Am Coll Surg. 2009; 208:931–937. 937.e1–937.e2. discussion 938-9.

27. Xenos ES, Vargas HD, Davenport DL. Association of blood transfusion and venous thromboembolism after colorectal cancer resection. Thromb Res. 2012; 129:568–572.

28. Jung DH, Lee HJ, Han DS, Suh YS, Kong SH, Lee KU, et al. Impact of perioperative hemoglobin levels on postoperative outcomes in gastric cancer surgery. Gastric Cancer. 2013; 16:377–382.

29. Mullen JT, Davenport DL, Hutter MM, Hosokawa PW, Henderson WG, Khuri SF, et al. Impact of body mass index on perioperative outcomes in patients undergoing major intra-abdominal cancer surgery. Ann Surg Oncol. 2008; 15:2164–2172.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download