Abstract
Purpose
The aim of this study is to investigate the clinical factors affecting on the cure rate by invasive and open surgery for gastric cancer and to establish a subgroup of patients who can be applied by the early recovery after surgery program through this retrospective analysis.
Materials and Methods
In this retrospective study, we analyzed 425 patients who underwent gastric cancer surgery between January 2011 and December 2011 and were managed with conventional clinical therapies. This clinical algorithm was made when the patient was in minimally invasive surgery group and discharged from hospital one day faster than them in open surgery group.
Results
The completion rate of the clinical pathway was 62.4%. Despite the different applications of clinical pathway, completion rate in minimally invasive surgery group was significantly higher than that of open group (P<0.001). In multivariate analysis, the surgical procedure of minimally invasive surgery (odds ratio=4.281) was the most predictable factor to complete clinical pathway. Additionally, younger patients (odds ratio=1.933) who underwent distal gastrectomy (odds ratio=1.999) without combined resection (odds ratio=3.069) were predicted to accomplish the clinical pathway without any modifications.
Conclusions
We concluded that high efficacy of the clinical pathway for gastric cancer surgery was expected to selected patients through retrospective analysis (expected completion rate=85.4%). In addition, these patients would become enrolled criteria for early recovery program in gastric cancer surgery.
Although the incidence of gastric cancer has been decreased world wide, it is still one of the most common solid tumors in Asian countries like Korea and Japan.1 The standard treatment to be able to improve the survival of the patients diagnosed with the gastric cancer without distant metastasis is surgical resection.2 Therefore, most of patients who have been diagnosed with gastric cancers in Asian countries require the surgical resection for their treatments, and then gastric cancer surgery has become the most of popular surgical procedures.2
The critical pathway (CP) for surgical patients is a standardized plan including preoperative preparation and postoperative managements. For the popularly performed surgery, the standardization of patients care is one of the ways to improve surgical outcomes, reduce the postoperative length of stay and hospital cost.3-6 Regarding with gastric cancer surgery, CP has been rarely suggested due to complicated procedures performed in gastric cancer surgery. However, recent development in gastric cancer surgery has been made the surgical outcome to be improved, and the possibility of application of the CP for perioperative care has been increased.
In particular, minimally invasive surgery (MIS) for early gastric cancer showed the improved surgical outcomes like enhanced postoperative recovery and reduced the length of stay.7-9 Based on these clinical studies, we established different CP according to laparoscopic and open surgeries. The CP was planned as the patients in MIS group start the diet one day faster than them in open group. To date, there had been no report to evaluate the different efficacy about the application of CP according to approach methods in gastric cancer surgery. In this study, we reviewed the results of application of the CP to investigate the clinical factors affecting on the drop from the CP in MIS and open surgery.
After the analysis of this retrospective study, we will progress more advanced CP in which the perioperative care programs for early recovery after surgery (ERAS), so called fast-track CP, like early oral feeding were included. Several results in colon surgery have been reported that it could enhance the recovery of patients, and reduced the length of hospital stay. However, it is not established that ERAS program is acceptance in gastric surgery. Therefore, it is impossible to apply the ERAS program on all patients who underwent gastric cancer surgery. Here, we want to investigate a subgroup of patients who can be applied by the ERAS program through this retrospective analysis for the patients managed with conventional CP.
Our clinical study for ERAS program in gastric cancer surgery was approved by the Institutional Review Board at the Ajou University Hospital, Suwon, Korea (AJIRB-MED-OBS-11-420). Approved clinical study included the retrospective review about the results from patients managed under conventional CP and prospective clinical trial for ERAS. Here, we reported the results from retrospective study.
The Gastric Cancer Center, Ajou University Hospital introduced a standard CP in order to guide perioperative care of the patients who underwent gastric cancer surgery from 2008. Revised version of CP was established to differently manage the patients who underwent MIS including laparoscopic and robotic procedures from 2010, since several prospective researches has been reported that laparoscopic surgery for gastric caner has been improved the recovery after surgery.7,9,10
We operated consecutive 441 patients diagnosed with gastric adenocarcinoma at the Gastric Cancer Center, Ajou University Hospital from January 2011 to December 2011. They did not receive neoadjuvant treatment for gastric cancer diagnosed at this time. Sixteen patients who could not undergo tumor resection for severe advanced disease were excluded. Finally, we analyzed 425 patients in this retrospective study.
Three surgeons (Cho YK, Han SU and Hur H) who had more than 50 gastric cancer surgeries per year were participated in this study. Preoperative gastrofiberscope and computed tomography were performed to exclude the patients with metastatic lesions and to plan the operation including the range of resection, the extent of lymphadenectomy and combined resection. Before surgery, we discussed with patients about the surgical procedures and possibility of postoperative complication. We explained the plan for management after surgery, and obtained informed consents from all patients enrolled in this study. We applied MIS for patients relatively less advanced disease (clinical stage I and stage IIA, American Joint Committee on Cancer [AJCC] 7th edition), but robotic surgery were selected by patients themselves because of the higher cost of it. We have been managed two kinds of CP for gastric cancer surgery in our institution according the approach methods (MIS vs. open surgery). Different and common points of these two pathways were listed in Table 1. These pathways included preoperative bowel preparation by enema, non-per oral diet at one day before surgery in common. Surgical procedures including the resection of primary tumor and lymphadenectomy were performed according to the guideline suggested by Japanese Gastric Cancer Association.11 We planed that the soft diet start at postoperative 5 days for patients underwent MIS and six day for open conventional surgery. All patients were recommended the discharge from a hospital when the patients exhibited tolerability three times of soft diet without complaint and had normal physical condition. As results, there was a difference of one day at the time of discharge from the hospital between two procedures.
The 'Complete' of CP was defined when it was progressed favorably without schedule change, and the patients discharged or recommended at planned schedule. The 'Drop' was defined when that surgeon intentionally changed the schedule because of the preoperative or postoperative observation of the patients' condition and the postoperative complication, or patients were readmitted for various reasons.
Statistical analyses were performed using Statistical Package for Social Science ver. 18.0 (IBM Corp., Armonk, NY, USA). Chi-square tests were adopted to analyze the difference of distribution among the categorized data. We performed the binary logistic regression test for multivariate analysis to predict the drop from CP. A P-value was of 0.05 or less was considered statistically significant.
Comparison between MIS and open groups. During 12 months, we performed MIS for 260 and open surgery for 165 patients. MIS was including 222 patients who operated by laparoscopic surgery and 38 patients by robotic surgery. Although there was no difference in clinical features like age, gender and so on, the rate of palliative resection (P<0.001), total gastrectomy (P=0.003) and combined resection (P=0.004) in MIS group were significantly lower than those in open group (Table 2). In pathologic finding, the proportion of early gastric cancer in the patients who underwent MIS was significantly higher than that in open surgery (P=0.001).
There was significant difference in the complete rate of CP between two procedures (P<0.001). Of 260 patients who underwent MIS for gastric cancer, 198 patients (76.2%) showed the scheduled postoperative recovery without any complaint, and were recommended discharge from hospital. On the other hand, only 67 patients (40.6%) of 165 in open group completed the CP. Common cause of drop from in MIS group was to take care of postoperative complication. However, it was most common cause of drop in open group that surgeons adjusted the planned schedule of CP to observe the patients without postoperative complication. This category included to improve preoperative condition using nutritional support or to manage patients' comorbidity before surgery or to delay discharge due to perioperative non-specific symptom without any complication. This group is called 'desired delay and no readmission group' (Table 3).
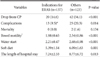
Factors affecting on the drop from CP. Besides open conventional surgery, the rate of drop from CP was significantly increased in old age (P=0.011) and patients who underwent palliative surgery (P=0.007), total gastrectomy (P=0.001) or combined resection (P=0.002) (Table 4). Palliative resection, total gastrectomy and patients' age were predicting factors for the drop from CP in multivariate analysis (Table 5). However, open surgery showed the most obvious factor to predict it (odd ratio=4.281, 2.771 <95 percent c.i. <6.613).
Suggested indications for ERAS in gastric cancer. In our retrospective cohort, 137 patients (32.2%) had the all kinds of factors suggested in multivariated analysis. In these patients, the complete rate of CP was 85.4%, and only 11 patients were dropped due to surgical complication (Fig. 1).
We compared the surgical outcomes of 137 patients who had those factors with them of other 123 patients who underwent MIS (Table 6). Drop from CP and postoperative complication were significantly less frequent in patients who had four factors (P<0.001 and P=0.014). Two case of mortality were occurred only in other group. The postoperative recovery including bowel motility, diet progress and the length of stay of patient who had those factors were faster than those of others.
We investigated the surgical outcomes of complications in patients with indications for ERAS. Except for two patients who diagnosed with wound infection and anastomosis stricture, first symptoms like abdominal pain, fever and abnormality of laboratory were occurred within postoperative four days in most patients. The complications were treated by non-operative managements without mortality (Table 7). Based on those results, we could suggest, 1) MIS 2) no combined resection 3) distal gastrectomy and 4) 65 year old and less, as indications for ERAS in gastric cancer.
We found out the several factors to predict the accomplishment of conventional CP in this retrospective study. According to these results, the surgical procedure of MIS was most predictable factor to complete CP, in spite of faster diet and discharge schedule in CP for patients who underwent MIS. In addition, younger patients who underwent distal gastrectomy without combined resection were predicted to accomplish the CP without modification.
In this study, we want to investigate the subclass of patients with reasonable completion rate for the CP in gastric cancer surgery. The CP in surgical procedure was well established that it could reduce the cost and the length of hospital stay.12,13 However, a previous clinical study reported that the CP for gastrectomy in gastric cancer patients is less effective compared with that in patients with other benign disease.14 The completion rate of the CP was only 19% in that study, on the other hand, 45 to 58% in mastectomy, thyroidectomy and laparoscopic cholecystectomy.14 They assumed that this low efficacy of the CP for gastric cancer surgery resulted from serious operative procedures following with requiring additional medical care. Additional care was mainly required when the postoperative complications were occurred, and the complication rate in gastric cancer surgery was generally known as from 17.5% to 20.1% in cohort studies with large-scale series.15-17 Moreover, these studies suggested that age, combined resection, extension of lymphadectomy or the method of reconstruction would be contributing factors for postoperative morbidities.15,16 Therefore, we expected that the efficacy of the CP for gastric cancer surgery will be increased if the patients for application of the CP were well selected. In our study, 32.2% of all patients had all kinds of factors, which could predict the completion of the CP. They showed the lower complication rate (8.0%) and available complete rate (85.4%) of CP enough to apply it on them.
Recent trends in gastric cancer surgery, which MIS for early gastric cancer has become a widely acceptable procedure, should be considered in this selection.18 Minimally invasive approach to gastric cancer surgery has showed the several benefits like reducing postoperative pain and surgical trauma, enhanced recovery and improved quality of life.8,9,19 As results, most of clinical studies reported that the length of postoperative ileus and hospital stay after surgery were significantly reduced in the gastric cancer patients who underwent MIS.8,9,20 Therefore, we made the different CP between minimally invasive and open surgery for gastric cancer. Based on the results from these previous studies, the diet schedule was delayed one day in the CP for the group of open surgery, and it was planned to stay the postoperative one-day more comparing with it in MIS group. Nevertheless, the complete rate (41.7%) of the CP for open group was significantly lower than it (76.2%) for MIS group. Although there were differences in the distribution of cancer progression, extend of gastric resection and so on, the multivariate analysis showed the MIS was most significant factor for predicting the completion of CP (odd ratio: 4.281). We assumed that increased complication like wound problem and prolonged postoperative ileus, and surgeons' intention of observation in patients who underwent open surgery were contributed to increasing drop rate from the CP.
Besides open surgery, combined resection (odd ratio: 3.069), total gastrectomy (odd ratio: 1.999) and old age (odd ratio: 1.933) were other independent factors which could predict the drop from the CP. Several studies have already reported the morbitidy and mortality after gastric cancer surgery were significantly increased in the elderly.21-23 In addition, other report presented that extent of gastric resection could be significant factors to predict the length of hospital stay.24 Regarding the combined resection, some studies, which evaluated the efficacy of additional splenectomy or pancreatectomy to total gastrectomy in gastric cancer, presented that the combined resection could increase the postoperative complication.25,26 Therefore, it is possible that surgeons predict the frequent occurrence of complication and additional medical care in patients with those factors. In addition, most surgeons want to observe more duration the patients who have the risk factors, despite they present mild symptomatic or laboratory change not related to complications. These reasons might affect on increasing the drop rate from the CP.
These retrospective results were analyzed before design for the prospective clinical study about the ERAS program in patients who underwent gastrectomy with lymphadenectomy for gastric cancer (as NCT01642953 registered in www.clinicaltrials.gov). ERAS program in gastric cancer surgery has been unusually applied due to concerning about the early oral feeding after upper gastrointestinal surgery. However, recent prospective clinical trial of single center reported that the early oral feeding after gastric cancer surgery was feasible.27 This trial showed the complication rate of 25% and the length of hospital stay of 7 days in early oral feeding group. In spite of postoperative early oral feeding, these results were not remarkable outcomes compared with recent outcomes of MIS for gastric cancer. Therefore, we tired to make a plan in order to enhance recovery more after gastric cancer surgery. Developed ERAS program for gastric cancer surgery includes the liquid diet without bowel preparation at the preoperative one day, proper pain management combined with non-opioid drug, fluid restriction, early oral feeding and early discharge at postoperative 4th day. However, under the situation as less evidence of fast track-CP, we thought that it is important to select indicated patients who are expected to perform the ERAS program without sever complications. Of enrolled patients in this retrospective study, selected patients showed the lower complication rate and even the most of complications were detected within 4th postoperative day. Although recent several clinical trials about fast-track surgery for gastric cancer were designed as postoperative 4 days stay in hospital,28,29 we suggested that the application of this schedule on selected patients with suggested indication would be more effective.
In conclusion, high efficacy of the CP for gastric cancer surgery was expected to selected patients through retrospective analysis. In addition, these patients would become enrolled criteria for early recovery program in gastric cancer surgery.
Figures and Tables
 | Fig. 1Outcomes of patients selected by novel criteria for early recovery program in gastric cancer surgery. |
Table 1
Critical pathway for gastrectomy with lymphadenecetomy in gastric cancer patients at Ajou university hospital, 2011

Table 5
Predicting factors which can predict the drop from critical pathway in gastric cancer surgery by multivariable analysis

Acknowledgments
We especially thank to physician assistants (Nr. Yun Hwa Cho and Nr. Seon Mi Eom) and coordinator (Nr. Mi Sun Yang) in Gastric Cancer Center, Ajou University Hospital, who contributed to the record of clinical data and management for patients enrolled in this study.
This study was supported by a grant from the National R&D Program for Cancer Control, Ministry of Health & Welfare, Republic of Korea (1320270).
References
3. Bradshaw BG, Liu SS, Thirlby RC. Standardized perioperative care protocols and reduced length of stay after colon surgery. J Am Coll Surg. 1998; 186:501–506.

4. Kulkarni RP, Ituarte PH, Gunderson D, Yeh MW. Clinical pathways improve hospital resource use in endocrine surgery. J Am Coll Surg. 2011; 212:35–41.

5. Lin YK, Chen CP, Tsai WC, Chiao YC, Lin BY. Cost-effectiveness of clinical pathway in coronary artery bypass surgery. J Med Syst. 2011; 35:203–213.

6. Uchiyama K, Takifuji K, Tani M, Onishi H, Yamaue H. Effectiveness of the clinical pathway to decrease length of stay and cost for laparoscopic surgery. Surg Endosc. 2002; 16:1594–1597.

7. Hayashi H, Ochiai T, Shimada H, Gunji Y. Prospective randomized study of open versus laparoscopy-assisted distal gastrectomy with extraperigastric lymph node dissection for early gastric cancer. Surg Endosc. 2005; 19:1172–1176.

8. Kim YW, Baik YH, Yun YH, Nam BH, Kim DH, Choi IJ, et al. Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: results of a prospective randomized clinical trial. Ann Surg. 2008; 248:721–727.

9. Kitano S, Shiraishi N, Fujii K, Yasuda K, Inomata M, Adachi Y. A randomized controlled trial comparing open vs laparoscopyassisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery. 2002; 131:S306–S311.

10. Lee JH, Han HS, Lee JH. A prospective randomized study comparing open vs laparoscopy-assisted distal gastrectomy in early gastric cancer: early results. Surg Endosc. 2005; 19:168–173.

11. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011; 14:113–123.
12. Dy SM, Garg P, Nyberg D, Dawson PB, Pronovost PJ, Morlock L, et al. Critical pathway effectiveness: assessing the impact of patient, hospital care, and pathway characteristics using qualitative comparative analysis. Health Serv Res. 2005; 40:499–516.

13. Pritts TA, Nussbaum MS, Flesch LV, Fegelman EJ, Parikh AA, Fischer JE. Implementation of a clinical pathway decreases length of stay and cost for bowel resection. Ann Surg. 1999; 230:728–733.

14. Jeong SH, Yoo MW, Yoon HM, Lee HJ, Ahn HS, Cho JJ, et al. Is the critical pathway effective for the treatment of gastric cancer? J Korean Surg Soc. 2011; 81:96–103.

15. Park DJ, Lee HJ, Kim HH, Yang HK, Lee KU, Choe KJ. Predictors of operative morbidity and mortality in gastric cancer surgery. Br J Surg. 2005; 92:1099–1102.

16. Persiani R, Antonacci V, Biondi A, Rausei S, La Greca A, Zoccali M, et al. Determinants of surgical morbidity in gastric cancer treatment. J Am Coll Surg. 2008; 207:13–19.

17. Wu CW, Hsieh MC, Lo SS, Wang LS, Hsu WH, Lui WY, et al. Morbidity and mortality after radical gastrectomy for patients with carcinoma of the stomach. J Am Coll Surg. 1995; 181:26–32.
18. Hur H, Xuan Y, Ahn CW, Cho YK, Han SU. Trends and outcomes of minimally invasive surgery for gastric cancer: 750 consecutive cases in seven years at a single center. Am J Surg. 2013; 205:45–51.

19. Yasunaga H, Horiguchi H, Kuwabara K, Matsuda S, Fushimi K, Hashimoto H, et al. Outcomes after laparoscopic or open distal gastrectomy for early-stage gastric cancer: a propensity-matched analysis. Ann Surg. 2013; 257:640–646.

20. Lee SI, Choi YS, Park DJ, Kim HH, Yang HK, Kim MC. Comparative study of laparoscopy-assisted distal gastrectomy and open distal gastrectomy. J Am Coll Surg. 2006; 202:874–880.

21. Katai H, Sasako M, Sano T, Fukagawa T. Gastric cancer surgery in the elderly without operative mortality. Surg Oncol. 2004; 13:235–238.

22. Kunisaki C, Akiyama H, Nomura M, Matsuda G, Otsuka Y, Ono HA, et al. Comparison of surgical outcomes of gastric cancer in elderly and middle-aged patients. Am J Surg. 2006; 191:216–224.

23. Winslet MC, Mohsen YM, Powell J, Allum WH, Fielding JW. The influence of age on the surgical management of carcinoma of the stomach. Eur J Surg Oncol. 1996; 22:220–224.

24. Bozzetti F, Marubini E, Bonfanti G, Miceli R, Piano C, Crose N, et al. The Italian Gastrointestinal Tumor Study Group. Total versus subtotal gastrectomy: surgical morbidity and mortality rates in a multicenter Italian randomized trial. Ann Surg. 1997; 226:613–620.
25. Csendes A, Burdiles P, Rojas J, Braghetto I, Diaz JC, Maluenda F. A prospective randomized study comparing D2 total gastrectomy versus D2 total gastrectomy plus splenectomy in 187 patients with gastric carcinoma. Surgery. 2002; 131:401–407.

26. Otsuji E, Yamaguchi T, Sawai K, Okamoto K, Takahashi T. Total gastrectomy with simultaneous pancreaticosplenectomy or splenectomy in patients with advanced gastric carcinoma. Br J Cancer. 1999; 79:1789–1793.

27. Hur H, Kim SG, Shim JH, Song KY, Kim W, Park CH, et al. Effect of early oral feeding after gastric cancer surgery: a result of randomized clinical trial. Surgery. 2011; 149:561–568.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download