Abstract
Through the advent of surgical techniques and the improvement of laparoscopic tools including the ultrasonic activated scissor, laparoscopic gastrectomy has been increasingly used in far more cases of benign or malignant gastric lesions for the benefit of patients without compromising therapeutic outcomes. Even though possible complications provoked by the ultrasonic activated scissor can be prevented during the procedure with increasing advanced laparoscopic experience and supervision, unexpected late complications after the operations rarely occur. An extremely rare case of left incarcerated diaphragmatic hernia of the transverse colon developed in an 81-year-old female patient as a late complication, 8 months after laparoscopy-assisted total gastrectomy for gastric cancer, with laparoscopy successfully resumed and without the need to sacrifice any portion of the bowel.
To date, conventional open gastrectomy for the gastric cancer has been gaining superior popularity than the laparoscopic counterpart. However, many of the laparoscopic enthusiasts strongly believe that totally laparoscopic or laparoscopy-assisted gastrectomy, either distal or total gastrectomy, may not be worse than the open gastrectomy in terms of oncologic outcomes.(1) Even though all kinds of laparoscopic procedures are considered as the less invasive ones than laparotomies, laparoscopic operations always carry their own pitfalls to entail some risk of morbidity. In exchange for patients' benefit, surgeons are supposed to suffer themselves from time-consuming hands-on training to overcome the learning curve and physical exertion during the laparoscopic procedures.
Fortunately, lots of technological improvements on the instruments have been boosting the effectiveness and efficacy of laparoscopic procedures by making laparoscopic surgeons' ideas coming true. These specific laparoscopic instruments, such as ultrasonic activated scissor, many of the graspers or stapling devices, are very useful and safe, but may harbor potential problems to result in early or late complications during the procedure if used without thorough precaution, which mandates laparoscopic surgeons to stay alert to prevent or locate any kinds of morbidity by iatrogenic injuries by the end of the operation.(2-4)
Many have reported on the successful laparoscopic repair of the diaphragmatic hernia, regardless of its etiology and there has been a few reports commenting this complication.(5,6) However, those not only developed after esophageal surgery but also localized at hital area. On the other hand, late occurring diaphragmatic hernia, by the iatrogenic injury during the previous laparoscopy-assisted total gastrectomy, resulting in transverse colon herniation into the chest is a very rare one.
Herein, we report the details of that case, which we ought to have experienced.
An 81-year-old woman with progressing upper abdominal pain for the past three days underwent routine chest radiography, which showed an ill-defined, low density mass with air that measured more than 5 cm in diameter and changed the left cardiophrenic angle into opaque density with air-fluid level (Fig. 1). Eight months ago, by full laparoscopic approach, she had undergone total gastrectomy with Roux-en-Y reconstruction for gastric carcinoma (pT3N0M0) at the cardia. At that time, she returned to her house on the ninth postoperative day without any morbid conditions. By routine follow-up taken six months after the total gastrectomy, anything that might either indicate any recurrence or suggest sign or symptom of left sided diaphragmatic injury was not found.
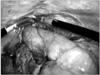
Contrast-enhanced, abdominal computed tomography with coronal reconstruction easily pointed out herniated bowel into the left pleural cavity through a possible defect of the left hemidiaphragm (Fig. 2). All the hematologic and biochemical values from the blood were within the reference ranges. Right after getting diagnosis, she necessitated surgical intervention. Under general anesthesia, she underwent laparoscopic exploration to correct her surgical problem. All the ports used at the previous operation were recruited for this herniorrhaphy. Rarely, intraabdominal adhesion was found, except herniated transverse colon through the defect on the left sided diaphragm (Fig. 3). Herniated colon with some exudates but no ischemic sign was drawn safely with graspers back into the abdominal cavity after extending the defect about 2.5 cm long. Before we applied Gore-Tex mesh (6×6 cm) on the diaphragmatic hernia site, the opening in the diaphragm had been debrided and closed thoroughly with non-absorbable Prolene 2-0 sutures by intracorporeal continuous suture. After then, Gore-Tex mesh was applied above the suture site and fixed interrupted sutures to reinforce and to prevent any possible recurrent hernia. She could fully regain her normal condition rapidly, and discharged on the seventh postoperative day.
Laparoscopic gastrectomy has been gathering scientific evidences to prove its potential as an alternative to the conventional laparotomy by maximizing patients' benefits and minimizing morbidity without compromising oncologic outcomes represented by locoregional recurrences or metastases.(1,7) Many attempts have been tried to improve technical drawbacks of laparoscopic operations, which have resulted in the inventions of ultrasonic activated scissors and others.(8) Meticulous intraoperative use of ultrasonic activated scissor rarely provokes tissue damage, but some kinds of iatrogenic injuries can be entailed if intraoperative negligence or premature experience had been given.
Ultrasonic activated scissor has been gaining widespread enthusiasm among laparoscopic surgeons, because it can help to reduce operation time and surgeons' work to dissect the tissue away without profuse bleeding. In this case, we can't figure out the exact other energy source of damaging for diaphragm except ultrasonic activated scissor only device emitting energy during operation. Because tumor was located at cardia, dissection of gastric fundus from surrounding structure and paraesophageal lymph nodes was carried by ultrasonic activated scissor. In itself, diaphragmatic hernia after operations, either conventionally or laparoscopically, has been rarely reported and more than six months after the initial operation is an extremely rare one. Mostly, this complication has been known to develop after esophagectomy.(9,10) Unfortunately, we had used 30 degree rigid electro-laparoscope, which might prevent us from getting full view of those left to esophagus and superior pole of spleen. We suspect that the energy possibly from the ultrasonic activated scissor was sufficient to provoke a weak point in that area, and brought on further diaphragmatic hernia progressively. In addition to the diaphragmatic tissue damage directly by the ultrasonic activated scissor under poor visual inspection, probable sparse adhesion around the crura and left diaphragm might be the reason of this far delayed complication in the elderly patient.(10) With consideration to position of hernia located 3 cm from left crus muscle and attendant circumstances, it might be strongly correlated with ultrasonic activated scissor.
Patients having a diaphragmatic hernia might have a chance to experience repeated respiration difficulty, abdominal cramp or even intestinal obstruction in case of incarceration, so the physicians should take into consideration of grave complications from the incarceration or strangulation of bowels, such as death or even a systemic shock.(11) Just like this case, diaphragmatic hernia comprised of bowels can easily be diagnosed by routine chest radiography and auscultation to see the abnormal density into the thoracic cavity accompanied by air bubbles and to hear intestinal peristaltic sound, which can be supported by additional imaging studies such as computed tomography with acceptable diagnostic accuracy.(12) Typically, diaphragmatic hernia along with pleural effusion may show sinus cut-off sign that means obliterated posterior costophrenic sulcus shadow by the herniated bowel itself or pleural effusion, which can be seen in computed tomogram or even in routine chest film.(13) Presumably, she had developed diaphragmatic hernia commencing forty eight or seventy two hours before the diagnosis, considering the follow-up radiologic studies including chest film taken two months before the onset of this complication were normal.
Laparoscopic herniorrhaphy of the diaphragmatic defects has proven itself effective and efficacious without further need to open abdominal or thoracic cavity in many cases. If associated solid organ or bowel damage is anticipated, care should be taken to choose laparoscopic procedure. But, other than that, laparoscopic repair can be considered as first choice, especially for the late onset cases with stable patient's condition.(14) Indeed, it was reported that defects in the hemidiaphragm was easier site for the secure of the hole.(15) In this case, the defect was confined in the left hemidiaphragm and a delayed one, so we needed to use polytetrafluoroethylene mesh to abolish the lesion without unfavorable tension. And a few intra-abdominal adhesions developed after previous laparoscopic total gastrectomy helped us to finish all the procedures laparoscopically without any difficulty.
In conclusion, during laparoscopy-assisted total gastrectomy near to the diaphragm, while using ultrasonic activated scissor or electrocautery, especially behind the esophagogastric junction where giving poor view, surgeon should be very careful not to disseminate any energy from these instruments to prevent any possible damage that can result in iatrogenic diaphragmatic hernia sequestering in incarceration or even strangulation of the herniated bowels. It will be help to by keeping the active blade away from the surface of the diaphragm accompanying with good surgical field. In addition, delayed-onset diaphragmatic damage should be suspected in patients complaining pain or discomfort during follow-up, although it is very rare. Needless to say, prevention and a good number of experiences with ultrasonic activated scissor should be the best measures to avoid this complication.
Figures and Tables
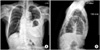 | Fig. 1(A, B) Preoperative plain chest film showed air-fluid levels by the herniated bowels in the left pleural cavity. |
References
1. Shehzad K, Mohiuddin K, Nizami S, Sharma H, Khan IM, Memon B, et al. Current status of minimal access surgery for gastric cancer. Surg Oncol. 2007. 16:85–98.

2. Farn J, Hammerman AM, Brunt LM. Intraoperative pneumothorax during laparoscopic cholecystectomy: a complication of prior transdiaphragmatic surgery. Surg Laparosc Endosc. 1993. 3:219–222.
3. Eder F, Putzki H, Tautenhahn E. Right-sided pneumothorax in laparoscopic cholecystectomy. Chirurg. 1994. 65:484–485.
4. Armstrong PA, Miller SF, Brown GR. Diaphragmatic hernia seen as a late complication of laparoscopic cholecystectomy. Surg Endosc. 1999. 13:817–818.

5. Kent MS, Luketich JD, Tsai W, Churilla P, Federle M, Landreneau R, et al. Revisional surgery after esophagectomy: an analysis of 43 patients. Ann Thorac Surg. 2008. 86:975–983.

6. Vallböhmer D, Hölscher AH, Herbold T, Gutschow C, Schröder W. Diaphragmatic hernia after conventional or laparoscopic-assisted transthoracic esophagectomy. Ann Thorac Surg. 2007. 84:1847–1852.

7. Kim JJ, Song KY, Chin HM, Kim W, Jeon HM, Park CH, et al. Totally laparoscopic gastrectomy with various types of intracorporeal anastomosis using laparoscopic linear staplers: preliminary experience. Surg Endosc. 2008. 22:436–442.

8. Besozzi A, Besozzi S, Lanza V, Mitolo CI, Novelli D, Sisto T. Laparoscopic treatment gastric cancer with advanced techniques: technical notes and follow-up. Chir Ital. 2007. 59:63–67.
9. Balázs A, Forgács A, Flautner L, Kupcsulik P. A case of unusual complication of diaphragmatic herniation of transverse colon following transhiatal esophagectomy. Orv Hetil. 1997. 138:2535–2538.
10. Aly A, Watson DI. Diaphragmatic hernia after minimally invasive esophagectomy. Dis Esophagus. 2004. 17:183–186.

11. Kuhn R, Schubert D, St Wolff, Marusch F, Lippert H, Pross M. Repair of diaphragmatic rupture by laparoscopic implantation of a polytetrafluoroethylene patch. Surg Endosc. 2002. 16:1495.

12. Killeen KL, Mirvis SE, Shanmuganathan K. Helical CT of diaphragmatic rupture caused by blunt trauma. AJR Am J Roentgenol. 1999. 173:1611–1616.

13. Kaya SO, Karabulut N, Yuncu G, Sevinc S, Kiroğlu Y. Sinus cut-off sign: a helpful sign in the CT diagnosis of diaphragmatic rupture associated with pleural effusion. Eur J Radiol. 2006. 59:253–256.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download