Abstract
Regarding the removal of a gastric bezoar, laparoscopic surgery was performed and it was shown that the laparoscopic approach is safe and feasible. However, the laparoscopic method has the risk of intraabdominal contamination, when the gastric bezoar is retrieved from the gastric lumen in the peritoneal cavity. We developed and applied a new procedure for the removal of the gastric bezoar using one surgical glove and two wound retractors as a fashion of intragastric single port surgery. Herein we present this new minimal invasive procedure, so named "hybrid access surgery" which involves the use of existing devices and overcomes the weakness of laparoscopic removal of the gastric bezoar. Our new procedure, combining the concept of intragastric and single port access, is acceptable and feasible to retrieve the gastric bezoar. In the future, this procedure may be one of the alternative procedures for retrieving gastric bezoar even when it is incarcerated in the pylorus.
Gastric bezoar is not a common disease; however, it may become the reason for an intraluminal obstruction. Non-operative management of gastric bezoar such as medication and endoscopic fragmentation and retrieval has been proposed for treatment.(1,2) If these treatments fail, surgical approach is needed and removal of the bezoar has classically been performed by gastrotomy.
Recently, the advancement of surgical instruments has produced new surgical procedures and minimally invasive surgery such as laparoscopic surgery and single-port surgery is gaining considerable interest.(3-6) Regarding the removal of gastric bezoar, laparoscopic surgery has previously been performed and it was shown that the laparoscopic approach is safe and feasible.(7-12) However, the laparoscopic method has a risk of intraabdominal contamination, when the gastric bezoar is retrieved from the gastric lumen in the peritoneal cavity. If the bezoar is incarcerated into the pylorus, the decision of the location of gastrotomy is difficult because of the risk of pyloric stricture.
We encountered a 77 year old female patient who had a complaint of an epigastralgia derived from the gastric bezoar incarcerated in the pylorus. We developed and applied a new procedure for the removal of the bezoar using one surgical glove and two duplicated small wound protectors as a fashion of intragastric single port surgery. Herein, we present this new minimal invasive procedure, so named "hybrid access surgery", which involves the use of existing devices and overcomes the weakness of the laparoscopic removal of the gastric bezoar.
A 77 year old woman with diabetes and old cerebellar ataxia received an upper gastrointestinal endoscopic examination for a recurrent intermittent epigastralgia and epigastric fullness. Endoscopic finding showed a gastric ulcer (A1 stage) at the prepylorus and a gastric bezoar of 4 cm in diameter in the pyloric channel (Fig. 1A). Abdominal computed tomography scan revealed a substantial intragastric mass at the pylorus (Fig. 1B). We decided to retrieve this massive bezoar by surgical approach due to the difficulty of endoscopic removal.
Under general anesthesia, a 4 cm mid-line incision was made at the supra-umbilical area. After laparotomy, a small wound protector (Alexis® Applied Medical, Rancho Santa Margarita, CA, USA) was inserted from the skin to the peritoneum to prevent the wound from contamination. The stomach was pulled out of the wound and a longitudinal gastrotomy of about 3 cm in length was made at the anterior wall of the stomach body. Around the gastrostomy site, four 3-0 silk stay sutures were made to secure the traction of the anterior gastric wall (Fig. 2A). While keeping traction of the stomach to the extra-peritoneum, another wound protector was inserted from the skin wound to the gastric lumen (Fig. 2B). A surgical glove as a homemade single port device was employed to wrap the wound protector and 2 access ports (12 mm and 5 mm in diameter) were secured with a tie to fingers of the glove. While intra-gastric pneumatic pressure was established with 12 mm Hg, a 30 degree laparoscope was inserted through the 12 mm port and the laparoscopic instrument was introduced via the 5 mm port (Fig. 2C).
Since the gastric bezoar was easily confirmed laparoscopically to be impacted in the pylorus, endo-forceps were employed to retrieve and break up the bezoar into the stomach body (Fig. 2D). After the glove was removed, the fragment of the bezoar was directly retrieved by forceps through the gastrotomy. The content of the bezoar contained seeds of persimmon, and is considered as phytobezoar derived from persimmon. After confirming the hemostasis of the gastric lumen, the inner side wound protector was removed (Fig. 2E). The gastrotomy was closed using endolinear staplers (Fig. 2F). Interrupted 3-0 silk sutures were made to the staple line for reinforcement (Fig. 2G). Then, the outer wound protector was removed and the fascial incision was closed, followed by skin closure (Fig. 2H). The total operation time was 69 minutes. The patient recovered uneventfully. The patient resumed a soft diet 3 days after the operation and was discharged 5 days after the operation.
This technical report describes a novel application of a single port intragastric operative procedure for intraluminal pathology. Our new procedure combining the concept of intragastric and single port access, so named "hybrid access surgery", is simple and securely accomplished to retrieve the gastric bezoar. The surgeon was able to perform the operative procedure without contamination in the peritoneal cavity.
Due to good postoperative outcomes of less pain, faster recovery and cosmesis, minimally invasive surgery such as laparoscopic surgery and single port access surgery is becoming popular and the number of these surgeries being performed is increasing.(3-6) Bezoars are the most common type of foreign body that can lodge in the stomach and can increase in size by the accretion of nonabsorbable food or fiber.(11) Endoscopic or medical treatments are currently being used; however, the failure in non-surgical treatment requires surgical intervention.(8) Recently, several authors have reported good results of laparoscopic removal of gastric bezoar.(7-11) In these laparoscopic procedures, gastrotomy was performed intracorporeally under the pneumoperitoneum and the bezoar was placed into a water-impervious bag. To avoid making a large incision, the bezoars were fragmentized and extracted.
However, these procedures have two shortcomings. One is the risk of intraabdominal contamination. Gastric bezoar is often easily broken and the spilled fragments may have a risk of intraabdominal abscess formation. The other shortcoming is the difficulty in deciding the location of the gastrotomy. If the bezoar is impacted in the pylorus such as in the case presented in this report, the gastrotomy should be made near the pylorus in the laparoscopic procedure for easier retrieval of the gastric bezoar. However, there may be a high risk of stricture of the pylorus. Although intragastric surgery is one of the options in the management of gastric bezoar,(13) this procedure is not common because of the complicated procedure of trocar placement while guiding endoscopically and the time-consuming procedure of the removal of the bezoar.
To overcome these shortcomings, we developed the present procedure which is quite simple using two wound protectors.(14) By using duplicated wound protectors, not only the wound, but also the peritoneal space is completely protected from the spillage of the gastric contents or the gastric bezoar. The scope involved directly introducing the gastric lumen at the middle of the anterior stomach and it is easy to confirm the bezoar. Furthermore, extracorporeal closure of the gastrotomy is significantly easier than the intracorporeal procedure.
Although our procedure has shown a satisfactory result, there are some limitations. One is the difficulty in deciding the position of the skin incision. According to the body shape of the patients and the size of the stomach, the movement from the access port may be restricted. We suggest that a preoperative CT scan should be examined under full gastric distension. Another limitation is the difficulty in maintaining intragastric pneumatic pressure. In such a difficult case, temporal occlusion of the jejunal lumen is helpful. Another limitation is the difficulty of grasping the bezoar. We used only one endo-forceps. However, in a difficult case, the additional securing of the trocar to the surgical glove may be helpful by making the procedure easier without the need to make another incision. However, this is the first technical report of the present procedure combining intragastric and single port surgery and has strong benefits not only for the prevention of contamination but is also a safe procedure in maintaining the concept of minimally invasive surgery.
In conclusion, our new procedure combining the concept of intragastric and single port access is acceptable and feasible for retrieving a gastric bezoar. In the future, this procedure may be an alternative procedure for retrieving a gastric bezoar even in cases where it is impacted in the pylorus.
Figures and Tables
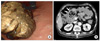 | Fig. 1Preoperative diagnosis of gastric bezoar. (A) Endoscopic finding of gastric bezoar. (B) Heterogeneous mass (arrows) in the pylorus revealed by computed tomography scan. |
 | Fig. 2Operative procedure. (A) Securing gastrotomy with stay sutures at the incision site. (B) Intragastric application of wound protector. (C) Homemade single port device using a surgical glove with 2 access ports (12 mm and 5 mm in diameter) through the glove fingers. (D) Laparoscopic removal of a gastric bezoar impacted in the pylorus. (E) Removal of impacted gastric bezoar through gastrotomy. (F) Closure of gastrotomy with linear staplers. (G) After reinforcement sutures of gastrotomy site in the peritoneal cavity. (H) A 4 cm sized supraumbilical skin incision After closure. |
Acknowledgments
This work was supported by a grant of the Korea Healthcare technology R&D project, Ministry of Health, Welfare, & Family Affairs, Republic of Korea (A084120).
References
1. Blam ME, Lichtenstein GR. A new endoscopic technique for the removal of gastric phytobezoars. Gastrointest Endosc. 2000. 52:404–408.

2. Wang YG, Seitz U, Li ZL, Soehendra N, Qiao XA. Endoscopic management of huge bezoars. Endoscopy. 1998. 30:371–374.

3. Bucher P, Pugin F, Morel P. From single-port access to laparoendoscopic single-site cholecystectomy. Surg Endosc. 2010. 24:234–235.

4. Romanelli JR, Roshek TB 3rd, Lynn DC, Earle DB. Single-port laparoscopic cholecystectomy: initial experience. Surg Endosc. 2010. 24:1374–1379.

5. Merchant AM, Cook MW, White BC, Davis SS, Sweeney JF, Lin E. Transumbilical Gelport access technique for performing single incision laparoscopic surgery (SILS). J Gastrointest Surg. 2009. 13:159–162.

6. Langwieler TE, Nimmesgern T, Back M. Single-port access in laparoscopic cholecystectomy. Surg Endosc. 2009. 23:1138–1141.

7. Fraser JD, Leys CM, St Peter SD. Laparoscopic removal of a gastric trichobezoar in a pediatric patient. J Laparoendosc Adv Surg Tech A. 2009. 19:835–837.

8. Song KY, Choi BJ, Kim SN, Park CH. Laparoscopic removal of gastric bezoar. Surg Laparosc Endosc Percutan Tech. 2007. 17:42–44.

9. Shami SB, Jararaa AA, Hamade A, Ammori BJ. Laparoscopic removal of a huge gastric trichobezoar in a patient with trichotillomania. Surg Laparosc Endosc Percutan Tech. 2007. 17:197–200.

10. Meyer-Rochow GY, Grunewald B. Laparoscopic removal of a gastric trichobezoar in a pregnant woman. Surg Laparosc Endosc Percutan Tech. 2007. 17:129–132.

11. Yao CC, Wong HH, Chen CC, Wang CC, Yang CC, Lin CS. Laparosopic removal of large gastric phytobezoars. Surg Laparosc Endosc Percutan Tech. 2000. 10:243–245.

12. Nirasawa Y, Mori T, Ito Y, Tanaka H, Seki N, Atomi Y. Laparoscopic removal of a large gastric trichobezoar. J Pediatr Surg. 1998. 33:663–665.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download