Abstract
Purpose
Intracorporeal anastomosis during laparoscopic gastrectomy is becoming increasingly prevalent. However, selection of the anastomosis method after laparoscopic distal gastrectomy is equivocal because of a lack of technical feasibility and safety. We compared intracorporeal gastroduodenostomy with gastrojejunostomy using linear staplers to evaluate the technical feasibility and safety of intracorporeal anastomoses as well as its' minimally invasiveness.
Materials and Methods
Retrospective analyses of a prospectively collected database for gastric cancer revealed 47 gastric cancer patients who underwent laparoscopic distal gastrectomy with either intracorporeal gastroduodenostomy or gastrojejunostomy from March 2011 to June 2011. Perioperative outcomes such as operation time, postoperative complication, and hospital stay were compared according to the type of anastomosis. Postoperative inflammatory response was also compared between the two groups using white blood cell count and high sensitivity C-reactive protein.
Results
Among the 47 patients, 26 patients received gastroduodenostomy, whereas 21 patients received gastrojejunostomy without open conversion or additional mini-laparotomy incision. There was no difference in mean operation time, blood loss, and length of postoperative hospital stays. There was no statistically significant difference in postoperative complication or mortality between two groups. However, significantly more staplers were used for gastroduodenostomy than for gastrojejunostomy (n=6) than for gastroduodenostomy and (n=5).
Conclusions
Intracorporeal anastomosis during laparoscopic gastrectomy using linear stapler, either gastroduodenostomy or gastrojejunostomy, shows comparable and acceptable early postoperative outcomes and are safe and feasible. Therefore, surgeons may choose either anastomosis method as long as oncological safety is guaranteed.
With the help of screening program for gastric cancer, the detection of early gastric cancer is increasing in Korea. In recent years, more and more gastric cancer patients in Korea are diagnosed as early gastric cancer.(1,2) Along with increased proportion of early gastric cancer, laparoscopic gastrectomy is also increasing because of its minimally invasiveness.(1) Along with the increase of endoscopic treatment of early gastric cancer, laparoscopic surgery is being a preferred option for early gastric cancer surgery. Thus, laparoscopy-assisted procedures for gastric cancer are becoming popular which results in an improved quality of life. However, laparoscopy assisted gastrectomy still requires an additional mini-laparotomy incision to perform the anastomosis. Furthermore, making anastomosis through a mini-laparotomy may diminish the potential minimally invasiveness, especially for obese patients for whom requires longer mini-laparotomy.
By eliminating the mini-laparotomy, intracorporeal anastomosis may improve cosmetic result as well as clinical outcomes such as earlier bowel function recovery.(3) Various types of intracorporeal anastomosis after distal gastrectomy have been introduced and reported to be a safe and simple method.(3-5) However, there has been no report that compared the different types of the intracorporeal anastomosis method in terms of their postoperative outcomes. We compared intracorporeal gastroduodenostomy with gastrojejunostomy to evaluate the technical feasibility and safety of intracorporeal anastomoses as well as it's minimally invasiveness.
A retrospective review of a prospectively collected database for gastric cancer revealed 47 gastric cancer patients who underwent laparoscopic distal gastrectomy from March 2011 to June 2011. All these 47 laparoscopic gastrectomies were performed with either intracorporeal gastroduodenostomy or gastrojejunostomy. These 47 patients were divided into two groups for comparison: gastroduodenostomy (n=26) and gastrojejunostomy (n=21) group. Patient demographics, underlying diseases, data on surgery, data on preoperative and postoperative monitoring including complications and length of hospital stays, and pathologic results were compared between the two groups.
All the operations were performed by a single surgeon with same operative methods at the Department of Surgery, Yonsei University College of Medicine. In our institution, minimally invasive surgery for gastric cancer was performed on patients, who were diagnosed as having early stage gastric cancer preoperatively (in other words, when there is no evidence of tumor invasion to serosa of stomach wall or extraperigastric lymph node metastasis) with the exception of those who with lesions for endoscopic mucosal resection. All patients eligible for minimally invasive surgery were informed about the operative procedure, as well as open gastrectomy. Patients with early stage gastric cancer were allowed to choose the type of operation, either minimally invasive or open surgery. All patients provided a written informed consent for an operation at the time of surgery.
All patients in this study underwent laparoscopic distal gastrectomy with either gastroduodenostomy or gastrojejunostomy including D1+β or D2 lymphadenectomy according to the rules of the Japanese Research Society for Gastric Cancer.(6) Detailed description of surgical procedure for laparoscopic distal gastrectomy especially for lymph node dissection was presented elsewhere.(7) To detect the intraluminal lesion which was marked with endoscopic clips the before the operation and to decide the resection line, intraoperative plain radiography was taken after applying the clips on the greater and the lesser curvature of the stomach.(8) Then intestinal continuity was restored either gastroduodenostomy or gastrojejunostomy based on the tumor location. Gastroduodenostomy was performed whenever it was possible to get the tumor-free margins.
Intracorporeal gasrtoduodestomy was performed using linear staplers, similar to so-called Delta-shape anastomosis.(3-5) After the dissection of the infrapyloric area and making a window just distal to pylorus, the duodenum is transected from posterior to the anterior wall using a 45 mm endoscopic linear stapler with blue cartilage which was inserted through a port in the left flank area. After completing the all lymph node dissection, stomach was resected from greater curvature to lesser curvature by applying two 60 mm endoscopic linear staplers with blue cartilage through a port in the left flank area. After resection, the specimen was placed in a plastic bag and placed at lower abdominal cavity. Small holes were created along the edge of the grater curvature of the remnant stomach and the medial edge of the duodenum. A 45 mm endoscopic linear stapler with blue cartilage was placed between the remnant stomach and duodenum (cartilage in the stomach and anvil into the duodenum), and then the posterior wall of the remnant stomach and the posterior wall of the duodenum were approximated by the stapler. By firing the stapler, the common channel between the stomach and the duodenum was made. The entry hole left was also closed by linear staplers. When closing the common entry hole, previous stapled duodenal stump was also removed to secure the blood supply to the duodenum.
Intracorporeal gastrojejunostomy was performed by a side-to-side fashion using linear staplers. Small holes were created at the grater curvature of the remnant stomach and the antimesenteric border of the jejunum. A 60 mm endoscopic linear stapler with blue cartilage was placed between the remnant stomach and jejunum (cartilage in the stomach and anvil into the jejunum), and then the greater curvature of the remnant stomach and the antimesenteric border of the jejunum were approximated by the stapler through a left flank port. The length of the afferent loop was made as short as possible unless tension was made. The common entry hole was closed by a 60 mm linear stapler through a right flank port.
After the operation, a standardized postoperative care protocol was applied to both groups as follows. When patients were tolerable, sips of water were permitted from postoperative day 2, a liquid diet was given on postoperative day 3, and a soft diet was started on postoperative day 4. After 1 day of a soft diet without complications, patients were encouraged to be discharged.
We performed all statistical analyses using the Statistical Package for Social Science (SPSS) version 18.0 for Microsoft Windows (SPSS Inc., Chicago, IL, USA). Student t-test was used to analyze the mean differences in continuous variables between the groups. Mixed model analysis was use to compare the laboratory results of white blood cell count and high sensitivity C-reactive protein between the groups. Chi-square test was used to compare categorical variables. All P-values less than 0.05 were regarded as statistically significant.
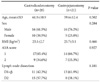
All 47 gastric cancer patients in this study underwent laparoscopic distal gastrectomy with either gastroduodenostomy or gastrojejunostomy without open conversion or additional mini-laparotomy incision. Patients' characteristics are shown in Table 1. There was no significant difference in patients' characteristics such as age, gender, body mass index and the American Society of Anesthesiologist score between two groups. Pathologic results of two groups such as histology, tumor size, location of tumor, depth of invasion and number of retrieved lymph nodes were not statistically significant as shown in Table 2. Only lymph node metastasis showed statistical difference, however tumor stage based on 7th American Joint Committee on Cancer Classification was not statistically significant.
The mean operation time of intracorporeal gastroduodenostomy group was 185.6 minutes compared to 192.4 minutes in intracorporeal gastrojejunostomy group. The estimated blood loss was 101 ml in intracorporeal gastroduodenostomy group and 72 ml in intracorporeal gastrojejunostomy group. Significantly more staplers were used for gastroduodenostomy than for gastrojejunostomy. The mean number of staplers used was 6 with a range of 5 to 8 in intracorporeal gastroduodenostomy group while it was 5 with a range of 5 to 7 in intracorporeal gastrojejunostomy group (Table 3).
There were no intraoperative complications related to anastomosis. In terms of postoperative complication, one patient who received intracorporeal gastroduodenostomy experienced melena after the operation which resolved spontaneously. There were 3 patients who experienced postoperative complications after intracorporeal gastrojejunostomy, 1 patient with wound abscess and 2 patients with postoperative atelectasis. Regarding the inflammatory response, the level of high sensitivity C-reactive protein and white blood cell count were not different between the two groups and the patterns of those were similar during the postoperative period. The changes of high sensitivity C-reactive protein and white blood cell count during perioperative period showed similar patterns (Fig. 3). The mean length of hospital stays after the operation was 5.5 days in intracorporeal gastroduodenostomy group and 5.7 days in intracorporeal gastrojejunostomy group without statistical difference (Table 3).
In this comparative study, postoperative outcomes after intracorporeal anastomosis were comparable between gastroduodenostomy and gastrojejunostomy, except that more staplers were used for gastroduodenostomy than for gastrojejunostomy. No intraoperative problems related to anastomosis procedure were observed. Postoperative complications in intracorporeal anastomosis using linear staplers were acceptable. Furthermore, complication related to anastomosis was only one conservatively managed intraluminal bleeding in gastroduodenostomy group.
In the initial period of laparoscopic surgery for gastric cancer, most of surgeons preferred extracorporeal anastomosis regardless of its type because extracorporeal anastomosis was more familiar and technically easy. However, mini-laparotomy incision is needed to perform extracorporeal anastomosis. Mini-laparotomy could cause difficulties in anastomosis due to limited view and working space which could lead to unnecessary injuries to structures around anastomosis.(3) Thus, extracorporeal anastomosis is not well fit for the concept of minimally invasive surgery. Recently, several reports of safety and feasibility of laparoscopic gastrectomy with intracorporeal anastomosis were introduced.(3-5,9) With technical advances in minimally invasive surgery, laparoscopic distal gastrectomy with intracorporeal anastomosis using linear stapler is likely to become more popular recently. In laparoscopic gastrectomy with intracorporeal anastomosis, anastomosis is performed with better view of the field and whole procedure can be observed, thus anastomosis can be done more safely and unnecessary manipulation of surrounded structures can be avoided. Surgical wound of intracorporeal anastomosis may result in better cosmetic outcomes because specimens can be retrieved through a smaller incision than the mini-laparotomy for extracorporeal anastomosis.
For intracorporeal anastomosis, localization of tumor during surgery is utmost important. Unlike in extracorporeal anastomosis, surgeons cannot localize the tumor with their hands. As reported in other studies, preoperative endoscopic clipping or tattooing and intraoperative ultrasonography may be helpful to localize the tumor. (10) In our series, preoperative endoscopic clipping was done and intraoperative plain x-ray was taken after applying the laparoscopic metallic clip at stomach wall to confirm the location.(8) After identifying the location of tumor, surgeon decided whether to perform gastroduodenostomy or gastrojejunostomy. The proximal margin from the tumor in both type of anastomosis was all sufficient and there was no margin positive result in any of cases.
Another suggested concern for intracorporeal anastomosis was longer operation time. In this study, the operation time was 185.6 minutes for gastroduodenostomy and 192.4 minutes for gastrojejunostomy. These operation times were comparable to that of operation time for extracorporeal anastomosis reported previously. (3,11,12) Theoretically, if surgeons become proficient to perform intracorporeal anastomosis, operation will not be longer than extracorporeal anastomosis. Furthermore, operation time for intracorporeal anastomosis can be shorter than extracorporeal anastomosis, because time for making and closing mini-laparotomy is not needed.
In our institution, laparoscopic gastrectomy with intracorporeal gastrojejunostomy has been performed mostly whereas intracorporeal gastroduodenostomy has been recently adopted. It has been suggested that gastrojejunostomy was associated with higher rate of complications and also higher risk of remnant cancer in the long-term.(13,14) However, gastroduodenostomy cannot be done if there is tension on the anastomosis. As shown in this study, postoperative outcomes were not different between gastroduodenostomy and gastrojejunostomy. Therefore, surgeon can choose any type of anastomosis when it is oncologically safe and technically feasible.
As far as we know, this study is the first report to compare the surgical outcomes of intracorporeal gastroduodenostomy and gastrojejunostomy. Moreover, results in this study was not influenced by differences in surgeons' technique, instrument used, or patient care protocol because all surgical procedures were performed with same anastomotic technique without any modification during a relatively short period of time. However, retrospective nature of analyses and no follow-up data hindered the comprehensive comparison of outcomes related to anastomosis method. Thus more detailed and long-term comparative results such as times spent only for the anastomosis and long-term anastomosis related problems such as stenosis and nutritional sequelae cannot be assessed. Also number of patients included was too small to analyze the difference of leakage rates between two procedures. Considering the limitation of retrospective analysis and small number of cases in this study, further evaluations with large number of cases and well designed prospective randomized study with long-term surgical outcomes would be necessary.
In conclusion, intracorporeal anastomosis during laparoscopic gastrectomy using laparoscopic linear stapler, gastroduodenostomy or gastrojejunostomy, showed comparable and acceptable early postoperative outcomes and they were safe and feasible. Therefore, surgeons may choose any type of anastomosis as long as the tumor-free margins were obtained.
Figures and Tables
 | Fig. 1Intracorpoeal gastroduodenostomy using linear staplers. (A) Intraoperative image showing resection of the duodenum. (B) Resection of the stomach. (C) Creation of entry hole along the edge of the greater of the remnant stomach. (D) Creation of entry hole at medial end of the duodenum. (E) A linear stapler is placed in between the remnant stomach and the duodenum and fired. (F) First firing of a linear stapler to close the common entry hole. (G) Second firing of a linear stapler to close the common entry hole. (H) Stapler line of anastomosis aft er reconstruction. |
 | Fig. 2Intracorporeal gastrojejunostomy using linear staplers. (A) Intraoperative image showing resection of the duodenum. (B) Resection of the stomach and stapler line of artificial lesser curvature. (C) Creation of entry hole on the antimesenteric border of the jejunum. (D) Creation of entry hole on the greater curvature side of the remnant stomach. (E) A linear stapler is placed in between the remnant stomach and the jejunum. (F) Closure of the common entry hole using a linear stapler. (G) Anterior stapler line of the anastomosis. (H) Posterior stapler line of the anastomosis. |
 | Fig. 3(A) Changes of high sensitivity C-reactive protein aft er laparoscopic distal gastrectomy with intracorporeal gastroduodenostomy or gastrojejunostomy. There was no statistical diff erence between the anastomosis methods (Mixed model analysis, P=0.501). (B) Changes of white blood cell count aft er laparoscopic distal gastrectomy with intracorporeal gastroduodenostomy or gastrojejunostomy. There was no statistical diff erence between the anastomosis methods (Mixed model analysis, P=0.864). Preop = preoperative; postop = postoperative; POD = postoperative day. |
Acknowledgments
This work was supported by a grant of the Korea Healthcare technology R&D project, Ministry of Health, Welfare, & Family Affairs, Republic of Korea (1020410).
References
1. Jeong O, Park YK. Clinicopathological features and surgical treatment of gastric cancer in South Korea: the results of 2009 nationwide survey on surgically treated gastric cancer patients. J Gastric Cancer. 2011. 11:69–77.

2. Hyung WJ, Kim SS, Choi WH, Cheong JH, Choi SH, Kim CB, et al. Changes in treatment outcomes of gastric cancer surgery over 45 years at a single institution. Yonsei Med J. 2008. 49:409–415.

3. Song KY, Park CH, Kang HC, Kim JJ, Park SM, Jun KH, et al. Is totally laparoscopic gastrectomy less invasive than laparoscopy-assisted gastrectomy?: prospective, multicenter study. J Gastrointest Surg. 2008. 12:1015–1021.

4. Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe H, Katayama T, et al. Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg. 2002. 195:284–287.

5. Kanaya S, Kawamura Y, Kawada H, Iwasaki H, Gomi T, Satoh S, et al. The delta-shaped anastomosis in laparoscopic distal gastrectomy: analysis of the initial 100 consecutive procedures of intracorporeal gastroduodenostomy. Gastric Cancer. 2011. 14:365–371.

6. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma - 2nd English edition -. Gastric Cancer. 1998. 1:10–24.
7. Hyung WJ, Song C, Cheong JH, Choi SH, Noh SH. Factors influencing operation time of laparoscopy-assisted distal subtotal gastrectomy: analysis of consecutive 100 initial cases. Eur J Surg Oncol. 2007. 33:314–319.

8. Kim HI, Hyung WJ, Lee CR, Lim JS, An JY, Cheong JH, et al. Intraoperative portable abdominal radiograph for tumor localization: a simple and accurate method for laparoscopic gastrectomy. Surg Endosc. 2011. 25:958–963.

9. Lee SW, Bouras G, Nomura E, Yoshinaka R, Tokuhara T, Nitta T, et al. Intracorporeal stapled anastomosis following laparoscopic segmental gastrectomy for gastric cancer: technical report and surgical outcomes. Surg Endosc. 2010. 24:1774–1780.

10. Hyung WJ, Lim JS, Cheong JH, Kim J, Choi SH, Song SY, et al. Intraoperative tumor localization using laparoscopic ultrasonography in laparoscopic-assisted gastrectomy. Surg Endosc. 2005. 19:1353–1357.

11. Lee HJ, Kim HH, Kim MC, Ryu SY, Kim W, Song KY, et al. Korean Laparoscopic Gastrointestinal Surgery Study Group. The impact of a high body mass index on laparoscopy assisted gastrectomy for gastric cancer. Surg Endosc. 2009. 23:2473–2479.

12. Song KY, Kim SN, Park CH. Laparoscopy-assisted distal gastrectomy with D2 lymph node dissection for gastric cancer: technical and oncologic aspects. Surg Endosc. 2008. 22:655–659.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download