This article has been corrected. See " Erratum to: Clinical Outcomes of Gastrectomy after Incomplete EMR/ESD" in Volume 11 on page 248.
This article has been corrected. See "Erratum to: Clinical Outcomes of Gastrectomy after Incomplete EMR/ESD" in Volume 12 on page 53.
Abstract
Purpose
Endoscopic resection is widely accepted as standard treatment for early gastric cancer (EGC) without lymph node metastasis. The procedure is minimally invasive, safe, and convenient. However, surgery is sometimes needed after endoscopic mucosal resection/endoscopic submucosal dissection endoscopic mucosal resection (EMR)/endoscopic submucosal dissection (ESD) due to perforation, bleeding, or incomplete resection. We evaluated the role of surgery after incomplete resection.
Materials and Methods
We retrospectively studied 29 patients with gastric cancer who underwent a gastrectomy after incomplete EMR/ESD from 2006 to 2010 at Korea University Hospital.
Results
There were 13 incomplete resection cases, seven bleeding cases, three metachronous lesion cases, three recurrence cases, two perforation cases, and one lymphatic invasion case. Among the incomplete resection cases, a positive vertical margin was found in 10, a positive lateral margin in two, and a positive vertical and lateral margin in one case. Most cases (9/13) were diagnosed as mucosal tumors by endoscopic ultrasonography, but only three cases were confirmed as mucosal tumors on final pathology. The positive residual tumor rate was two of 13. The lymph node metastasis rate was three of 13. All lymph node metastasis cases were submucosal tumors with positive lymphatic invasion and no residual tumor in the gastrectomy specimen. No cases of recurrence were observed after curative resection.
Early gastric cancer (EGC) is defined as a neoplasm confined to the mucosa or submucosa, regardless of regional lymph node metastasis.(1) EGC without evidence of nodal metastasis is treated by endoscopic resection, either endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD). The endoscopic method is widely accepted because it is less invasive and less costly and requires a shorter hospital stay than surgical resection.(2-4)
Guidelines for EMR/ESD, established by the Japanese Gastric Cancer Association, are generally accepted and state that: 1) elevated EGCs less than 2 cm in diameter and 2) small (≤1 cm) depressed EGCs without ulceration are indications for EMR/ESD. At the same time, these lesions must be differentiated adenocarcinoma confined to the mucosa with no lymphatic or vascular involvement.(5)
The so-called extended criteria have been proposed to include: 1) mucosal cancers without ulceration regardless of lesion size, 2) ulcerated mucosal cancers with a size restriction of 30 mm, and 3) cancers with minute submucosal invasion (<500 µm) with a size restriction of 30 mm. Lesions with undifferentiated histology and lymphatic or vascular invasion are still excluded.(6,7)
Although endoscopic resection has the advantage of preserving most of the stomach and maintaining quality of life, some EMR/ESD patients have incomplete resections.(8) In addition, EMR/ESD is associated with a complication frequency, particularly perforation and post-operative bleeding (delayed bleeding).(9) The risk of synchronous and metachronous gastric cancer developing in the patient after endoscopic resection has also become a major problem. (10) Incomplete resection patients are treated empirically, by either gastrectomy, additional endoscopic treatment, or careful follow-up. (11)
We conducted this study to evaluate clinical outcomes and the role of surgery for patients with incomplete resection after EMR/ESD.
We retrospectively evaluated 510 gastric cancer patients who underwent EMR/ESD for gastric neoplasm at Korea University Hospital from 2006 to 2010. From these patients, 482 patients with diagnosed gastric cancer were identified. We studied 29 gastric cancer patients who underwent gastrectomy following EMR/ESD.
Incomplete resection was the most common cause of gastrectomy (13 of 29 cases) following EMR/ESD. Thirteen patients who underwent gastrectomy after incomplete EMR/ESD was enrolled in the study. Indications for EMR in our hospital encompassed the extended criteria including mucosal cancers without ulceration regardless of lesion size, ulcerated mucosal cancers with a size restriction of 30 mm, and cancers with minute submucosal invasion with a size restriction of 30 mm.
The EMR/ESD specimen was examined histopathologically. Resected specimens were systematically sectioned at 2-mm intervals, centered on the part of the lesion closest to the margin and the site of deepest invasion. Incomplete resection was classified as a positive lateral margin, a positive vertical margin and both positive lateral and vertical margin.
The reasons for gastrectomy after EMR/ESD are shown in Table 1. There was bleeding in 7 cases, metachronous lesion in 3 cases, recurrence in 3 cases, perforation in 2 cases, and lymphatic invasion 1 in case. Curative resection was performed in all patients. The surgeries performed were subtotal gastrectomy, B-I & B-II and total gastrectomy with Roux-en-Y esophagojejunostomy.
Characteristics of the patients and the gastric lesions in incomplete cases (n=13). Of the 13 patients, 7 were male and 6 were female. The mean age of the patients was 63.1±7.7 years. There were 8 cases with lesion size greater than 2 cm.
After surgery, the depth of invasion was at the mucosa level in 3 cases, at the submucosal level in 9 cases, and to the muscle in 1 case. Three cases had LN metastases and 1 case was stage N3.
In the final pathology, 8 cases (61.6%) were diagnosed as well or moderately differentiated adenocarcinoma. Four cases were poorly differentiated, and 1 case was diagnosed as signet ring cell carcinoma. The most common type of operation was subtotal gastrectomy with Billroth I anastomosis (Table 2).
9 of 13 cases were diagnosed as mucosal tumors on endoscopic ultrasonography (EUS) but only 3 cases were confirmed as mucosal tumors on final pathology.
Three cases were diagnosed as tubular adenoma on endoscopy, with 1 case well differentiated and 2 cases moderately differentiated. Four cases were diagnosed as well differentiated on EMR/ESD with 1 case revised to moderately differentiated on final pathology (Table 3).
We analyzed the relationship between positive margins with residual tumors and lymph node metastasis. Positive residual tumor was present in 2 of 13 positive margin cases.
There was 1 case with lymph node metastasis in the positive lateral margin and 2 cases in the positive vertical margin (Table 4).
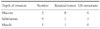
We also analyzed the relationship between depth of invasion with residual tumor and lymph node metastasis. One case with residual tumor had submucosal invasion and the other case had muscle invasion. All lymph node metastasis cases were submucosal tumors (Table 5).
There were 3 cases of LN metastasis. The sizes were 1.5, 1.6, and 2.2 cm.
The histological results were moderately differentiated for case 1, and poorly differentiated in cases 2 and 3. All cases had submucosal invasion. The number of LN metastases were 7, 2, and 1.
Cases 1 and 3 had lymphatic invasions and no cases had vascular or neural invasions (Table 6).
The role of surgery after incomplete EMR/ESD was has been previously reported.
Song et al.(12) reported that gastrectomy with lymph node dissection should be performed in patients with submucosal invasion with or without margin involvement after EMR.
Nagano et al.(13) reported that patients with submucosal invasion or a positive vertical margin should undergo gastrectomy and lymph node dissection.
At first, we expected that if the margin was positive, there'll be residual tumor. But, the results were different. In our study, the positive residual tumor rate was only 15.4% (2 of 13) in positive lateral and/or vertical margin cases. 84.6% (11 of 13) had no residual tumor despite positive margins. In the case that had both the lateral and vertical margins positive, there was no lymph node metastasis.
In a recent study, Chang et al.(14) reported that in lesions invading the lateral margin, the possibility of residual cancer was low. This may be because the EMR/ESD specimen was not fully evaluated histologically. In addition, EMR/ESD is performed using a coagulating device which means that there might not be cells within the margin of the coagulated tissue.
With regard to the depth of invasion, the presence of residual tumor was associated with submucosal and muscle invasion. In particular, the muscle invasion case required EMR with piecemeal dissection.
All lymph node metastasis cases were associated with submucosal tumor. There was no lymph node metastasis in tumors confined to the mucosa.
These results suggest that the depth of invasion deserves greater consideration than positive margin status as an indication for surgery after incomplete EMR/ESD.
Recently there have been a few report regarding extended criteria for EMR/ESD, it is significant especially regarding the application of extended criteria its presence.
The indications for EMR/ESD in our hospital used the extended criteria. There are some concerns regarding the application of extended criteria for EMR/ESD.
Existing methods for preoperative detection of lymph node metastasis are not sufficiently accurate. The only reliable diagnostic method for lymph node metastasis is pathological examination after lymph node dissection.(15,16) Therefore, EMR/ESD may miss lymph node metastases.(17) Our study showed lymph node metastasis in 3 of 13 (23.1%) cases that met the extended indication criteria.
Ishikawa et al.(18) reported the relationship between lymph node metastasis and the tumor depth of wall invasion. When the depth of invasion was submucosal (<500 µm), 2/15 (13%) of EGC differentiated type without ulcer had lymph node metastasis. The authors suggested that indications for EMR/ESD should be limited to mucosal tumors. In our study, all lymph node metastasis cases were submucosal tumors. Extending the indications for EMR/ESD remains controversial, and the applicability of the extended criteria should be further evaluated.
The invasion of tumor can be assessed by performing EUS. The accuracy of EUS for gastric cancer from different authors ranges from 64.8%(19) to 92%(20) in T staging and 50%(21) to 90%(22) in N staging. Currently, EUS is the most reliable method in T and N staging of gastric cancer with high accuracy rates.(23)
In our results, 9 of 13 cases were diagnosed as mucosal tumors on EUS but only 3 cases were confirmed as mucosal tumors on final pathology. More accurate pretreatment staging by EUS should be undertaken for proper stage-dependent patient management.
In conclusion, the gastrectomy is needed for patients with incomplete resection after EMR/ESD, because of the risk of both residual tumor and lymph node metastasis. Precise T staging is essential to avoid unnecessary procedures.
Figures and Tables
References
1. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma - 2nd English edition -. Gastric Cancer. 1998. 1:10–24.
2. Ono H, Kondo H, Gotoda T, Shirao K, Yamaguchi H, Saito D, et al. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001. 48:225–229.

3. Okamura T, Tsujitani S, Korenaga D, Haraguchi M, Baba H, Hiramoto Y, et al. Lymphadenectomy for cure in patients with early gastric cancer and lymph node metastasis. Am J Surg. 1988. 155:476–480.

4. Sue-Ling HM, Martin I, Griffith J, Ward DC, Quirke P, Dixon MF, et al. Early gastric cancer: 46 cases treated in one surgical department. Gut. 1992. 33:1318–1322.

6. Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000. 3:219–225.

7. Soetikno R, Kaltenbach T, Yeh R, Gotoda T. Endoscopic mucosal resection for early cancers of the upper gastrointestinal tract. J Clin Oncol. 2005. 23:4490–4498.

8. Korenaga D, Orita H, Maekawa S, Maruoka A, Sakai K, Ikeda T, et al. Pathological appearance of the stomach after endoscopic mucosal resection for early gastric cancer. Br J Surg. 1997. 84:1563–1566.

9. Tsunada S, Ogata S, Ohyama T, Ootani H, Oda K, Kikkawa A, et al. Endoscopic closure of perforations caused by EMR in the stomach by application of metallic clips. Gastrointest Endosc. 2003. 57:948–951.

10. Nakajima T, Oda I, Gotoda T, Hamanaka H, Eguchi T, Yokoi C, et al. Metachronous gastric cancers after endoscopic resection: how effective is annual endoscopic surveillance? Gastric Cancer. 2006. 9:93–98.

11. Takekoshi T, Fujii A, Takagi K, Baba Y, Kato Y, Yanaghisawa A. The indication for endoscopic double snare polypectomy of gastric lesions (in Japanese with English abstract). Stomach and Intestine. 1988. 23:387–398.
12. Song KY, Hyung WJ, Kim HH, Han SU, Cho GS, Ryu SW, et al. Is gastrectomy mandatory for all residual or recurrent gastric cancer following endoscopic resection? A large-scale Korean multi-center study. J Surg Oncol. 2008. 98:6–10.

13. Nagano H, Ohyama S, Fukunaga T, Seto Y, Fujisaki J, Yamaguchi T, et al. Indications for gastrectomy after incomplete EMR for early gastric cancer. Gastric Cancer. 2005. 8:149–154.

14. Chang JH, Lee IS, You CR, Nam KW, Kwon JH, Suh JP, et al. Re-endoscopic mucosal resection for a residual or locally recurrent gastric lesion after endoscopic mucosal resection. Korean J Gastrointest Endosc. 2007. 35:6–13.
15. Rösch T. Endosonographic staging of gastric cancer: a review of literature results. Gastrointest Endosc Clin N Am. 1995. 5:549–557.

16. Polkowski M, Palucki J, Wronska E, Szawlowski A, Nasierowska-Guttmejer A, Butruk E. Endosonography versus helical computed tomography for locoregional staging of gastric cancer. Endoscopy. 2004. 36:617–623.

17. Jee YS, Hwang SH, Rao J, Park DJ, Kim HH, Lee HJ, et al. Safety of extended endoscopic mucosal resection and endoscopic submucosal dissection following the Japanese Gastric Cancer Association treatment guidelines. Br J Surg. 2009. 96:1157–1161.

18. Ishikawa S, Togashi A, Inoue M, Honda S, Nozawa F, Toyama E, et al. Indications for EMR/ESD in cases of early gastric cancer: relationship between histological type, depth of wall invasion, and lymph node metastasis. Gastric Cancer. 2007. 10:35–38.

19. Yanai H, Matsumoto Y, Harada T, Nishiaki M, Tokiyama H, Shigemitsu T, et al. Endoscopic ultrasonography and endoscopy for staging depth of invasion in early gastric cancer: a pilot study. Gastrointest Endosc. 1997. 46:212–216.

20. Botet JF, Lightdale CJ, Zauber AG, Gerdes H, Winawer SJ, Urmacher C, et al. Preoperative staging of gastric cancer: comparison of endoscopic US and dynamic CT. Radiology. 1991. 181:426–432.

21. Akahoshi K, Misawa T, Fujishima H, Chijiiwa Y, Maruoka A, Ohkubo A, et al. Preoperative evaluation of gastric cancer by endoscopic ultrasound. Gut. 1991. 32:479–482.

22. Habermann CR, Weiss F, Riecken R, Honarpisheh H, Bohnacker S, Staedtler C, et al. Preoperative staging of gastric adenocarcinoma: comparison of helical CT and endoscopic US. Radiology. 2004. 230:465–471.

23. Nakamura T, Tajika M, Kawai H, Yokoi T, Yatabe Y, Nakamura S, et al. Is endoscopic ultrasonography (EUS) needed for deciding the indication for endoscopic submucosal dissection (ESD) of early gastric carcinoma? The significance of diagnosis of the invasive depth and lymph node metastasis of gastric carcinoma by EUS. Stomach and intestine. 2005. 40:465–467.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download