Abstract
Purpose
There is controversy over the treatment for low grade dysplasia, while resection is recommended for high grade dysplasia. But the concordance of the grade of dysplasia between pre- and post-resection is low because of sampling errors with endoscopic biopsy. We attempted to establish a clearer direction for the treatment of dysplasia by clarifying the discrepancy between the pre- and post-resection diagnoses.
Materials and Methods
We performed a retrospective review of 126 patients who had undergone resection with the diagnosis of dysplasia on biopsy at Bundang CHA Hospital from 1999 to 2009.
Results
Seventy patients were diagnosed with low grade dysplasia and 56 patients were diagnosed with high grade dysplasia. Among the 33 patients who received gastrectomy with lymph node dissection, 30 patients were revealed to have invasive cancers and 4 patients showed lymph node metastasis. Discordance between the diagnoses from biopsy and resection occurred in 55 patients (44%). There was no correlation on the comparative analysis between the size, location or gross type of lesion and the grade of dysplasia.
Conclusions
The rate of discordance between the diagnoses of endoscopic biopsy and the post resection pathologic report was as high as 44%. Endoscopic mucosal resection was not sufficient for some patients who were diagnosed with dysplasia on biopsy due to the presence of lymph node metastasis. It is necessary to be prudent when determining the follow-up and treatment based solely on the result of the biopsy.
Atrophic gastritis, intestinal metaplasia and gastric epithelial dysplasia are the precancerous lesions of gastric cancer.(1,2) Dysplasia histologically shows atypical and abnormal cell differentiation and altered glandular structures. As the histological category of dysplasia becomes higher, the incidence of gastric adenocarcinoma is also increased.(3) In low category dysplasia as examined under a microscope, relatively even tubular glandular structures proliferate, and structural alteration of the glandular epithelium rarely occurs. Nonetheless, the change of the size of the nucleus and alterations of it are observed: the elongated nucleus is densely arranged, and the nucleolus is detected in various sites. Cell division is occasionally observed, but the polymorphism or pachychromatic nucleus is not clear. In high category dysplasia, the alteration of the size and shape of glandular structures is severe and thus there are associated structural abnormalities, and due to the pachychomatic nature of the nucleomicrossomes, the nucleus is located in the apex of the epithelial cells, and cell division is increased. As the cells of the glandular structure become a single layer, the size and shape of the nucleus becomes diverse, and the change to carcinoma in situ is observed as being pachychromatic and the loss of polarity. When such cells infiltrate to the lamina propria, this is diagnosed as intramucosal adenocarcinoma.(4) A high histological discrepancy of gastric dysplasia as assessed by biopsy and as assessed by the tissues obtained by resection has been reported, and since the prospective studies on the natural course of these lesions are not sufficient, it is difficult to establish a treatment policy. It is agreed that resection is required for high grade dysplasia; however, the treatment policies for low grade dysplasia are controversial. In our study, to help establish treatment protocols for gastric epithelial dysplasia, we retrospectively analyzed the medical record of patients who were diagnosed as having gastric epithelial dysplasia by endoscopic biopsy and underwent resection.
We analyzed the medical record of 126 patients who were diagnosed as category 3 or category 4 by endoscopic biopsy according to the Vienna classification of gastrointestinal epithelial neoplasia on gastrofiberscopic biopsy(4) from 1999 to 2009 at the Bundang CHA Hospital. These patients subsequently underwent polypectomy, endoscopic mucosal resection, submucosal resection or gastrectomy, including lymph node dissection, and the accuracy of the diagnosis prior to and after resection was compared after performing histological re-examination. As references, category 1 is negative for neoplasia/dysplasia, category 2 is indefinite for neoplasia/dysplasia, category 3 is non-invasive low category neoplasia (low grade adenoma/dysplasia), category 4 is non-invasive high grade neoplasia, including high grade adenoma/dysplasia, noninvasive carcinoma (carcinoma in situ) as well as a suspicion of invasive carcinoma, and category 5 is invasive neoplasia, including intramucosal carcinoma and submucosal carcinoma or beyond. The patients who were classified by the previous 3-category system as mild, moderate and severe were re-examined by 2 pathologists and then they were reclassified by the 2-category system as low grade/category 3 or high grade/category 4. Ultimately, the study subjects were the patients who were definitely diagnosed as the low category or the high category of dysplasia.
The correlation of the grade of gastric epithelial dysplasia with the macroscopic findings of the lesion and the lesion's location, and size was analyzed. The size of lesion was analyzed by two methods: the long axis and the area. The area was calculated by multiplying the long axis and the short axis. In addition, the 33 patients diagnosed with invasive cancer after resection were divided in to the early gastric cancer and advanced gastric cancer groups, and the correlation of the macroscopic findings of the lesion according to the depth of invasive and the lesion's location and size was analyzed. Among the 25 patients who underwent surgery, the correlation of the macroscopic findings and the lesion's location and size was analyzed according to the status of lymph node metastasis. The TNM classification of invasive cancers was done according to the UICC classification, 6th edition (2002). The SAS 9.1 program was used for statistical analysis. P-values below 0.05 were considered to be significant.
The age of the 126 patients ranged from 43 years to 90 years, and the mean age was 64.9 years. There were 77 males and 49 females, and the ratio of the males to females was 1.57 : 1. The age and gender according to the category were not different.
Among the total 126 patients, 33 cases received gastrectomy, including lymph node dissection, because they were patients at the early period when endoscopic resection was not performed, their lesion was located in an area where endoscopic resection is difficult and/or they had a high probability of having invasive cancer. The postsurgical results of the 33 patients who underwent surgery were 2 patients of category 3, 6 patients of category 4 and 25 patients of category 5.
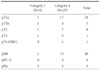
Among the 70 cases diagnosed as category 3 by biopsy, there were 7 cases (10%) whose category was lowered to category 1 or category 2 after surgery, there were 51 cases (73%) whose category prior to resection was identical to that after resection, there were 8 cases (11%) whose category was raised to category 4 and there were 4 cases (6%) whose category was raised to category 5.
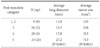
Among the 56 cases diagnosed as category 4 by biopsy, there were 2 cases (9%) whose category was lowered to category 1 or category 2, there were 5 cases (9%) lowered to category 3 (9%), there were 20 cases (36%) that the biopsy and surgical category (category 4) were identical and there were 29 cases (52%) who were raised to category 5. Among the total 126 patients, there were 71 patients (56%) whose biopsy category concurred with the category after resection (Table 1).
The average number of biopsies of the total 126 patients was 4.4. Examining the concurrence rate of the diagnosis according to the number of biopsies, 27 of 45 patients underwent biopsy less than 3 times (60%), 27 of 52 patients underwent biopsy 4 or 5 times, and 17 of 29 patients underwent biopsy more than 6 times (58.6%) and the concurred histopathological results of before resection compared to that after resection showed no statistically difference among the groups.
To compare the accuracy of the diagnosis according to the size of lesion, the concurrence rate of the diagnosis for the 88 patients with lesion smaller than 2 cm and for the 38 patients with the lesion larger than 2 cm was examined. There was concurrence of the diagnosis prior to and after resection for 57 patients with lesion smaller than 2 cm (62%) and 15 patients with lesion larger than 2 cm (39%). For the patients with lesion smaller than 2 cm, the accuracy of the diagnosis was significantly higher (P=0.008).
Among the 126 cases, the 84 cases assessed to be category 3 or category 4 after resection were divided according to the endoscopic findings as elevation, flat and depression, and we compared the categories after resection. It was found that the category of dysplasia did not correlate with the macroscopic findings. The patients were divided according to the location of lesion as upper, middle and lower, and the correlation to the category of dysplasia was compared and analyzed. Similarly, the category of dysplasia did not correlate with the location of lesion (Table 2).
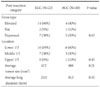
The area and long axis of the lesions of the total 126 cases were obtained, and their correlation to the category after resection was compared and analyzed. For the dysplasia of category 1, category 2, category 3 and category 4, the size was not significantly different. The area and long axis of the category 5 invasive cancer were significantly larger than those of the other categories (Table 3).
To determine the indications for endoscopic resection or surgery, the presurgical clinical findings of the 33 cases diagnosed as category 5 after resection (8 cases by endoscopic resection and 25 cases by surgery) were analyzed. The depth of tumor of the 4 patients diagnosed as category 3 by biopsy after resection was one patient each for T1a, T1b, T2, and T4, respectively. Among them, one patient did not have lymph node metastasis and the other 3 patients' statuses were unknown. Twenty nine patients were diagnosed as category 4 by biopsy. The depth after resections was T1a for 17 patients, T1b for 4 patients, T2 for 7 patients and Tx for one patient. There were 19 patients without lymph node metastasis, 4 patients with lymph node metastasis and 6 patients were Nx, including 1 case that underwent opening and closure (Table 4).
The thirty three category 5 patients after resection were divided into early gastric cancer and advanced gastric cancer. Twenty three patients had early gastric cancer and 10 patients had advanced gastric cancer. After dividing them into early gastric cancer and advanced cancer, the macroscopic findings, the location of lesion, the area and the long axis were compared and analyzed. No differences were detected (Table 5).
Among the 33 patients diagnosed as category 5 after resection, 25 patients underwent surgery and 8 patients underwent endoscopic resection. Among the 25 patients who received surgery, the macroscopic findings of the lesions, the location of the lesions and the size of lesions were analyzed for the 4 patients with lymph node metastasis and the 20 patients without lymph node metastasis, and one patient was NX because of opening and closure. No significant differences were detected.
Gastric epithelial dysplasia is a microscopic term. As a macroscopic finding, it is referred to as adenoma. It occurs more frequently with aging, and atrophic gastric mucosa in the vicinity of a lesion is detected in many cases. Gastric epithelial dysplasia progresses to the intestinal type gastric cancer in many cases.(5) It occurs more frequently in males than in females, and the ratio of the males and females is 2.4~3.9 : 1. The frequency of dysplasia is increased in individuals older than 60 years or in those with severe atrophic gastritis.(6,7)
The 2 category classification system (low category and high category) is currently being used. In the past studies, the 3 stage classification system was used in most cases, and so comparing between older studies and newer studies is difficult. The classification of the 2 category classification system has advantages that it is simple, the reproducibility among investigators is high and it can be applied to other parts of the gastrointestinal tract. In addition, since the difference of the probability to progress to gastric adenocarcinoma between the categories is clear, it is more advantageous for follow up observation or to decide on treatment protocols.(8) As compared with that for low category dysplasia, there is a high probability of high category dysplasia progressing to gastric adenocarcinoma. Degenerative lesions, more advanced or continuous lesions are significantly more abundant in the high category dysplasia as compared with that of low category dysplasia, and high category dysplasia is observed more frequently with aging.(9,10)
In our study when examining the accuracy of biopsy of gastric epithelial dysplasia, the concurrence rate of endoscopic forceps biopsy and the diagnosis after resection was 56%, and the concurrence rate for category 3 lesion was 73%, which did not show a great difference from the results of the previous studies. Nonetheless, the concurrence rate for the category 4 cases was as low as 36%. For the results of other studies, the pathohistological concurrence rate of the endoscopic mucosal resection and forceps biopsy was 65~75%, which was not high.(11,12) According to a study conducted in Korea,(13) in the total 434 cases, the diagnosis was changed after endoscopic submucosal resection for 253 patients (58.3%). Therefore, for the cases diagnosed as dysplasia by biopsy, attention should be paid when deciding the treatments. In our cases, similarly, 7 patients (10%) whose lesions were diagnosed as low category dysplasia by biopsy were diagnosed as being negative for dysplasia after resection. It is controversial whether to consider the cases whose lesions can not be detected anymore during the follow-up observation as degenerative changes or regenerative epithelial changes due to repeated biopsies. It is difficult to clearly explain the result that the concurrence rate of the diagnosis prior to and after resection was high for lesions smaller than 2 cm. Nonetheless, it should be kept in mind that as the size of lesion becomes larger, the diagnostic accuracy becomes lower.
According to a study conducted in Korea,(14) 17.1% of the high category dysplasia cases and 7.8% of the low category dysplasia cases were diagnosed as gastric adenocarcinoma after resection. In the study reported by Kim et al.,(15) it has been also reported that 54% of the cases of high category dysplasia were diagnosed as gastric adenocarcinoma, and similarly for the low category dysplasia, 17.6% of the cases were diagnosed as gastric adenocarcinoma, and the authors stated the necessity of an accurate diagnosis via aggressive resection even for the low category dysplasia cases.
In our cases, similarly, when comparing and analyzing by an identical method, it was found that even for the low category dysplasia lesions diagnosed by biopsy, 6% of the cases were diagnosed as invasive cancer after resection. For the high category dysplasia, the percent of cases diagnosed as invasive cancer after resection reached 52%. Even considering that our study was a retrospective study, the result that more than half of the cases of high category dysplasia were diagnosed as invasive cancer should not be overlooked.
According to the grade of dysplasia, the shape, location and size and were compared. It was found that the macroscopic findings or location was not significant, and differences were detected only according to size. On the comparison of low grade and high grade dysplasia, the lesion size of the category 5 invasive cancer was significantly larger. In another Korean study,(16) it was reported that as the dysplasia grade became severer, the size of lesion was significantly increased. In our study, the sizes of the category 3 and 4 lesions were not different, and so it is difficult to guess the category of dysplasia based on the size only prior to resection. For the comparison of the size of lesion, this was analyzed by two methods by using the area and the length of the long axis. Nonetheless, the results were not different, and so it is thought that the analysis of the size of lesion by using only the long axis is adequate. It may be considered that the possibility of the lesion with a long axis larger than 27 mm being category 5 is high. Nonetheless, from the point of view of clinicians, since the indication for resection is category 4 and 5 lesions, for making the diagnosis of dysplasia by biopsy, it is difficult to determine the indication for resection based on only the lesion size. For the category 5 lesions, the area and the long axis were significantly different, which is thought that although they were either low category or high category dysplasia on biopsy, the cases whose endoscopic results were suspicious for invasive cancer were included, and the overall endoscopic impression could be an important guideline to predict the presence of invasive cancer.
Thirty three patients diagnosed as having invasive cancer after resection were classified as having early gastric cancer or advanced gastric cancer, and the lesions were analyzed by dividing the macroscopic findings, the location and the size according to the depth of invasion, and any differences were not detected. Therefore, it was impossible to distinguish the patients diagnosed as having dysplasia by biopsy as having early gastric cancer or advanced gastric cancer in advance by the endoscopic findings only. In addition, to determine the patients who have the possibility of lymph node metastasis, among the 33 patients diagnosed as having invasive cancer after resection, for the 25 patients who underwent surgery, the endoscopic macroscopic findings as well as the location and size of the lesions of the patients with lymph node metastasis were compared with that of the patient without lymph node metastasis, and significant differences were not detected. Nonetheless, similar to the 4 patients with lymph node metastasis, some cases were diagnosed as gastric cancer based on the endoscopic findings, but the results of several times biopsies were dysplasia, and so attention must be paid to this.
Our results show that even for patients diagnosed as having low grade dysplasia by biopsy, 17% were high grade dysplasia cases or cases associated with invasive cancer and for such cases, instead of the follow-up observation or repeated biopsy, endoscopic resection of the mucosa, including the entire lesion, is required. In addition, depending on the clinical findings, the possibility of invasive cancer should always be kept in mind. In our study, for the cases diagnosed as having high grade dysplasia by biopsy, 52% were diagnosed as invasive cancer after resection. Among them, 10 cases were advanced cancer, and early gastric cancer and advanced cancer could not be distinguished in advance based on the macroscopic findings of the lesions, the area and the long axis. In conclusion, even for the patients with low category dysplasia, a substantial number of patients were associated with invasive cancer, and the factors increasing the possibility of invasive cancer are the grade of dysplasia at the time of biopsy, the size of the lesion and suspicious endoscopic results for cancer. Low grade dysplasia and high grade dysplasia could not be differentiated by the other clinical findings, and it is also difficult to assess the presence of lymph node metastasis or to distinguish early gastric cancer from advanced cancer. Therefore, not only for the high grade dysplasia cases, but also for the low grade dysplasia cases, the possibility of invasive cancer, infiltration to the submucosal layer and lymph node metastasis should be considered. In addition, it is thought to be preferable to perform endoscopic resection rather than repeated biopsy, and to perform additional surgery if it is required.
The result of our study shows that the concurrence rate of the diagnosis by biopsy and after resection was 56%, and so the accuracy of biopsy was not high. Therefore, it is not desirable to perform follow-up observation based on the results of biopsy only, and the endoscopic results together with the biopsy results are of help to reduce biopsy errors. It is desirable to perform minimal endoscopic resection not only for high grade dysplasia, but also for low category dysplasia rather than just follow-up observation or repeated biopsy, and to add surgery if required, depending on the resection results.
References
1. Ming SC, Bajtai A, Correa P, Elster K, Jarvi OH, Munoz N, et al. Gastric dysplasia. Significance and pathologic criteria. Cancer. 1984. 54:1794–1801.

2. Morson BC, Sobin LH, Grundmann E, Johansen A, Nagayo T, Serck-Hanssen A. Precancerous conditions and epithelial dysplasia in the stomach. J Clin Pathol. 1980. 33:711–721.

3. Ghandur-Mnaymneh L, Paz J, Roldan E, Cassady J. Dysplasia of nonmetaplastic gastric mucosa. A proposal for its classification and its possible relationship to diffuse-type gastric carcinoma. Am J Surg Pathol. 1988. 12:96–114.
4. Schlemper RJ, Riddell RH, Kato Y, Borchard F, Cooper HS, Dawsey SM, et al. The Vienna classification of gastrointestinal epithelial neoplasia. Gut. 2000. 47:251–255.

6. You WC, Blot WJ, Li JY, Chang YS, Jin ML, Kneller R, et al. Precancerous gastric lesions in a population at high risk of stomach cancer. Cancer Res. 1993. 53:1317–1321.
7. Tosi P, Filipe MI, Luzi P, Miracco C, Santopietro R, Lio R, et al. Gastric intestinal metaplasia type III cases are classified as low-category dysplasia on the basis of morphometry. J Pathol. 1993. 169:73–78.

8. Choi JY, Lee SH. Therapeutic strategy and clinicopathologic analysis of gastric epithelial dysplasia. J Korean Surg Soc. 2004. 67:192–197.
9. Farinati F, Rugge M, Di Mario F, Valiante F, Baffa R. Early and advanced gastric cancer in the follow-up of moderate and severe gastric dysplasia patients. A prospective study. I.G.G.E.D.--Interdisciplinary Group on Gastric Epithelial Dysplasia. Endoscopy. 1993. 25:261–264.

10. Bearzi I, Brancorsini D, Santinelli A, Rezai B, Mannello B, Ranaldi R. Gastric dysplasia: a ten-year follow-up study. Pathol Res Pract. 1994. 190:61–68.
11. Hansson LE, Lindgren A, Nyrén O. Can endoscopic biopsy specimens be used for reliable Laurén classification of gastric cancer? Scand J Gastroenterol. 1996. 31:711–715.

12. Palli D, Bianchi S, Cipriani F, Duca P, Amorosi A, Avellini C, et al. Reproducibility of histologic classification of gastric cancer. Br J Cancer. 1991. 63:765–768.

13. Kim YD, Cho JY, Jung IS, Koh BM, Hong SJ, Ryu CB, et al. Comparison of endoscopic forcep biopsy and the histopathologic diagnosis after endoscopic submucosal dissection. Korean J Gastrointest Endosc. 2009. 38:188–192.
14. Hwang JY, Park KS, Hwang JS, Ahn SH, Park SK. Histological comparison of endoscopic forceps biopsy with endoscopic resection in gastric mucosal elevated lesion. Korean J Gastrointest Endosc. 2003. 26:68–72.
15. Kim EY, Kim JJ, Kim B, Park SM. Treatment of gastric epithelial dysplasia that is diagnosed by endoscopic biopsy. J Korean Gastric Cancer Assoc. 2010. 10:1–4.

16. Min JS, Noh SH, Kim HG, Yoo CH, Lee YC. Therapeutic strategy for gastric epithelial dysplasia. Korean J Gastroenterol. 1998. 32:176–183.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download