Abstract
Objectives
The purpose of this survey was to explore physicians' opinions to identify an adequate time range for clinical information to be provided with a referral that would help minimize wasteful retesting.
Methods
In 2011, we conducted a questionnaire survey of 193 physicians. Examining the degree of utilization of provided medical information, we determined the range of clinical information of referral documents.
Results
Less than three months of prescription history and blood sample test results in patient referral was most frequent. Less than one year of image information was most frequent. Most doctors answered there is no need to repeat the same type of blood test in their institute when they had information less than half a month old. Less than half to one month of image information was most frequent. Also, it appeared many doctors think “fundamentally they do not change their mind from their own medical department standpoint.” At the actual site, those who would even review referral clinical notes accounted for about 30% of all participants.
Go to : 
A ‘patient referral document,’ or so-called referral letter, contains clinical information necessary for the patient to continue receiving treatment and is essential for medical collaboration. For the issuing organization, the document also counts toward points for patient referral fees under the medical service remuneration system; therefore, they are frequently exchanged between medical facilities. However, even after many tests have been conducted by a referring hospital and all of the results have been provided, the same tests are often repeated at the recipient hospital [12]. From the perspective of reducing national medical expenses, it is extremely important for physicians to understand how much of the provided clinical information they should handle on their own to determine whether they can forgo performing the same tests. However, to the best of our knowledge, there have been no fact-finding surveys conducted on this topic in Japan or internationally. The purpose of this survey was to explore physicians' opinions to identify an adequate time range for clinical information to be provided with a referral that would help minimize wasteful retesting of a patient.
Go to : 
We conducted a questionnaire survey for the abovementioned purpose. The questionnaire items are shown in a separate document (Appendix 1). The framework of the questionnaire was to ask, “How much of the clinical information provided with a referral by an outside source is actually reviewed by the recipient?” Specifically, in a situation where a patient brings in ‘prescription information,’ ‘laboratory results,’ and ‘radiological images/reports’ with a referral letter in an outpatient setting, respondents were asked “How much of the provided historical information they would review” and “How recent the last tests should be for them to determine that there would be no need for retesting.” Respondents were also instructed to provide their answers in general terms and from the standpoint of their specialized fields. Additionally, with respect to ‘EMR sharing features,’ which are seen in some regional collaboration systems, respondents were asked how much of the shared data they would actually be able to review within the limited time allowed in their outpatient practice.
The questionnaire was conducted with the participation of two groups. Through research projects funded by the Health and Labour Sciences Research Grants of the Ministry of Health, Labour and Welfare, we gained an opportunity to collect data from two samples: ‘relevant persons in hospitals within Shizuoka Prefecture’ by mail and ‘member physicians of Japan Association for Medical Informatics (JAMI)’ through the Internet. We asked the two groups the same questions and collected their responses. The survey was conducted from 2011 to 2012.
(1) Survey subjects: Physicians working at hospitals within Shizuoka Prefecture (all hospitals with 20 beds or more)
(2) Mailing list: A list of addressees was created by searching through the public information available on the Internet, phone book, etc.
(3) Survey method: Distribution/collection by mail
(4) Collection results: Number of questionnaires sent out (n = 183), number of questionnaires collected (n = 107), response rate (58.5%, based on definition RR5 in the American Association for Public Opinion Research [AAPOR] guidelines [3]).
(5) The executing agency and main body of the survey: Department of Medical Informatics, Hamamatsu University Hospital
(6) The main body conducting the survey: TOMS Corporation
(1) Survey subjects: Member physicians of JAMI
(2) Survey method: Online survey
(3) Collection results: Number of requests made (n = 384), number of questionnaires collected (n = 85), response rate (22.1%, the number of healthcare professionals among JAMI's 3,200 members is undisclosed, but was hypothesized to be 12% here—calculated from the percentage of HIS-related staff—based on definition RR3 in the AAPOR guidelines 2).
(4) The executing agency and main body of the survey: Department of Medical Informatics, Hamamatsu University School of Medicine
Go to : 
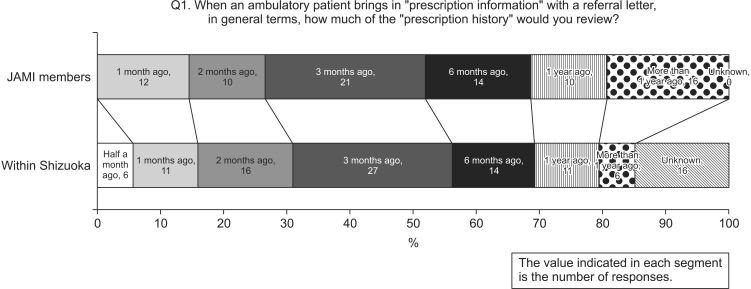
Q1. To the question about how much of the provided historical prescription information they would review, ‘three months ago’ was most frequently selected by both JAMI members and Shizuoka respondents (Figure 1).
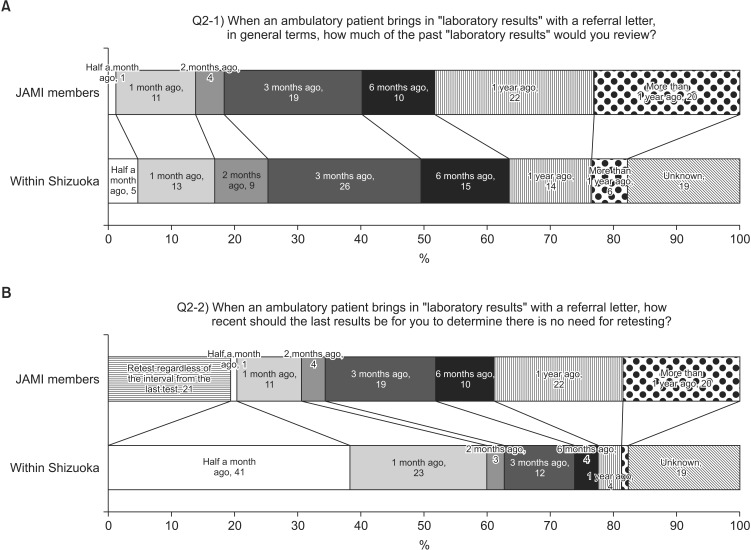
Q2. To the question about how much of the provided historical laboratory results they would review, ‘three months ago’ was most frequently selected by both JAMI members and Shizuoka respondents (Figure 2A). On the other hand, to the question about how recent the provided data should be for them to determine that there would be no need for retesting, the highest percentage of JAMI members selected ‘one year ago,’ but the second most frequently selected answer among them was “retest regardless of the interval from the last test.” The highest percentage of Shizuoka respondents selected ‘six months ago’ (Figure 2B).
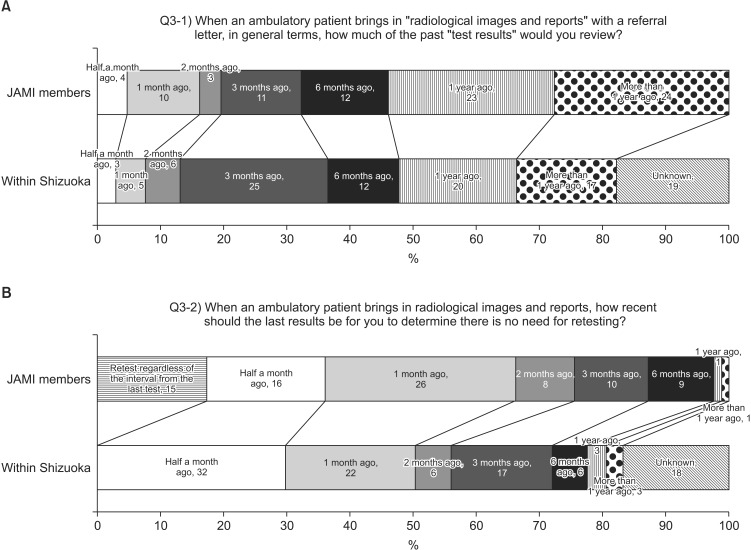
Q3. To the question about how much of the provided historical radiology results they would review, the most frequently selected answer was ‘more than one year ago’ among JAMI members and ‘three months ago’ among Shizuoka respondents (Figure 3A). To the question about how recent the provided data should be for them to determine there would be no need for retesting, the most frequently selected answer was ‘one month ago’ among JAMI members and ‘half a month ago’ among Shizuoka respondents (Figure 3B).
Q5 only asked for the specialized field of the target and was omitted from the analysis.
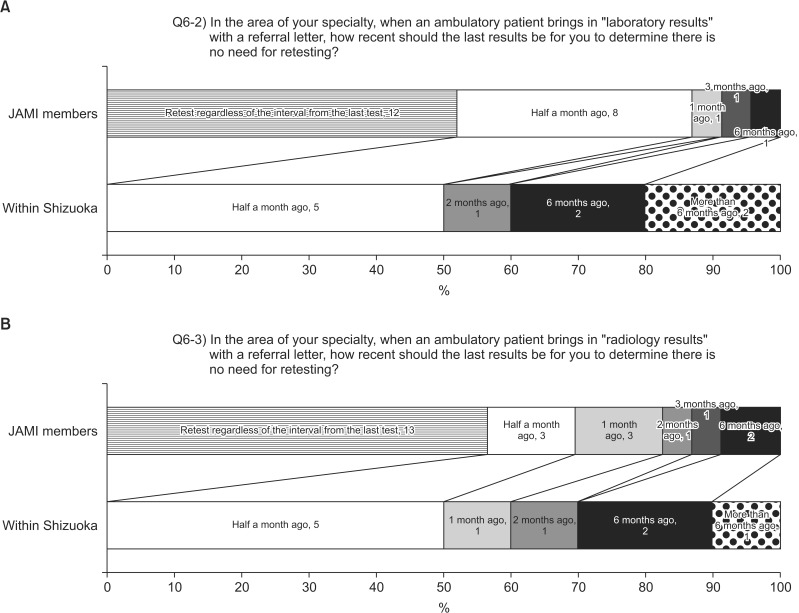
Q6. To the question about whether or not their judgment about the reference periods would be any different from their answers given in general terms, many JAMI members and Shizuoka respondents answered ‘not different’ (JAMI 23 vs. 63; within-Shizuoka 10 vs. 78). To the question about how recent the last laboratory results should be to determine that there would be no need for retesting from the standpoint of specialists, the most frequently selected answer was “retest regardless of the interval from the last test” among JAMI members and ‘half a month ago’ among Shizuoka respondents (Figure 4A). To the question about how recent the last radiology results should be to determine that there would be no need for retesting from the standpoint of specialists, the most frequently selected answer was “retest regardless of the interval from the last test” among JAMI members and ‘half a month ago’ among Shizuoka respondents (Figure 4B).
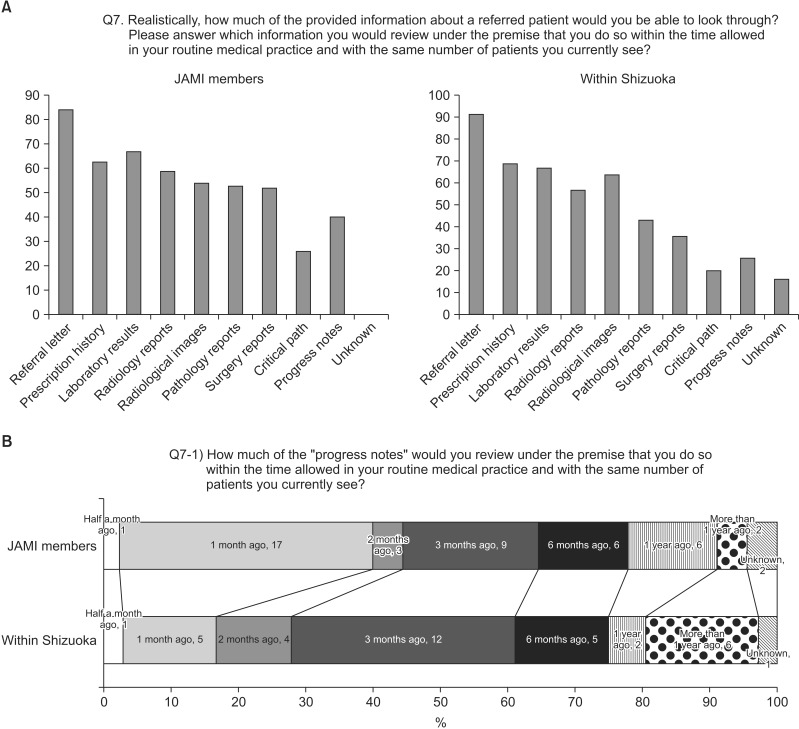
To the question about which information they would review within the time allowed in their medical practice, commonly selected answers among JAMI members were ‘referral letter,’ ‘prescription history,’ ‘laboratory results,’ ‘radiological images,’ and ‘radiology reports.’ About 47% (40 respondents) of all JAMI members and about 24% (26 respondents) of all Shizuoka respondents said they would be able to review ‘progress notes’ (Figure 5A). To the question about how much of the historical progress notes they would actually be able to review within the time allowed in their practice, the most frequently selected answer was ‘one month ago’ among JAMI members and ‘three months ago’ among Shizuoka respondents (Figure 5B).
Go to : 
This questionnaire targeted two groups—one was conducted by mail and had a response rate of 58%, and the other was conducted with a large sample over the Internet and had a response rate of 22%. One group consisted of JAMI members, who were presumably involved in or somewhat familiar with the operations relating to IT systems, while the other group responding to the mail survey comprised relevant persons in hospitals within Shizuoka Prefecture who were likely to be involved in general hospital services.
Some researchers have identified differences in credibility between online and mail surveys, noting that mail survey respondents are inclined to be those who are particularly interested in the survey topic. However, in an online survey, responses can efficiently be obtained from a large sample. In this survey, due to the difference in response rates, credibility of the responses differed greatly between the two groups. In addition to that, respondents' work duties were also different. Therefore, some of their responses may have been biased. This survey was able to be done because there was financial aid to conduct a questionnaire survey with different groups with two profiles at the same time. However, the numbers of parameters or the job types of the targets differed, and this may have affected the survey results. In principle, it would have been legitimate to gather information from a group with a larger number of people and to analyze the trend, so the data collection method of this study might be limited. However, it was very meaningful to investigate the utilization of medical information provided with a referral in terms of the examination result provision period, so we reported this as the first step. Therefore, was is no purpose in choosing different groups with two profiles, but as a hypothesis, we expected that the JAMI group would tend to perform data processing using the information system because the IT skills of JAMI group were expected to be higher, and we found that this expected tendency was true. As the result, regarding “the relation between the provided medical treatment period and utilization situation” which was the essence of this survey, there was not a big difference between the two groups.
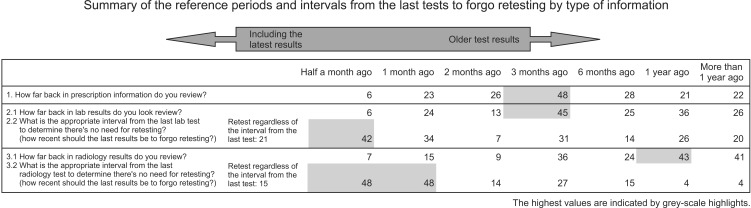
Regarding the adequate reference periods and interval from the last test to forego retesting, we summarized the responses from JAMI members and Shizuoka residents in a table by type of information (Figure 6). In general outpatient services, the most frequently selected answer to the question “How much of the provided information would you review?” was ‘three months ago’ for laboratory results and ‘one year ago’ for radiology results. To the question, “How recent should the results of the last test be for you to determine that there would be no need for retesting?” the highest percentage of respondents selected ‘half a month ago’ for laboratory tests and ‘half to one month ago’ for radiology tests. When the same question was reconsidered from the standpoint of specialists, most physicians said their basic stance was ‘not different,’ but many of those who answered ‘different’ said they would “retest regardless of the interval since the last test.” Regarding how much of the provided historical data they would review, responses slightly varied between different orders; respondents did not review as much past data to check laboratory results and prescription information as they would for radiology results. This may be because clinicians believe that “laboratory results, such as blood glucose levels and white blood cell counts, are good for a shorter period of time than radiology results.” In other words, laboratory results from a long time ago may not even be reviewed, although this may depend on the test item. Regarding the differences between adequate reference periods for test results and the interval from the last test to forgo retesting, respondents would examine significant historical data to review laboratory results and radiology results, but forgo retesting only when they have more recent results. This tendency was pronounced when respondents answered from their specialist point of view. ‘Forgoing retesting’ would be convenient in a sense that recipients can use provided data as their own. Despite that, they would still conduct the same tests, possibly for the following two reasons: (1) test results provided by a referring hospital are or are thought to be less than accurate. This may be truer for radiology tests than laboratory tests. Recipients may want a specific type of data, such as thin-slice data (to construct 3D images, for example), and the provided data may not be sufficient. Sometimes, more detailed data are desired for the purpose of academic research; however, such cases were excluded from consideration in this work. (2) Test results that cannot be used in medical practice at a recipient hospital are meaningless. When clinical data are sent from other hospitals, they may be provided in ‘paper form’ known as referral letters, on a CD-R, or through ‘online registration’ as seen in collaboration systems. When paper data are imported by scanners, there may be times when scanned data, such as blood test results, cannot be used for subsequent treatment at the recipient hospital because they are “illegible,” “cannot be imported into the EMR system,” etc. It appears there is a need for patients' data to be imported as digital data, not scanned images.
Our survey results indicate that doctors cannot regard the referral medical information as a result of their own facility adequately. To evaluate referral medical information in chronological order in their own facility, it is necessary to standardize information capture profiles and data formats. It is necessary to align JLAC10 code (which is standardized laboratory test item classification code in Japan) for laboratory tests, and YJ code or HOT code (which is medicine code master) for prescriptions.
Regarding image-exchange, HE (which is group by healthcare professionals to improve the way computer systems in healthcare share information) provides PDI (Portable Data for Imaging) profiles. PDI profiles are used for reliable interchange of image data and diagnostic reports on CD-R. To use this kind of profile, there must be a unified system between the cooperating institution.
To question Q7, “Realistically, how much of the provided information about a referred patient would you be able to review?,” respondents said they would look through many items, but those who would even review clinical notes accounted for about 30% of all participants (Figure 5A). The intention behind this question was to investigate the ‘interfacility patient data sharing’ used in some EMR systems. The results indicated that many physicians review report-type documents, but only around 30% of them actually checked daily clinical notes; even the physicians who would check clinical notes do not have enough time to examine many past records. Thus, sharing an EMR of a patient with a long clinical history does not mean that the recipient will be able to review all of the data. It is almost impossible to review and remember all information recorded in daily clinical notes, and physicians should not be expected to do so. Although, in such cases, we believe that exemptions are made accordingly through an agreement between facilities, it is still an important issue to consider. Realistically, report-type documents, such as discharge summaries, are considered sufficient to share with other facilities. After all, the adequate range of clinical information to provide with a referral should be determined according to the convenience of the recipient, which is a basic approach to all communication. It is necessary to consider the IT environment and other associated factors in the recipient's facility and predict what additional tasks and inconvenience the data may cause to the recipient. When providing a patient's data, it is important to summarize or omit nonessential information altogether. In some medical facilities, the issues discussed in this paper have been a frequent cause of confusion. Therefore, rather than waiting for the systematization or formulation of clear guidelines, we should put into the consideration when determining how much clinical information to provide with a referral.
In conclusion, patient referrals are carried out through two-way communication. Therefore, when a referring hospital or clinic provides a patient's data, the recipient's workflow and system environment should be taken into consideration.
Go to : 
Acknowledgments
This survey was supported by the following research funded by Health and Labour Sciences Research Grants of Japan Ministry of Health, Labour and Welfare (No. H23-iryoshitei-015, “Research on clinical indicators out of hospital information system data” by Michio Kimura; No. H24-iryoippaniryoippan-027, “Research on the standardization necessary for the use of electronic medical information and measures for its dissemination” by Kazuhiko Ohe). This research dealt with anonymization aggregation processed data items and judged that no appointment is required.
Go to : 
Appendix
Appendix 1
A questionnaire survey on sharing and using clinical information on a referred patienta
Responses to this questionnaire will be statistically processed. Summarized results will be disclosed to the public. The data used in statistical processing will not include any personal information. Individuals cannot be identified from the disclosed summary. If you are willing to participate, please answer the following questions.
Premise: Your answers may differ depending on your department or the disease in which you specialize, but please first answer in general terms.
Q1. When an ambulatory patient brings in “prescription information” with a referral, in general terms, how much of the “prescription history” would you review?
Q2. When an ambulatory patient brings in “laboratory results,” in general terms,
Q3. When an ambulatory patient brings in “radiological images and report” with a referral, in general terms,
Q5. In which disease do you primarily specialize?
Q6-1. If the referred patient had the disease, would any of the above answers given “in general terms” be different?
If you chose “different,” please answer the following questions:
In the area of your specialty, when an ambulatory patient brings in the results of the following tests with a referral, how recent should the last results be for you to determine that there would be no need for retesting?
Q6-2. In case of “laboratory results”
Q6-3. In case of “radiology results”
Q6-4. Please provide examples of the laboratory tests or radiology tests that are different from general cases and the reasons for the differences in your answers.
If the sharing of patient data among medical facilities is further developed, it may become possible to view various data of the referred patient, including all past information recorded by the referring hospital.
Q7. Realistically, how much of the provided information would you be able to review? Please answer which information you would look through under the premise that you would do so within the time allowed in your routine medical practice and with the same number of patients that you currently see. (If you chose “Progress notes” in Q7)
Q7-1. How much of the “progress notes” would you review under the premise that you would do so within the time allowed in your routine medical practice and with the same number of patients that you currently see?
This is the end of the questionnaire. Thank you for your cooperation.
aSome answer choices are omitted here; Q4, Q8, and Q9 were excluded from the analysis.
Go to : 
References
1. Barrett B, Tyrer P, Tyrer H, Cooper S, Crawford MJ, Byford S. An examination of the factors that influence costs in medical patients with health anxiety. J Psychosom Res. 2012; 73(1):59–62. PMID: 22691561.

2. Bahous MC, Shadmi E. Health information exchange and information gaps in referrals to a pediatric emergency department. Int J Med Inform. 2016; 87:68–74. PMID: 26806713.
3. Johnson T, Owens L. Survey response rate reporting in the professional literature. In : Proceedings of 58th Annual Meeting of the American Association for Public Opinion Research; 2003 May 15-18; Nashville, TN.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download